All published articles of this journal are available on ScienceDirect.
Spontaneous Osteonecrosis of the Knee: A Retrospective Analysis by Using MRI and DEXA
Abstract
Objective:
Although there are many etiology and prediction for prognosis of spontaneous osteonecrosis of the knee (SONK) by using radiological examinations, these issue have not been clarified yet. Furthermore, most of the studies evaluated them by only radiological examination such as magnetic resonance imaging (MRI), bone mineral density (BMD) in dual-energy X-ray abosorptiometry (DEXA) or plain X-ray. Therefore, we focused our investigation on the measurements of the affected área in MRI and BMD in DEXA, and whether these results were conected with the cause and prognosis of SONK or not.
Method:
A consecutive case series of two groups composed of ten osteoporotic patients who were suffering from SONK was considered. Based on the severity or duration of pain, one group was treated with surgical procedure which was unicompartmental knee arthroplasty (UKA), the other received conservative treatment. Both groups underwent DEXA in their distal fêmur and próximal tíbia and all patients who took MRI measured the affected lesion in low and high intensity área on T2 weighted images. This data was analyzed from these areas and units.
Results:
Significant decrease in regional boné density of the affected femoral condyle compared to the unaffected side was observed. However, the boné mineral density in the affected side was similar in the non-operative and surgical group. The área of the lesion which showed in both low and high intensity indicated that the operation group was significantly larger than the conservative group on T2 weighted images.
Conclusion:
The cause and prognosis of SONK have a close relationship with the size of the affected lesion and decreased boné mineral density
INTRODUCTION
There are many multifactorial pathogeneses of spontaneous osteonecrosis of the knee (SONK) which were derived from oeteoporosis and the continuous cycle, the repeated impact and stress on the subcondral bone [1]. These may induce microfracture, thus leading to subcondral insufficiency fracture [2-7] the prognosis of which is thought to be dependent on the lesion as detected in the MRI [8-12], few studies with the combination of BMD and MRI have been reported [13]. In this article, we examined the cause and prognosis of our cases which were initially diagnosed as SONK by using MRI and DEXA. It appears that our cases are inconsistent with the hypothesis that low BMD is a risk factor for microfractures that might lead to permanent osteonecrosis. The size of its lesion on the MRI suggests whether they should undergo surgery or not.
PATIENTS AND METHODS
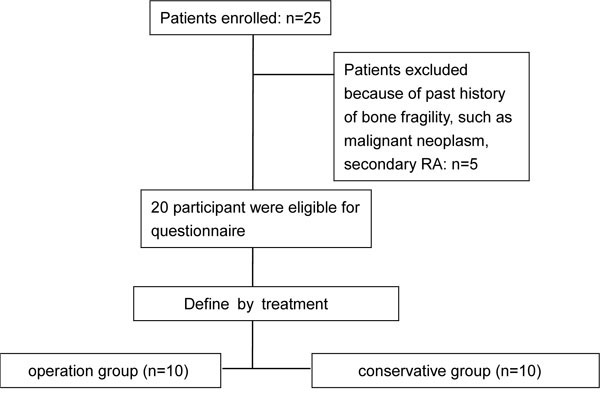
Between 2009 and 2013, we checked and treated twenty-five consecutive patients with SONK. We focused on healthy status, sex, age and duration of initial onset (Fig. 1), we excluded five patients who had past history of illness including Rheumatoid arthritis, diabetes, chronic kidney disease, alcoholics and steroid user which are the risk factor for fragility of bone. Those who fit our criteria were twenty patients, of which ten patients were given conservative treatment and others were treated with surgical procedures because of the severity of symptom or non-resolution of symptoms during 1 month bed rest for non-weight-bearing with NSAIDs and all of them had radiography, MRI of the knee and DEXA of the lumbar spine performed on them on the distal femur and proximal tibia 2 weeks after the onset of pain. This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its amendments. Data analyses were performed as follows.
Radiography
Plain X-rays were classified as the definition of Kellgren-Lawrence in every patients’ knee A-P view and measured femoro-tibial angle on standing position.
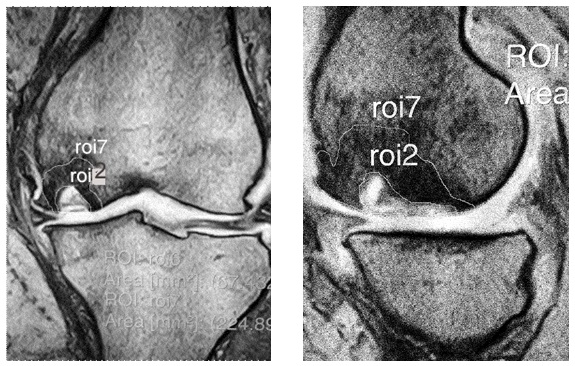
MRI
All patients’ affected lesions were measured in low and high intensity area on T2 weight image. This data was collected in coronal and sagittal view (Fig. 2).
BMD
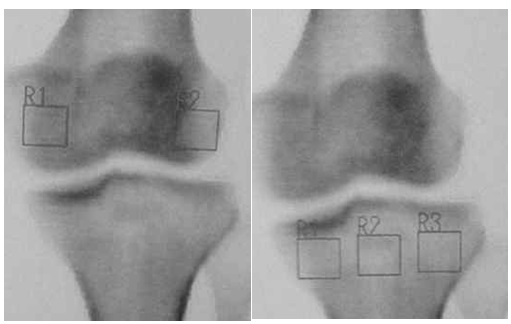
We measured both lumbar spine (L2-L4) and femoral neck using a dual energy X-ray absorptiometry (DXA, Hologic QDR Discovery W type; Toyo Medic., Tokyo, Japan).
Furthermore, the BMD measurement for the femoral condyles was performed. In the tibial condyles, 3 square regions of interest were marked with a square on the proximal tibia.
The medial tibial condyle BMDs in medial square region of interest and the lateral tibial condyle BMDs in lateral square region of interest were calculated for the tibia. And we calculated the BMD of both lateral and medial femoral condyle in square regions of interest of the same size as those on the tibial condyles (Fig. 3).
Statistical Analysis
Statistical analysis was performed using Microsoft Office Excel and Statcel 3 program (OMS, Inc., Hyogo, Japan). Both BMD and area of affected lesion in MRI for each subject were analyzed by Student’s t test to compare differences between the two groups. For the existence or non-existence of treatment related to osteoporosis, the Chi square test was used to evaluate the significance of differences. All results of statistical tests were regarded as significant with p<o.o5.
RESULTS
There were no significant changes in age, BMI, femoro-tibial angle and the number of definition of Kellgren-Lawrence in plain X-ray between these two groups. All patients were female and had no past illness of Rheumatoid arthritis, diabetes, chronic kidney disease which are connected with bone fragility. BMD of lumbar spine of all cases was categorized in osteoporosis less -2.5SD in T-score (Table 1). BMD in femoral condyle of affected side was significantly lower than that of the healthy side in the operation group, whereas there were no significant differences between both tibial sides in conservative group. The area of lesion which showed low intensity indicated that the operation group was significantly larger than that of the conservative group on T2 weighted images both coronal and sagittal views. It also had the same results in high intensity on T2 weighted images (Table 2). These results imply that we indicated that those who have low BMD and a large affected area have the tendency to undergo surgical procedure.
| Operation group (n=10) |
Conservative group (n=10) |
p-value | |
|---|---|---|---|
| Age (years) | 77±7.9 | 82±6.4 | 0.150a |
| Height (cm) | 155±3.2 | 152±5.1 | 0.012a |
| Weight (kg) | 56.8±7.9 | 52.2±4.6 | 0.039a |
| BMI (kg/m2) | 24±3.0 | 25.1±3.6 | 0.201a |
| BMD: femur (g/cm2) | 0.454±0.085 | 0.489±0.092 | 0.438a |
| BMD: lumbar spine (g/cm2) | 0.595±0.032 | 0.562±0.048 | 0.052a |
| K-L grade I (n) | 4 | 6 | 0.158b |
| K-L grade II (n) | 6 | 4 | 0.205b |
| FTA | 173 | 172 | 0.204b |
b χ2 test
| Healthy side (n=10) |
Affected side (n=10) |
p-value | |
|---|---|---|---|
| Operation | 0.933 | 0.593 | 0.045a |
| DXA of Femur (g/cm2) Conservative |
0.890 | 0.590 | 0.042a |
| Operation | 0.782 | 0.689 | 0.720a |
| DXA of Tibia | |||
| (g/cm2) Conservative | 0.579 | 0.501 | 0.602a |
| Conservative group (n=10) |
Operation group (n=10) |
p-value | |
| Low | 31.1±0.9 | 175.1±1.1 | 0.041a |
| MRI(Coronal, mm2) | |||
| High | 7.2±1.1 | 47.7±0.9 | 0.049a |
| Low | 18.3±0.9 | 65.3±2.1 | 0.048a |
| MRI(Saggital, mm2) | |||
| High | 4.0±1.1 | 20.0±0.9 | 0.035a |
DISCUSSION
Although a clear consensus about the cause and prognosis of SONK has yet to be reached [14-18], in the cases that required the surgical procedure had low BMDs and a large area of suspected lesion, we focused on BMD, the radiological procedures and MRI when considering the case of SONK. These cases were diagnosed as osteonecrosis of the medial femoral condyle based on the preoperative imaging and clinical findings, which showed bone collapse in the femoral medial condyle caused by severe osteoporosis. This suggests that the fragility of subchondral bone in the medial femoral condyle might have a close relationship with the imaging diagnosis of SONK.
Karvoren et al. [19] suggested that BMD of the subchondral bone in middle-grade osteoarthritis of the knee is lower than that of the surrounding joint surface in osteoarthritic knees, which implies that the subchondral bone area in the initial phase of osteoarthritis of the knee is fragile with mechanical stress, such as weight-bearing. Moreover, Karachialios et al. [20] noted that osteoarthritis of the knee could lead to the detection of SONK, which means idiopathic bone necrosis on MRI in Kellgren-Lawrence stage 1-2. Kesemenli et al. [21] noted that SONK is regarded as a microfracture. Fotiadis et al. [1] also noted that osteoporotic joint subchondral bone can lead to bone fragility, causing repeated microfractures, and its accumulation finally leads to osteonecrosis.
Therefore, osteoarthritis of the knee with sudden onset may be due to the collapse of subchondral bone caused by loss of BMD. Although there have been some reports that osteonecrosis was the cause of osteoarthritis in the light of radiological findings, as a matter of fact, there might exist cases of progressive local osteoarthritis that were caused by fracture of subchondral bone because of osteoporosis.
Next, we pay attention to the relationship between the size of affected area and prognosis with BMD. Those who underwent surgical procedures were relatively larger than those who received conservative treatment with respect to the size of MRI in both high and low intensity area on T2 weighed images. Previous papers have reported the prognosis about the size of SONK on MRI. Lecouvet et al. [22] suggested that the lesion of affected low intensity area which showed both the depth over 4mm and the length over 14mm on T2 weighted images was a bad prognosis which might had the possibility of changing into osteonecrosis. Yates et al. [23] also mentioned that the lesion of affected low signal area, which showed both the length within 30mm and the height within 8mm on T2, weighted images have no relation with bad prognosis. Therefore, we measured the size of affected lesion by using MRI on T2 weighted images. Our results indicated that the relatively larger size of affected area on T2 weighted images might predict the bad prognosis whether these were low signal or high signal. That means it may be possible f to predict the prognosis for SONK by measuring its area in T2 weighted image on MRI.
In addition, these surgical procedure-intervene cases also had low BMD in the medial femoral condyle and proximal tibia compared to conservative cases. Considering both MRI and BMD results, we assume that osteoporosis and large affected lesion of SONK were important factors in determing whether this disease will progress or not.
In other words, most of the SONK patients who have low bone mineral density in the lesion within -2.5SD in the lumbar spine or femur and a large affected area on MRI are likely to progress to osteonecrosis, those who have no osteoporosis and a small affected area are less likely to have a bad prognosis. We suppose that patients who suffer from and are diagnosed as SONK are mainly osteoporotic women, and their osteonecrosis accompanied with osteoporosis are seen because of our advocated etiology which implies that the osteonecrosis that occurs is due to the collapse and focal separation of bone from a blood supply [24].
However, our study design had several contradictions and limitations. First, we found that progression to surgery was related to increased MRI size of lesion. While we also found decreased regional bone density on the side of the lesion. That means the degree of decreased bone mineral density appears to be the same in the non-operative and operative group. These results indicate that there might exist some other risk factor which promote the SONK if osteoporotic patients have microfracture of knee.
Second, we had only ten patients who underwent surgical procedure and conservative treatment which followed up within one months of the onset. That implies radiographic changes prevent its symptoms from being diagnosed for a long time, so there may be many cases in which we overlooked this disease. We need to further investigate SONK by collecting data from patients who are suspected of having the symptom of sudden onset and early stage osteoarthritis of the knee.
CONCLUSION
Our study emphasized the importance of DEXA and MRI in searching and predicting the prognosis for SONK. It is important for orthopedic surgeons to detect the early phases of SONK and decide how to treat it adequately as soon as possible. Our research suggests that there might exist many cases of SONK which do not appear on radiographic images during early examination. Those who are diagnosed with osteoporosis complain of sudden knee pain. We should pay attention to early phase SONK and perform both DEXA and MRI in the affected lesion.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The South Akita Orthopedic Clinic and Akita University Graduate School of Medicine supported this study. The authors would like to extend their appreciation to the patients in this study and thank Dr. Yusuke Sugimura who assisted and supported their research.


