All published articles of this journal are available on ScienceDirect.
Metacarpophalangeal Joint Arthrodesis of the Thumb – Minimum of Eight Months Follow-up
Abstract
Background:
Disorders of the thumb metacarpophalangeal (MCP) joint can lead to significant loss of function and pain. Thumb MCP arthrodesis following traumatic injuries is inadequately described and recent studies have questioned the outcome of this treatment.
Purpose:
The purpose of this study was to report outcome and disability following thumb MCP joint arthrodesis in the treatment of chronic instability after traumatic injuries.
Methods:
A retrospective review of 26 patients operated on with MCP joint arthrodesis, median follow-up 42 months (8-104months). Subjective outcome was assessed using the disabilities of the Arm, Shoulder, and Hand-questionnaire (DASH). In addition, patient satisfaction, pain, stiffness, and impairment of activities of daily living were assessed on a Visual Analogue Scale (VAS) followed by a question stating whether they would undergo the same procedure again.
Results:
Two patients (7.7%) needed re-operation due to nonunion. Four patients (15.4%) needed hardware removal. Median DASH-score was 18 (25-75% range 6-47), with lower DASH scores being better. Scores were significantly worse in gender and age matched individuals (p<0.05). Median VAS for pain was 3.7 (range 0-8). More than 50% of patients reported mild, moderate or severe pain, but all patients reported that they were willing to undergo the same procedure again.
Conclusion:
Our data suggest, that patients with post-traumatic thumb injuries managed with thumb MCP joint arthrodesis perform worse than gender and age matched individuals. Many lived with pain, but all reported that they were willing to undergo the same procedure again. We suggest that the disability scale by the National Board of Industrial Injuries should be reconsidered for patients operated on with thumb MCP arthrodesis.
INTRODUCTION
Disorders of the thumb metacarpophalangeal (MCP) joint can lead to significant loss of function, deformity, and pain. Surgical treatment of these disorders ranges from arthroscopic synovectomy to ligament reconstruction or arthrodesis. Arthrodesis of the thumb MCP joint has been considered the standard treatment of many disorders ranging from rheumatoid arthritis, osteoarthritis, post-traumatic arthritis and chronic joint instability [1-3]. Multiple techniques have been used including K-wire fixation, interosseous wiring, tension-band wiring, plating, and lag screw technique to obtain osseous fusion [4-8]. However, a recent study has questioned the patients’ satisfaction and subjective outcome following thumb MCP joint arthrodesis [9].
The National Board of Industrial Injuries (NBII) in Denmark published the first national permanent injury rating list in 1979. Since then 6 editions have followed. At present time the disability following arthrodesis of the thumb MCP joint is categorized as <5% and not economically or otherwise compensated for while instability of the MCP joint, for example, equals 5% disability [10].
The aim of this study was to assess the disability following thumb MCP joint arthrodesis by evaluating outcome following arthrodesis due to traumatic injuries with chronic instability and pain.
MATERIALS AND METHODS
Inclusion and Exclusion Criteria
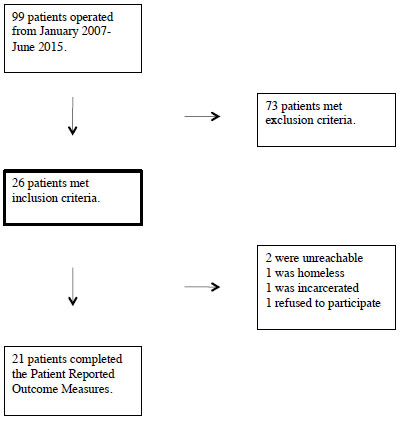
A retrospective review of 99 patients operated between January 2007 and June 2015 with thumb MCP joint arthrodesis was performed. 26 of 99 patients met the inclusion criteria of post-traumatic joint instability and pain. 73 patients were excluded due to pre-operative diagnosis of rheumatoid arthritis, multi-joint involvement or other non-traumatic conditions. There were no cases of bilateral involvement (Fig. 1).
Demographics
26 patients met inclusion criteria. The median follow up was 42 months (range 8-104 months). There were 11 men and 15 women. The median age at the time of the follow-up was 55 years (range 31-74 years). The dominant hand was involved in 9 cases (47.9%, n=19). The pre-operative diagnosis was post-traumatic chronic joint instability and pain.
Reference material was found in a Norwegian study of normative values of the DASH-score in Norway. 2800 DASH questionnaires were sent to random individuals in such a way that they included 200 men and 200 women in each age decade from 20 to 80 years and older [11]. Each of our patients and the respective DASH-value in this study was matched with the median of the normative material for gender and age decade. As scores were not normally distributed, the median was used instead of the mean.
Patient Reported Outcome Measures (PROM)
The Danish DASH-questionnaire [12, 13] was completed. It includes 30 questions concerning disability and symptoms and an optional section regarding music/sport. The DASH questionnaire is designed to evaluate physical function and symptoms in patients with musculoskeletal disorders of the upper limb. The scores range from 0 to 100, where 0 is no disability and 100 is extreme disability.
The patients were also asked to rate their overall satisfaction, pain, stiffness, and impairment of activities of daily living (ADL) on a Visual Analogue Scale (VAS) [14]. Together with an additional question if they would agree to undergo the same procedure again [9].
PROMs were used as subjective outcome measures of the patients’ quality of life following thumb MCP joint arthrodesis.
Statistical Analyses
PROMs were statistically tested with a significance level of 5%. A chi-square goodness of fit test was performed revealing that data were not normally distributed (p<0.05%). Therefore, non-parametric statistics was applied. A Mann-Whitney U test was performed with significance value of 0.05 (5%).
The National Committee on Health Research approved the study and all patients signed consent forms.
RESULTS
Twenty-four of 26 patients (92.3%) were operated with plate fixation technique. Two patients (7.7%) were operated with Kirschner-wire fixation. There were no cases of postoperative infection. Two patients (7.7%) needed repeat surgery for the lack of optimal positioning and continuous instability and pain. After re-operating these patients they were both satisfied and bony union was confirmed radiographically. Four patients (15.4%) needed hardware removal. The operating surgeon evaluated their patients with plain radiograph of the hand 5 weeks post-operatively. There were no non-unions at the end of treatment.
Patient Reported Outcome Measures
For the analysis of patient outcome, 21 out of 26 patients responded. Five patients did not respond, 3 of whom were lacking contact information, 1 had a history of alcohol abuse and was homeless, 1 was imprisoned, and 1 refused to participate for unknown reasons. DASH scores ranged from 3 to 60 points (Table 1). The median DASH-score was 18 (interquartile range, IQR 6-47). One of the patients who did not respond was one of the two cases who needed re-operation. The second patient who needed re-operation scored below the median DASH score. Twelve patients (57%) answered that they had moderate to severe difficulty with the ability to open a new jar, write, turn a key, prepare a meal, or make a bed. 6 patients reported mild pain, 5 patients reported moderate pain and 3 patients severe pain in their arm, shoulder or hand at follow-up. The Mann-Whitney U test showed DASH scores for the included patients were significantly higher than the age and gender matched controls indicating increased disability as compared to the control group (p<0.05).
Median VAS scores for impairment of activities of daily living, pain, satisfaction, and mobility of the thumb were 3.2, 3.7, 7.8, and 5.1 respectively (Tabel 1). When asked whether the patient would undergo the same operation again knowing the end result, nineteen of 21 agreed, two did not respond. No patients regretted the operation.
DISCUSSION
Previously studies have suggested that thumb MCP joint arthrodesis is safe and provides good pain relief and functional results with few complications [1, 5, 6]. Several techniques have been suggested including intermedullary interlocking devices with a two component compression screw system, K-wire fixations with one or two K-wires for optimal positioning and stability, plate fixation with cup and cone technique and multiple screws, and cannulated compression screws. Regardless of the techniques good patient satisfaction and good results with few complications and infections have been reported [4, 5, 8, 15]. This is presumably the reason that the disability following thumb MCP arthrodesis is categorized <5% by the NBII.
Most studies, however, focus mainly on bony union, surgical complications, and infections as parameters of success.
A recent study by Røkkum et al. has questioned the patient-satisfaction following thumb MCP joint arthrodesis for post-traumatic conditions [9]. They reported that thirty-seven of 46 patients (80%) experienced difficulties with one or more specific activities such as slicing bread, using scissors, opening jars, handling small or heavy objects, writing, using a keyboard, or writing messages on a mobile phone [9].
| Median | Range | Interquartile range | Intepretation | |
|---|---|---|---|---|
| DASH score (n=21) | 18 | 3-60 | 7-47 | 0-100 least is best |
| VAS, impairment of ADL (n=19) | 3.2 | 0-8 | 1-5 | 0-10 least is best |
| VAS, pain (n=19) | 3.7 | 0-8 | 1-5 | 0-10 least is best |
| VAS, satisfaction (n=19) | 7.8 | 2-10 | 7-10 | 0-10 highest is best |
| VAS, mobility of thumb (n=19) | 5.1 | 0-10 | 4-6 | 0-10 highest is best |
We report DASH values that are statistically higher (worse) than age and gender matched individuals with a significance level of 5%. These results suggest that our patients are worse off than their gender and aged matched controls. Our patients also reported mild, moderate or severe pain at follow-up in more than 50% of cases. These findings suggest that patients operated with thumb MCP arthrodesis following traumatic injury are living with some degree of disability compared to healthy individuals.
Despite these findings, all of our patients reported that they were willing to undergo the procedure again suggesting that no one regretted the operation. This indicates that patients are in fact happy about their choice of treatment. This also suggests that pre-operative conditions have been even more disabling than the post-operative result.
The NBII in Denmark categorizes thumb MCP injury and following arthrodesis as a permanent disability of less than 5% [10]. A clear description of what exactly a 5% permanent injury equals is not available as the permanent injury-rating list is historically composed from fractions of disability and are composed of subjective opinions of the disability following an injury. A cut-off value on a DASH score is not available, as the disability is not categorized from objective results of scientific studies but rather subjectively from expert opinions. As such it is not directly possible to address the question whether or not this categorization is fair. However, it is clear from our results, that this group of patients perform significantly worse than the general public [11] and that they do have some degree of disability. Reconsideration by the NBII of the categorization of patients operated with thumb MCP joint arthrodesis is warranted.
The external validity of this study is supported by a previous validation study of the DASH questionnaire in a Danish population by Herup, A. et al. [16]. They conclude that the reproducibility of the DASH questionnaire is good and that DASH scoring is stable and reliable in a Danish patient population.
Limitations of this study include those inherent to a retrospective study and the relatively limited patient population. The pre-operative inclusion of only post-traumatic cases sets a limitation for the number of patients included. Even at a high-volume facility of hand surgery, this particular case is rather uncommon. Future assessments of pre-operative scores in a larger patient population may provide more safe estimates.
CONCLUSION
We report that patients with post-traumatic thumb injuries managed with thumb MCP joint arthrodesis score significantly worse than gender and age matched individuals. More than 50% of cases report mild, moderate or severe pain, but all patients reported that they were willing to undergo the same procedure again. Two patients needed repeat surgery for lack of optimal positioning and continuous instability and pain. Four patients needed hardware removal. There were no non-unions at the end of follow-up. Reconsideration by the NBII of the categorization of patients operated with thumb MCP joint arthrodesis is warranted.
LIST OF ABBREVIATIONS
| ADL | = Activities of Daily Living |
| DASH | = Disabilities of the Arm, Shoulder, and Hand-questionnaire |
| MCP | = Metacarpophalangeal |
| NBII | = The National Board of Industrial Injuries |
| VAS | = Visual Analogue Scale |
| PROM | = Patient Reported Outcome Measures |
INSTITUTIONAL REVIEW BOARD STATEMENT
The study was reviewed and approved by the Committees on Health Research Ethics in the Capital Region of Denmark.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


