All published articles of this journal are available on ScienceDirect.
Comprehensive Operative Note Templates for Primary and Revision Total Hip and Knee Arthroplasty
Abstract
Background:
Adequate preoperative planning is the first and most crucial step in the successful completion of a revision total joint arthroplasty. The purpose of this study was to evaluate the availability, adequacy and accuracy of operative notes of primary surgeries in patients requiring subsequent revision and to construct comprehensive templates of minimum necessary information required in the operative notes to further simplify re-operations, if they should become necessary.
Methods:
The operative notes of 144 patients (80 revision THA’s and 64 revision TKA’s) who underwent revision total joint arthroplasty at Stanford Hospital and Clinics in the year 2013 were reviewed. We assessed the availability of operative notes and implant stickers prior to revision total joint arthroplasty. The availability of implant details within the operative notes was assessed against the available surgical stickers for adequacy and accuracy. Statistical comparisons were made using the Fischer-exact test and a P-value of less than 0.05 was considered statistically significant.
Results:
The primary operative note was available in 68 of 144 revisions (47%), 39 of 80 revision THAs (49%) and 29 of 66 revision TKAs (44%, p = 0.619). Primary implant stickers were available in 46 of 144 revisions (32%), 26 of 80 revision THAs (32%) and 20 of 66 revision TKAs (30%, p = 0.859). Utilizing the operative notes and implant stickers combined identified accurate primary implant details in only 40 of the 80 revision THAs (50%) and 34 of all 66 revision TKAs (52%, p = 0.870).
Conclusion:
Operative notes are often unavailable or fail to provide the necessary information required which makes planning and execution of revision hip and knee athroplasty difficult. This emphasizes the need for enhancing the quality of operative notes and records of patient information. Based on this information, we provide comprehensive operative note templates for primary and revision total hip and knee arthroplasty.
INTRODUCTION
The importance of operative notes and operative stickers of implants used for primary total joint arthroplasty surgery is undeniable for the planning of revision total joint arthroplasty. Adequate preoperative planning is the first and most crucial step in the successful completion of a revision total joint arthoplasty [1]. A detailed knowledge of implants used in the primary operation makes it possible to make appropriate arrangements for the necessary extraction tools, components and instrumentation to accomplish the revision surgery. This prevents intra-operative surprises and reduces stress on the surgical team, decreases operative time, and helps optimize the outcome for the patients by ensuring that the preoperative plan is carried out smoothly with the necessary instrumentation and prosthesis. Detailed and specific information of the primary procedure would make it easier to achieve the goals set for the revision surgery. Furthermore, accurate and detailed documentation of the surgical procedure forms an essential part of good medical practice [2-4]. The purpose of this study was to evaluate the availability, adequacy and accuracy of operative notes of primary hip and knee arthroplasty in patients requiring subsequent revision, and referred to our institution. Based on the above information, a second goal was to construct comprehensive operative note templates of minimum necessary information required in the operative notes of patients undergoing primary and revision hip and knee arthroplasty to further simplify re-operations, if they become necessary.
MATERIALS AND METHODS
This study was approved by our institutional ethics review board. The operative notes of 144 patients who underwent revision total joint arthroplasty at Stanford Hospital and Clinics in the year 2013 were reviewed. Three experienced fellowship trained arthroplasty surgeons at a single institution performed all surgeries. 80 patients (56%, 37 males and 43 females) underwent revision total hip arthroplasty (THA). Of the 80 revision THAs, 58% were performed for implant wear (with or without osteolysis), 10% for infection, 8% for instability, 11% for adverse local tissue reaction, 8% for periprosthetic fracture, 1% for implant fracture, 5% for and miscellaneous (e.g., pain, psoas tendonitis). The entire socket was changed in 40% of cases, both acetabular and femoral components were replaced in 37% cases, femoral component alone in 11% cases, head and liner alone in 7% cases, head alone in 3% cases, and liner alone in 2% cases. 66 patients (44%, 33 males and 33 females) underwent revision TKA. Of the 66 revision TKAs, 35% were performed for aseptic loosening with or without polyethylene wear, 24% for infection, 15% for instability, 9% for patellofemoral maltracking, 6% for stiffness, 3% for periprosthetic fracture, and 8% for other causes (e.g., pain, malrotation). Both femoral and tibial components were revised in 55% cases, femoral component alone and polyethylene insert in 11% cases, tibial component alone and polyethylene insert in 11% cases, and liner alone in 18% cases. Patellar component was revised in 5% cases.
We assessed the availability of operative notes and implant stickers prior to revision total joint arthroplasty. The availability of implant details within the operative notes was assessed against the available surgical stickers for adequacy and accuracy. Total hip implant details were considered adequate when the sizes of acetabular shell, acetabular screws (if used), acetabular liner, femoral head component and femoral stem were mentioned along with the type of bearing surface and the name of the manufacturing company. Total knee implant details were considered adequate when the size of femoral component, size of the tibial component, thickness of the polyethylene insert, size of the patellar component, bearing constraint, and the name of the manufacturer were specified. Implant details in the operative note matching the surgical stickers were considered accurate.
We also assessed the availability of procedure related information including surgical approach as well as quality of bone and soft tissues. Total knee procedural details were assessed, including the angle selected for distal femoral resection, angle of posterior tibial slope, the degree of gap balancing, stability in flexion and extension, and adequacy of patella-femoral tracking. Total hip procedural details were assessed, including, cup abduction and anteversion, femoral anteversion, the degree of stability achieved, adequacy of limb length discrepancy, and offset correction achieved
Statistics
All categorical variables are reported as the amount and percentage. Statistical comparisons were made using the Fischer-exact test and a p-value of less than 0.05 was considered statistically significant.
RESULTS
Operative notes and implant stickers were difficult to obtain prior to revision total joint arthroplasty (Table 1). The primary operative note was available in 68 of 144 revisions (47%), 39 of 80 revision THAs (49%) and 29 of 66 revision TKAs (44%, p = 0.619). Primary implant stickers were available in 46 of 144 revisions (32%), 26 of 80 revision THAs (32%) and 20 of 66 revision TKAs (30%, p = 0.859). When primary implant stickers were unavailable for reference, operative notes were available 33 of 144 revisions (23%), 17 of 54 remaining revision THAs (32%) and 16 of the 46 remaining revision TKAs (35%, p = 0.832).
| Operative Note | Implant Sticker | At Revision THA | At Revision TKA | p-value |
|---|---|---|---|---|
| Available | --- | 39/80 (49%) | 29/66 (44%) | 0.619 |
| --- | Available | 26/80 (32%) | 20/66 (30%) | 0.859 |
| --- | Unavailable | 54/80 (67%) | 46/66 (70%) | 0.859 |
| Available | Unavailable | 17/54 (31%) | 16/46 (35%) | 0.832 |
Specific implant information was in general difficult to obtain prior to revision total joint arthroplasty (Table 2). Implant details (For hips: size of acetabular shell, number and size of acetabular screws (if used), size of acetabular liner, size of femoral head component and femoral stem, type of bearing surface, and the name of the manufacturer and for knees size of femoral component, size of the tibial component, thickness of the polyethylene insert, size of the patellar component, bearing constraint, or the name of the manufacturer) were mentioned in 31 of the available 39 primary operative notes prior to revision THA (79%) and all 29 available primary operative notes prior to revision TKA (100%, p = 0.017). Complete and accurate implant details were reported in 14 of the available 39 primary operative notes prior to revision THA (36%) and 26 of the available 29 primary operative notes prior to revision TKA (90%, p < 0.001). Incomplete implant details were mentioned in 15 of the available 39 primary operative notes prior to revision THA (38%) and 2 of the available 29 primary operative notes prior to revision TKA (7%, p = 0.001). Inaccurate or mismatched implant details were mentioned in 2 of the available 39 primary operative notes prior to revision THA (5%) and 1 of the available 29 primary operative notes prior to revision TKA (1%, p = 1.00). Utilizing the operative notes and implant stickers combined identified accurate primary implant details in only 40 of the 80 revision THAs (50%) and 34 of all 66 revision TKAs (52%, p = 0.870).
| Operative Note | Implant Sticker | At Revision THA | At Revision TKA | p-value |
|---|---|---|---|---|
| Mentioned | --- | 31/39 (79%) | 29/29 (100%) | 0.017* |
| Accurate | --- | 14/31 (45%) | 26/29 (90%) | <0.001* |
| Incomplete | --- | 15/31 (48%) | 2/29 (7%) | 0.001* |
| Inaccurate | --- | 2/31 (7%) | 1/29 (3%) | 1.00 |
The description of surgical technique available in operative notes prior to revision total joint arthroplasty was highly variable with no obvious standards for reporting (Tables 3 and 4).
| Information | At Revision THA |
|---|---|
| Surgical Approach | 26/39 (67%) |
| Bone or Soft Tissue Quality | 15/39 (39%) |
| Cup Abduction and Anteversion Angle | 18/39 (46%) |
| Stem Anteversion Angle | 21/39 (54%) |
| Degree of Stability Achieved | 14/39 (36%) |
| Degree of correction of Limb Length and offset | 11/39 (28%) |
| Information | At Revision TKA |
|---|---|
| Surgical Approach | 17/29 (59%) |
| Bone or Soft Tissue Quality | 5/29 (17%) |
| Distal Femoral Resection Angle | 13/29 (45%) |
| Posterior Slope of the Tibia | 2/29 (7%) |
| Releases in Extension/Flexion | 15/29 (52%) |
| Stability in Extension/Flexion | 14/29 (48%) |
| Overall Alignment | 14/29 (48%) |
| Patella Tracking | 14/29 (48%) |
DISCUSSION
Comprehensive and well documented operative notes are crucial for delivery of quality care [5]. Operative notes not only serve as vital means of communication between surgeons, but are the only comprehensive legal record of an operation [2-5]. Strategies to improve the quality of operative notes include providing a proforma or an aide-memoire both of which have proven benefits in a number of specialities [6, 7]. A study by Al Hussainy et al.. demonstrated that operative templates help to produce more comprehensive operative notes [2].
This study demonstrates that primary operative notes are often inadequate and fail to provide the necessary information required for the planning of revision total joint arthroplasty. The primary operative note and implant stickers were available in only 47% and 32% cases respectively prior to revision total joint arthroplasty. This may be due to poor record keeping and the lack of access to electronic medical record systems. In cases with an available operative note, essential implant related information was available in only 50% cases prior to revision total joint arthroplasty. This indicates that vital data regarding the primary operation and implants used was not adequately recorded in the operative note and hence was unavailable to the surgeon at the time of revision surgery. This highlights the need for improved database, electronic medical record systems and standardized operative note templates. Implementation of an electronic operation note system could help resolve this problem [8]. There is evidence of the superiority of computerized operation notes over hand written notes [9].
Operative notes often fail to provide complete details concerning surgical approach and implant details. This may create intra-operative confusion and anxiety, and increase operative time. Necessary component extraction tools and instruments, as well as compatible implants may be unavailable during the revision surgery.
Not uncommonly, revision THA may require complex procedures (e.g., acetabular reconstruction, extended troch-anteric osteotomy, excision of heterotopic ossification, etc.) or special implants (e.g., augments, long revision stem, constrained liner, etc.). The many challenges the surgeon faces could be reduced by adequate preoperative planning and by a careful review of the implant stickers and operative notes of the primary surgery. It is specifically important to identify the components to be removed. This is particularly true if any components are to be left in place. It is crucial that the characteristics and design of a retained component are compatible with those of the new components. A study by Jones et al. revealed that at least one component is retained in more than 50% of the patients undergoing revision THA [10]. In our study, one or more components was retained in 67% cases of revision THA. The most accurate surgical implant information is the manufacturer’s implant record as documented in the patient’s operative notes. The availability of this information becomes vital in such circumstances. If the acetabular component is well-fixed and well-aligned, it may be appropriate to exchange only the liner [11]. The appropriate modular liner should be available. If the locking mechanism is damaged, a polyethylene liner which can be cemented into a well fixed acetabular shell must be available [12]. It is also important to know if the stem used is modular or monoblock. If the stem is monoblock, the diameter of the head should be known, so that in the event that the stem is retained, the appropriate acetabular component liner can be made available. If the stem is modular, the appropriate modular heads and trial implants should be available in case the head is damaged. Many implant companies provide more than one modular head taper, so it is important to know which components are in place. An acetabular component may have screws, which may require a special screwdriver for removal. Well-fixed cementless fully porous femoral stems may require an extended trochanteric osteotomy, sectioning the stem, trephining, which must be done with numerous high-speed carbide cutting tools and trephines. Similarly, removal of cementless acetabular components may be facilitated by the use of sharp curved osteotomes, which match the diameter of the implant or similar devices such as the Explant system (Zimmer, Warsaw, IN, USA). Modular femoral components may require special tools to disassemble or retrieve their modular portions. Removal of well-fixed cemented stems can be facilitated by use of special equipment such as ultrasonic tools; this requires advance planning because most hospitals do not own such special equipment [1].
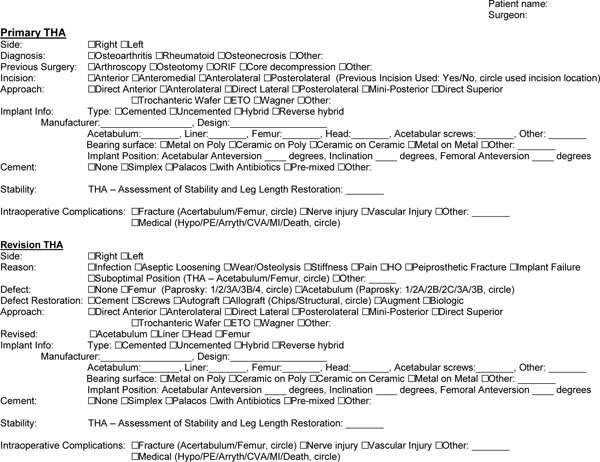
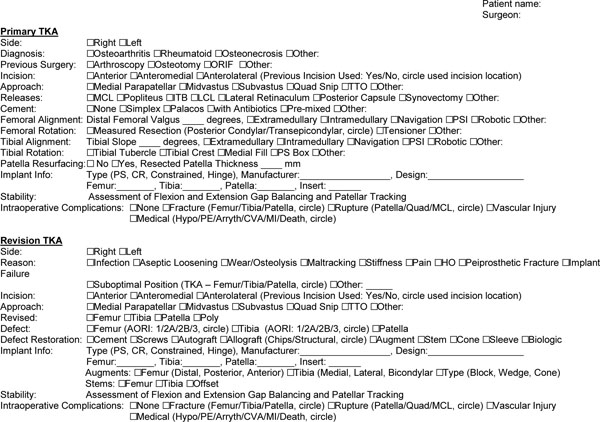
In revision TKA prosthetic components may also be required in addition to tools and instruments for component extraction. Component extraction requires in depth knowledge of the components implanted at primary TKA. The surgeon may have to contact the product representatives in order to obtain specific removal tools. The femoral component may often contain pegs that project into the distal femur and make access to this interface difficult. Offset osteotomes are useful in such cases. In cases where any component is to be left in place (partial joint revisions), it is crucial that the characteristics and design of a retained component are compatible with those of the new components. In our study, one or more components was retained in 50% cases of revision TKA. The most accurate surgical implant information is the manufacturer’s implant record as documented in the patient’s operative notes. The availability of this information becomes vital in such circumstances. The more that can be documented in the operative note the better subsequent patient care will be at the time of revision. A key to stable and successful revision TKA is good prosthetic alignment, reestablishing symmetry and equality of flexion and extension gaps [13]. The surgeon needs to determine what is deficient and what is necessary to reconstruct (bone and soft tissue deficits). Specific procedure related details from the previous surgeon’s operative notes (angle of distal femoral resection, degree of gap balancing in flexion and extension, angle of posterior tibial slope etc.) may help better plan the revision TKA surgery. Knowledge of the exposure used from the prior operative note can be important. If a previous lateral patellar arthrotomy was used at primary TKA, a subsequent medial parapatellar arthrotomy during a revision surgery increases the risk of avascular necrosis of the patella utilization of the previously chosen lateral arthrotomy might be considered [14]. Based on our findings, we provide comprehensive operative note templates containing minimum necessary information required in the operative notes of patients requiring primary and revision hip and knee arthroplasty surgery to facilitate later revision (Figs. 1 and 2). The templates are formulated with the aim to record most necessary operative-procedure and implant related information easily (tick-box format) in less than a couple of minutes. In addition to the referral patterns to tertiary medical centers, a key limitation of this study was that it was a single centre analysis. It is therefore imperative that collaboration between multiple secondary and tertiary care centers be fostered in order to facilitate better understanding of the lacunae in maintaining patient records and storage of patient related information.
CONCLUSION
Our study demonstrates that operative notes are often unavailable or fail to provide the necessary information required which makes planning and execution of revision hip and knee athroplasty difficult. This emphasizes the need for enhancing the quality of operative notes and records of patient information. Standardized operative note templates may help achieve this. These steps will ensure better preoperative planning, thereby reducing the operative time, potentially minimizing the risk of complications and improving the chances of success of a revision hip and knee arthroplasty surgery.


