All published articles of this journal are available on ScienceDirect.
The Role of Arthroscopic Partial Meniscectomy in the Management of Degenerative Meniscus Tears: A Review of the Recent Literature
Abstract
Background:
The use of arthroscopic partial meniscectomy for middle aged to older adults with knee pain is one of the most common surgical procedures with approximately 150,000 knee arthroscopies being carried out in the United Kingdom each year, and about five times that number in the United States. Despite this, the procedure remains controversial. The aim of this paper is to provide a comprehensive review of the role of arthroscopic meniscectomy in patients with degenerative meniscus tears and suggest recommendations for clinical practice.
Methods:
A thorough literature search was performed using available databases, including Pubmed, Medline, EMBASE and the Cochrane Library to cover important randomised control trials surrounding the use of arthroscopic partial meniscectomy.
Results:
The majority of randomised control trials suggest that arthroscopic partial meniscectomy is not superior to conservative measures such as exercise programmes. Furthermore, one randomised control trial found that arthroscopic partial meniscectomy was not even superior to sham surgery.
Conclusion:
There is significant overtreatment of knee pain with arthroscopic partial meniscectomy when alternative, less invasive and less expensive treatment options are equally effective. First-line treatment of degenerative meniscus tears should be non-operative therapy focused on analgesia and physical therapy to provide pain relief as well as improve mechanical function of the knee joint. Arthroscopic partial meniscectomy should be considered as a last resort when extensive exercise programmes and physiotherapy have been tried and failed.
INTRODUCTION
The menisci of the knee (medial and lateral) are wedge-shaped semilunar disks composed of fibrocartilage interposed between the tibia and the condyles of the femur [1]. They have an important role in load-bearing and shock absorption within the joint. They may also function as secondary stabilisers, have a proprioceptive role, and aid the lubrication and nutrition of the articular cartilage [2].
Meniscus tears are the most common injury of the knee [1]. They can be classified by their location and type. They may occur in acute knee injuries in younger patients, or as part of a degenerative process in older individuals. Acute meniscus tears typically occur when a person changes direction in a manner that involves rotating or twisting of the knee while the knee is flexed and the corresponding foot is planted. This commonly occurs in sports such as football, basketball and American football [3]. Older individuals can develop a degenerative meniscus tear with minimal or no trauma as the menisci become stiffer and less compliant with age [4].
The fundamental principle of meniscus surgery is to preserve as much ‘normal’ meniscus as possible [5]. Tears with a high probability of healing with surgical intervention are repaired (meniscus repair) but most tears are not repairable and partial meniscectomy is an alternative. The indications for performing a meniscus repair depend on a number of factors: location (peripheral tears heal better due to blood supply), morphology (shorter tears and vertical longitudinal tears are more amenable to repair vs. longer and degenerative horizontal tears) and chronicity (acute tears more amenable to repair) [6]. These conditions are rarely met in older patients, where degenerative meniscus tears are more common. Meniscus repair is thus performed almost exclusively in younger patients. Older patients are more likely to have degenerative tears that are not amenable to repair and therefore APM has been an inevitable treatment option [6].
The use of APM for middle aged to older adults with knee pain is one of the most common surgical procedures with approximately 150, 000 knee arthroscopies being carried out in the United Kingdom each year, and about five times that number in the United States [7, 8]. The number of knee arthroscopies performed in England on people aged ≥60 between 2000 and 2011 has risen substantially, from 185 procedures per 100 000 population to 267/100 000 [9]. In Denmark, the surgery rate doubled from 2000 to 2011, with 75% of patients aged more than 35 years [10]. The increases in arthroscopy rate in England are accounted by increases in meniscus resection, particularly between 2007 and 2010 in those aged 60-74 [9]. Indeed, APM has a role in patients with symptoms of mechanical locking. Nonetheless, the high rates of the procedure in people > 60 suggest that it is being used in other patient groups despite the fact that there is no evidence of a substantially increased prevalence of meniscus tears in this population [9].
REVIEWING THE LITERATURE
Observational studies, including longitudinal cohort studies, have suggested that APM is an effective treatment for meniscus tears [11-15]. However, a number of randomised control trials have been published since [16-21, 24]. The RCTs have predominantly focused on pain as the primary outcome of interest (see Table 1).
The first study to compare exercise alone to APM alone was a small pilot study by Østerås et al. [16]. They compared the effectiveness of medical exercise therapy (MET) versus arthroscopic surgery in patients with degenerative meniscus injury and knee pain. Nine patients were randomly assigned to MET (3 treatments a week for 3 months) and 8 patients were randomly assigned to arthroscopic meniscectomy with no structured conservative therapy after surgery. After 3 months, there were no statistical differences between the two groups regarding pain and function. Additionally, anxiety and depression were significantly reduced in the MET group compared with the patients receiving arthroscopic surgery [16]. Although this study demonstrated conservative therapy is equally effective as surgery with additional benefits on mental health, it’s very small sample size was a significant limitation.
About a decade ago, Herrlin and colleagues conducted an RCT comparing APM with exercise therapy [17, 18]. Ninety-six patients aged 45-64 with medial meniscus tears and osteoarthritis (OA) were followed for 5 years [17, 18]. Forty-seven patients were randomized to APM and exercise and 49 were randomized to exercise therapy alone. Twenty-seven % of patients managed by exercise therapy were eventually treated by APM. Although Intention to treat (ITT) analysis showed a greater difference on the pain outcome compared to baseline in favour of APM this was not statistically significant [17, 18]. This was the first RCT to compare exercise therapy with APM for degenerative meniscus tears with well standardized surgical and physical therapy protocols. However, the study had some limitations. The APM cohort had significantly poorer baseline characteristics leading to possible selection bias. Furthermore there was a low enrolment of eligible patients (55%) with high crossover rate of patients going from exercise therapy to APM (28%).
A multi-centred RCT by Katz et al. published in the New England Journal of Medicine also compared APM with physical therapy [19]. Subjects were symptomatic patients aged 45 years and over with a meniscus tear and evidence of OA (0-3 by Kellgren-Lawrence criteria). Of the 351 patients that were included in this trial, there were no significant differences in the magnitude of improvement in functional status and pain after 6 and 12 months between patients assigned to APM and postoperative physical therapy. This study had a strong design and large cohort size. It must be noted however that 30% of patients assigned to the physical-therapy group crossed over to surgery in the first 6 months [19]. The factors for this crossover were not clearly defined and may have skewed the results. Nonetheless, outcomes of the crossover patients at 12 months were similar to those patients who had surgery initially suggesting that non-operative treatment is a reasonable first line strategy.
Vermesan and colleagues compared arthroscopic debridement with intra-articular steroids in treating degenerative medial meniscus tears [20]. One-hundred and twenty patients with non-traumatic symptomatic knees with degenerative lesions of the medial compartment (cartilage and meniscus) on MRI were randomised to either intra-articular steroid injection or arthroscopic debridement. The arthroscopic group performed better in terms of the Oxford Knee Score at one month but the difference was small. Furthermore, this difference was not statistically or clinically significant at one year. The authors concluded that degenerative medial meniscus tears in the presence of OA can only marginally benefit from arthroscopic debridement over intraarticular steroid injections in the short term [20]. A major limitation to this study was that numerous factors were not taken into consideration such as the influence of physiotherapy and analgesia. Furthermore, there were limited outcomes measured and relatively short follow up time.
In the same year, Yim et al. [21] analysed 102 patients aged 43-62 years with degenerative horizontal tears of the posterior horn of the medial meniscus with OA (0-1 by Kellgren-Lawrence criteria) for two years. Fifty-two patients were treated with strengthening exercises alone and 50 patients with APM and strengthening exercises. There were no significant differences between arthroscopic meniscectomy and muscle strengthening exercises in terms of knee pain relief, improved knee function, or increased satisfaction in patients after a 2 year follow up [21]. Although this study had flaws including its low enrolment rate (66.7%) and relatively small sample size, it had low losses to follow-up rate and a low crossover rate (only one patients assigned to non-operative management crossed over to surgery) compared to the previous studies discussed above.
The first multi-centred randomised sham-controlled trial was conducted by Sihvonen and colleagues assessing the role of APM specifically [22]. This study had superiority in terms of its rigorous double-blinded, sham-controlled design, low losses to follow-up and low crossover rates with high enrolment rate. A total of 146 patients with degenerative medial meniscus tear underwent randomisation; 70 were assigned to undergo APM, and 76 were assigned to undergo sham surgery. This landmark study showed that although both groups had significant improvements in primary outcomes (knee pain after exercise and Lysholm knee score at 12 months), APM did not have a greater improvement than those assigned to sham surgery. Furthermore, no significant between-group differences were found in any of the secondary outcomes (need for subsequent knee surgery or frequency of serious adverse events). The authors concluded that the results argue against the current practice of performing APM in patients with degenerative meniscus tears [22].
There is opposing evidence by Gauffin and colleagues in favour of APM. One-hundred and fifty patients aged 45 to 64 were randomised to either physiotherapy or physiotherapy plus knee arthroscopy for resection of any significant meniscus injuries [23]. Of the 75 patients who initially were randomised to surgery, 66 had actually had surgery (56 had APM). Of the 75 patients who initially were randomised to non-surgical treatment, 16 crossed over and had surgery (11 had APM). Although both treatment groups improved significantly in pain score at 12-month follow-up (P < 0.001), the change in the pain score was significantly larger in the surgery group than the non-surgery group [23]. This was the first RCT to report superiority of APM compared to physical therapy, by both ITT and as-treated analyses. Strengths of this study included a high enrolment rate and long follow up period (up to 3 years). This was compounded however by a poorer baseline KOOS scores in the surgery group, heterogeneity in the surgeries performed, poor compliance to physiotherapy as well as high losses to follow-up rate and crossover (21%).
The above trials were summarised in two systematic reviews and meta-analyses [24, 25]. Khan et al. found that interventions including arthroscopy showed a small benefit for pain but this small effect was of short duration and absent one year after surgery. Furthermore, 9 studies reported significant harm. The number of adverse events per 1000 procedures was 5.68 for VTE, 2.11 for infection and 0.96 from any cause death [24]. Similarly another systematic review and meta-analysis based on 7 RCTs (n = 805 patients) found that there was no benefit to arthroscopic meniscus debridement compared to non-operative treatment. The authors concluded that a trial of non-operative management should be the first-line treatment for such patients [25]. A recent systematic review by Lampton et al. which included five RCTs described above and one prospective cohort study found that there was particular benefit from APM when mild OA existed but conservative therapy should be considered especially in patients with moderate OA [26].
Following on from this, a recent rigorous RCT has provided further convincing evidence to support conservative therapy over APM [27]. Kise et al. compared exercise therapy against APM alone for degenerative meniscus tears in middle aged patients (without radiological signs of OA). In this study, degenerative meniscus tears were verified by magnetic resonance imaging (MRI). One-hundred and forty adults (mean age 49.5 years) with degenerative medial meniscus tear were randomized to a 12 week supervised exercise therapy or APM alone. Primary endpoints were patient reported knee function at two years and thigh muscle strength at three months. The authors found no between group differences in patient reported knee function at the two year follow-up, but greater muscle strength in the exercise group at three months [27]. The strengths of this study included the high rate of participation in the two year follow-up and blinding of the assessors. It also provided further information compared to previous studies by assessing a younger, more active population with a lower body mass index as well as assessing thigh muscle strength as an additional outcome. Limitations of comparing surgical with non-surgical treatment included crossover from the non-surgical group to the surgical group (19%) which was not clearly defined. It should also be noted that participants in the meniscectomy group had better KOOS scores at baseline, were slightly younger, had a lower body mass index, and reported knee pain for a shorter time than the exercise therapy group. Their better baseline status may have provided an advantage in participants in the meniscectomy group, and, if anything, one would expect better results in this group which was not the case.
| Study | Year | Country | N0 of patients | Mean age | Associated osteoarthritis | Conservative group | Surgical group | Main outcomes | Cross over |
|---|---|---|---|---|---|---|---|---|---|
| Herrlin et al. [17, 18] | 2007, 2013 | Sweden | 90 | 55 | Ahlback grades 0-1 | Standardized exercise program for 8 wk | Exercise + APM |
KOOS, Lysholm Knee Scoring Scale, Tegner Activity Scale, VAS scores | 28% |
| Østerås et al. [16] | 2012 | Norway | 17 | 50 | Kellgren-Lawrence grades 0-2 | Exercise programme 3x week for 3 mo | APM | KOOS,, VAS, HAD scores, quadriceps muscle strength at 3 mo | None |
| Katz et al. [19] | 2013 | United States | 351 | 58 | Kellgren-Lawrence grades 0-3 | Individualized physical therapy with progressive home exercise | Exercise + APM |
WOMAC-pf, KOOS pain scale, SF-36 physical activity scores | 30% |
| Sihvonen et al. [22] | 2013 | Finland | 146 | 52 | Kellgren-Lawrence grades 0-1 | Sham surgical procedure | APM | Lysholm Knee Scoring Scale, WOMET, VAS, 15D, patient satisfaction scores | None |
| Yim et al. [21] | 2013 | South Korea | 102 | 56 | Kellgren-Lawrence grades 0-1 | NSAIDs + 3 wk supervised physical exercise followed by 8 wk home exercise program | APM + strengthening exercises | Lysholm Knee Scoring Scale, VAS, patient satisfaction, Tegner Activity | 2% |
| Vermesan et al. [20] | 2013 | Romania | 120 | 58 | Kellgren-Lawrence grades 0-1 | Intra-articular steroid injection | APM | Oxford knee score at 1 mo and one year | None |
| Gauffin et al. [23] | 2014 | Sweden | 150 | 54 | Kellgren-Lawrence grades 0-2 | Individual exercise programme or home-based exercise programme for 3 mo | Exercise + APM |
KOOS, EQ5D, the PAS, and the symptom satisfaction scale | 21% |
| Kise et al. [27] | 2016 | Norway | 140 | 50 | Kellgren-Lawrence grades 0-2. | Progressive neuromuscular and strength exercises over 12 weeks, performed 2-3 x each week (24-36 sessions) | APM | KOOS, SF-36, the one leg hop test for distance, the 6 m timed hop test, and the knee bends test | 19% |
DISCUSSION
Based on successive reproducible data from a diverse number of RCTs, there seems to be a strong argument that there is significant overtreatment of knee pain with APM when alternative, less invasive treatments are available.
Following on from studies discussed above, there has been a significant response from orthopaedic surgeons questioning the validity and generalisability of these studies. Many orthopaedic surgeons have argued that different results may be seen if procedures were analysed in patients reflective of actual clinical practice in the settings in which APM is actually delivered [28]. Some surgeons including the editors of the journal Arthroscopy have even gone on to say that “the New England Journal of Medicine are biased against arthroscopic knee surgery” [29]. Indeed there are limitations to the studies highlighted above. Moreover, the identification of candidates for arthroscopic surgery is not straight forward and the long-term outcome of patients with meniscus tears varies according to the type of tear and the type of patient. Certainly it has been demonstrated from previous studies that some patients may do well with meniscectomies. For example, patients who sustain a traumatic cartilage tear that results in mechanical symptoms (catching or locking) may benefit from arthroscopy [30, 31]. Furthermore, it can be argued that a subset of patients with degenerative tears, initially managed non-operatively, may have recurring symptoms over a longer period, as seen in the crossover trials (discussed above) of APM in other groups. Nevertheless, on the whole there is vigorous and high quality evidence against the use of knee arthroscopy for degenerative meniscus tears which may be ignored by surgeons due to strongly held beliefs or deep-rooted attitudes towards such procedures.
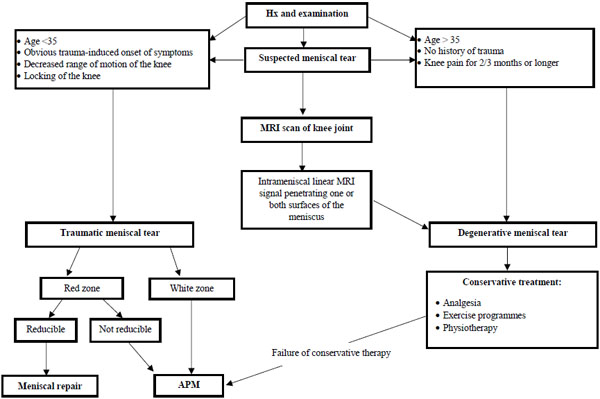
Those patients that generally do well are young patients with isolated tears [30, 31]. According to a retrospective review of 362 medial and 109 lateral isolated arthroscopic meniscectomies, factors associated with a favourable prognosis included those that were <35, a vertical tear, no cartilage damage and an intact meniscus rim upon completion of the procedure [30]. It is important to remember that Orthopaedic surgeons used to treat young people presenting after an injury with a “locked knee” (an inability to fully extend the painful knee because of a meniscus tear lodged between the articular surfaces) by trimming the torn meniscus in open surgery. With no support aside from biological rationale, the indication stemmed from locked knees in young patients to all patients of all ages with knee pain and meniscus tears of any sort [27]. Indeed, a large proportion of middle aged and elderly patients are found to have incidental meniscus tears [32] and this may be the first sign of OA [32-34]. Therefore, the finding of a meniscus tear on MRI in a patient without clinical symptoms should not warrant arthroscopy. Having said that it is not always straightforward to differentiate between traumatic meniscus tears and degenerative meniscus tears but there are several factors that should be taken into consideration when making a distinction between the two (see Table 2).
Although APM has consistently showed improvements compared to baseline, conservative therapy is equally effective and it also has the major advantage of being safer. Indeed the risks associated with knee arthroscopy are low yet present and include VTE, infection and death [24]. Furthermore, one must not forget the functions of the menisci - meniscectomy may lead to further destruction of cartilage and to OA of the knee joint. Degenerative changes have been found to be directly proportional to the amount of meniscus removed [2]. Even partial meniscectomy results in higher than normal stress on the underlying articular cartilage [35-38]. A recent study has even demonstrated that partial meniscectomy is strongly associated with incident OA within 1 year and worsening cartilage damage in the following year [39].
APM is not only potentially harmful for patients, but conservative therapy is also much more cost effective. A cost effective analysis of arthroscopic surgery compared with non-operative management for OA of the knee was performed recently by Marsh et al. [40]. They investigated 168 patients receiving arthroscopic debridement and partial resection of degenerative knee tissues plus optimised non-operative therapy vs. optimised non-operative therapy only. When using Western Ontario McMaster Osteoarthritis Index (WOMAC) and quality-adjusted life years (QALYs) as effectiveness outcomes, the sensitivity analysis suggested that resection of degenerative meniscus tears in addition to non-operative treatments for knee OA is not an economically attractive treatment option compared with non-operative treatment only, regardless of willingness-to-pay value [40]. Another cost effective analysis comparing meniscus repair vs. partial meniscectomy found that although meniscus repair was associated with an increased failure rate, there were meaningful reductions in OA and total knee replacement incidence compared to partial meniscectomies [41]. Moreover, they projected that payers could save approximately $43 million annually if 10% of current meniscectomies could be performed as meniscus repairs [41].
| Traumatic meniscus tears | Degenerative meniscus tears |
|---|---|
| Age <35 | Age > 35 |
| Obvious trauma-induced onset of symptoms | No history of trauma (sudden onset of knee pain resulting from a single physical impact event) |
| Decreased range of motion of the knee | Knee pain for 2/3 months or longer |
| Locking of the knee | Degenerative meniscus tear characteristic on MRI scan (defined as intrameniscus linear MRI signal penetrating one or both surfaces of the meniscus) |
CONCLUSION
The role of APM in the management of degenerative meniscus tears remains controversial. From our review, most RCTs have suggested that there is significant overtreatment of knee pain with APM when alternative, less invasive and less expensive treatment options are equally effective. APM should therefore be reserved for younger patients with acute traumatic tears and/or patients with a locked knee when meniscus repair is not possible due to reasons outlined in Fig. (1). First-line treatment of degenerative meniscus tears should be non-operative therapy focused on analgesia and physical therapy to provide pain relief as well as improve mechanical function of the knee joint. APM should be considered as the last resort when extensive exercise programmes and physiotherapy have been tried and failed (see Fig. 1). We feel that national and international guidelines should be updated to reflect this notion.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


