All published articles of this journal are available on ScienceDirect.
Revision of Metal-on-metal Hip Arthroplasty with Well Fixed and Positioned Acetabular Component Using a Dual-mobility Head and Review of Literature
Abstract
Background:
As a consequence of use of metal-on-metal hip arthroplasties some patients have precised revision for pain or metal hipersensivity reactions among other causes. We propose to salvage monoblock acetabular component and femoral component using a dual-mobility head and perform a lower morbidity operation in young patients preserving host bone stock in cases with well fixed and positioned components.
Objective:
(1) What clinical problems have been reported in patients with Metal-on-metal hip arthroplasties? (2) Could the tribocorrosion potentially cause a fracture of neck femoral component? (3) Can be the dual-mobility head a recourse in metal-on-metal hip revision?
Methods:
Ten patients were revised for pain or/and raised Cobalt/Chromium levels between August 2012 and December 2015. In three cases femoral neck component was fractured and femoral revision was necessary. In four hips, acetabular and femoral components could be maintained. Age, body index mass, ion levels, acetabular position, size of acetabular component and femoral head, approach, blood transfunsion and time of hospitalization were analized.
Results:
At a mean follow-up of 25,6 months (6 to 45) the mean postoperative HHS was 92. It was not statistically significant because several patients were low sintomatic before surgery, but had raised Cobalt/Chromium levels in the blood. All patients had near-normal levels of Cobalt/Chromium during the first 6 months after revision surgery. No relevant complications were reported.
Conclusion:
The use of dual-mobility head can be an acceptable option to revise metal-on-metal arthroplasties correctly oriented with abscence of loosening or infection signs and keeping bone stock in young patients.
INTRODUCTION
In the last 20 years metal-on-metal (MoM) total hip arthroplasty has reached much interest. The advantages of MoM articulation include improved wear because no polyethylene was used, which is particularly useful in young patients, and a large femoral head gives stability and mitigate dislocation risk, and preservation of proximal femoral bone stock in resurfacing arthroplasties [1].
However MoM bearings can also produce important complications like, among others, Aseptic Limphocyte Vasculitis Associated Lesions (ALVAL) or Adverse Local Tissue Reactions (ALTR) [2]. These are metal hipersensivity reactions produced by MoM friction surfaces and the corrosion caused by assembled pieces of modular large-head [3-5].
Blood levels of metal ions can accumulate and achieve high values, especially in patients with renal insufficieny and they are related with neurologic toxicity cardiotoxicity and thyroid toxicity [6, 7]. Subcapital femoral fracture or necrosis of femoral head are other causes of failure in patients with hip resurfacing replacements.
Most of patients with MoM hip implants are young with good quality bone. There are several alternatives to use in the revision of MoM. Single-component revision of pair of friction, has some advantages over femoral and acetabular component revision since it is a less invasive operation and it has lower morbidity [8]. Explantation of well fixed components is a highly morbid procedure involving loss of existing bone stock and increased blood loss in younger active cases.
Dual-mobility articulation consists of a 28 or 22-mm meta femoral head that snaps into a mobile polyethylene. The polyethylene liner functions as a large femoral head, increasing the jump distance required to dislocation and increasing functional range of motion [9]. This option for revision metal-on-metal hip replacements is related with less morbidity, secondary to faster operative time, preservation of host bone stock and a lower rate of dislocation since the large head with dual-mobility articulation is kept.
The aim of our study is to report on our experience the use of a dual-mobility femoral head leaving monoblock acetabular component when it was well fixed and positioned. These conditions are also applied for femoral component except in resurfacing hip arthroplasties.
MATERIAL AND METHODS
Between August 2012 and December 2015, 10 MoM hip arthroplasties were revised in 9 patients, for pain and raised levels of cobalt/chromium or elevated blood ions only.
The revisions included were 2 resurfacing replacements and 8 large-head MoM hip arthroplasty in nine patients were revised. The inclusion criteria were revision of metal-on-metal hip arthroplasty keeping acetabular component and replacing femoral head by dual-mobility head, Cr/Co ion levels >7 μ/L or femoral neck fracture of femoral component. Exclusion criteria included revision of two components of metal-on-metal hip arthroplasty, revision of M-o-M hip arthoplasty explanting acetabular component and revision of M-o-M for infection.
We consider <5μ/L Chromium and <2μ/L Cobalt levels as normal values. When cobalt values >10 μ/L are indicative of an increased joint wear and potentially adverse local tissue reaction (ALTR) could be developed. Cobalt values >20 μ/L are unacceptable beacuse of systemic toxicity. These values were taken from the Spanish Hip Society (SECCA, Sociedad Española de Cirugía de la Cadera) which are based on the European Hip Society guidelines. In the Hospital for Special Surgery, New York, Su EP. et al., take >7μ/L cobalt or chromium level as a cut off to consider the diagnosis of accelerated wear (metallosis) [10].
All patients were men with mean age for primary surgery of 51,3 years (range 34-64 years) and average time until revision surgery was 4,7 years (range 2-8 years). Body Mass Index (BMI) was 30 (range 24,2 - 38,7).
Ther were 6 right and 4 left hips. The average cup abduction angle was 48,9º (range 38º-56º), and the anterversion angle of the acetabular component was not measured because de hip-TC was not available in all patients. The mean acetabular component diameter index was 54 (range 48-62) and the mean head diameter was 48 mm. Tha average modular femoral head was 47,6mm (range 42 to 56); it was, standard in four patients and +6 in three. All data are shown in Table 1.
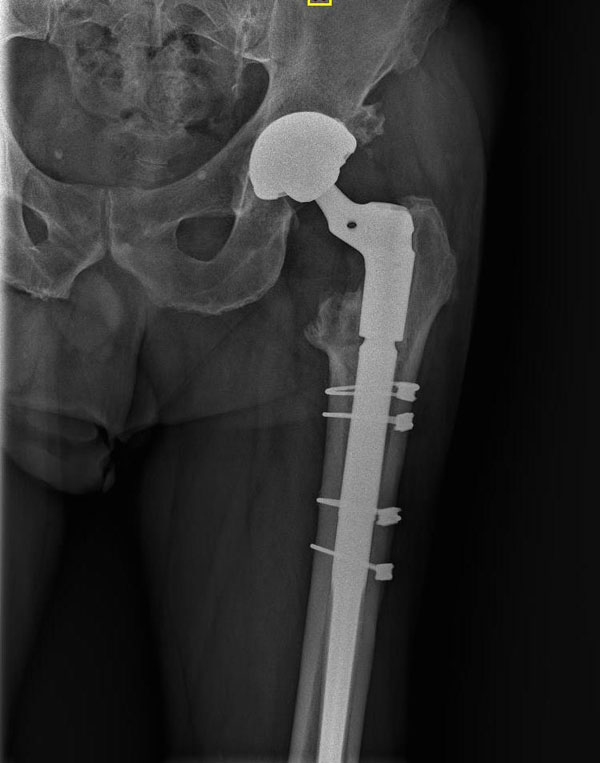
Of importance, in three cases the revision surgery was performed because the modular femoral neck component fractured (Fig. 1). Logically, all three patients precised revision of femoral component which was attached to a doublemobility femoral head, mantaining the acetabular piece (Fig. 2). Case number 5 also needed a femoral component revision because it was impossible to remove the large-femoral-head. Patients 8 and 10 underwent resurfacing arthroplasties and substitution of femoral component Figs. (3 and 4). In the remaining 3 patients acetabular and femoral components were well fixed and appropriately positioned and large-metal-head was removed and replaced by dual-mobility head leaving two primary components. Patient 3 was a bilateral case.




All operations were performed by senior orthopedic surgeons mainly using a posterolateral approach.
Preoperatively and postoperatively clinical outcomes were analyzed using U Mann Whitney U-test, with a P value less than 0,05 considered significant.
RESULTS
At a mean follow-up of 25,6 months (6 to 45 months) the mean post-operative Harris Hip Score (HHS) was 75 (range 58 to 95) while preoperative was 92 (range 79 to 99). The 17 point average improvement was not significant (p > 0,05 Mann Whitney U-test). We would like to remark that most patients were low sintomatic but had increased the blood ion levels.
All patients evaluated had a decrease ratio cobalt/chromium levels in the first six months of surgery.
Cloudy or dark synovial fluid was found in the joint during the revision surgery in the most of patients. Intraoperative cultures were negative for all patients. The operative findings were thin purulent material, inflammatory dark staining of the tissues. No malpositioning or component damage of acetabular component was observed.
There were no cases of dislocation, deep venous thrombosis, or nerve palsy during the follow-up. There was a re-operation performed for superficial infection by Serratia and S epidermidis in the first month of surgery in patient 4. He was treated with debridement preserving the components of arthroplasty.
All patients had a normal rate of cobalt in the first six months. There were one patient who showed a small increase of chromium level at sixt months that could possibly be ascribable to a bilateral case.
The average hospitalization time was 14 days (range, 4 - 62 days). The patient who needed 62 days in hospital had a decompensated liver cirrhosis and required a femoral component revision. Two other with prolonged hospitalization, 17 and 28 days, had also required a femoral revision.
The average blood transfusion units were 1,1 (range, 0 to 7 units) and the cirrhotic patient needed 7 units.
All patients had radiographs performed december 2015 and no osteolysis or obvious wear of the outer polyethylene liner was identified. We did not find a significant relationship between BMI and fracture of the femoral component. Moreover, we also did not observe any correlation between the size of acetabular component or the size of the head with cobalt/chromium levels and the pain or functional scores.
DISCUSSION
Our study extends the experience of performing a revision of metal-on-metal hip arthroplasty leaving acetabular component (if it is well fixed and positioned) using dual mobility head. It includes 10 cases with good results during a 2-year follo-up. It is also of interest tha 3 of the 9 patients presented a femoral neck fracture of the femoral component. In addition, we failed to find a significant relationship between BMI and fracture of femoral component, but from our point of view greater BMI gives more possibilities to elevate cobalt/chromium blood levels. Moreover, we did not observe an influence of the acetabular component size and the head size with the cobalt / chromium plasma levels, pain or the functionals scores.
The goal of revision surgery is to provide a stable hip specially in young patients [11]. The reported complication rate with revision to THA (total hip arthroplasty) is: for an adverse reaction to metal wear debris has been 10-50%, the re-revisio rate has been 5-38%, and the rate of dislocation has been 4-19% [12, 13]. The increased dislocation rate may be due to the decrease of the femoral head diameter in revisions of THA [13-16]. The use of dual-mobility device compared with standard revision of THA allows the surgeon not only to mantain a large femoral head size similar in size to the native one but also to increase, potentially, the stability and range of motion postoperatively [9, 17, 18]. Therefore, dual-mobility head can be used to convert some MoM arthroplasties with a secure acetabulum to a polyethylene-metal bearing if acetabular component is well positioned [19]. Luk A. Verhelst, who proposed to leave the metal socket in situ and replace the femoral implant with double-mobility component in patients presenting a well-fixed and oriented cup in the context of pain and raised ion levels [20]. We have also observed the even a slight malalignement cup led to an increase of polyethylene wear debris, like in MoM arthroplasties may produce an increase of chromium and cobalt ion levels [21, 22].
Some papers have reported that in hip resurfacing arthroplasties, matching a stemmed total hip femoral component with a metal head to the existing metal acetabular component has been successful only when the reason for resurfacing revision has been femoral loosening or femoral neck fracture [11, 14, 23, 24]. Therefore there were several surgeons that thought to retain the acetabular component for conversion of failed femoral component [10]. Pritchett J.W. serie suggest a more limited procedure of one-component revision results in less blood loss and infection compared to revision of THA [9, 11, 13, 25]. These statments were also present in our follow up. De Steiger RN et al. reported that femoral-only revision had a risk of re-revision similar to that of revision of both, the acetabular and femoral components [25]. Ball ST et al. concluded that conversion of a hip resurfacing with a femoral-side failure in a total hip replacement appeared to be comparable with primary total hip arthroplasty in terms of surgical effort, safety, blood loss or complications rates [23]. In our study a similar surgery had been performed retaining acetabular component in all cases and femoral too in 5 cases. In the remaining 5 patients the femoral component was revised because of resurfacing arthroplasty, or femoral neck fracture of the femoral component. On the other hand many authors reported to revision both components if a biological failure mechanism is found to an alternative bearing combination in hip resurfacing arthroplasty [13, 26]. Nevertheless, a recent study recognizes that patients who undergo conversion of hip resurfacing to total hip arthroplasty have an increased risk of recurrent revision surgery and their functional outcomes are inferior to primary total hip replacement [27].
Other possibilities to preserve well positioned monoblock acetabular component were to cement of an unconstrained tripolar implant into an acetabular component [28, 29].
Dual-mobility technology has been shown to have excellent wear characteristics with polyethylene wear measurements being comparable to conventional metal-on-polyehtylene designs. Their specific design increases the surface subjected to friction and can raise the suspicion of increased wear and periprosthetic osteolysis [30]. To know the wear rates on standard anteroposterior views, the femoral head is the most often invisible because of the metal back, which makes measurement difficult [31]. Radiostereometric analysis (RSA), developed by Selvik in the early 1970s, enables precise measurement of femoral head penetration in the acetabular component [32-34]. Some authors think that measurement of femoral head penetration cannot differentiate between wear of the small or the large articulation [30]. Adam P. et al. published that mean external polyethylene wear is only a sixth of total wear [35]. Following this line, the same author reported that the motion is supposed to occur preferentially at the inner bearing, and limited polyethylene wear at the outer bearing [19, 35, 36]. Such an assumption that was documented in a laboratory study of retrieved polyethylene inserts ten years ago [35]. We are agree with all of these comments. However some biomechanics studies recognize greater wear at the convex bearing surface of the liner [26].
Also, when studying polyethylene wear in mobile liners in dual mobility implants, potential wear due to contact between the femoral neck and the retention collar of the liner (“third articulation”) must be taken into account. This wear is not measurable using radiographic techniques, but can be responsible for the release of polyethylene particles at the origin of osteolysis [28, 30].
It has been described the relationship between cobalt/chromium ratios and the high prevalence of head-stem junction corrosion in MoM total hip arthroplasty [4, 37]. In this sense our patient 5 needed a revision of femoral component because it was impossible to remove large metal head. A severe fretting corrosion had been ocurred. Yet, corrosion of modular head-neck junction has been identified in metal-on-polyethylene hip prothesis too [38].
In our study we have been included three patients with modular femoral neck fracture. There is a rare complication related in literature [39]. The combined effects of crevice and fretting corrosion, large diameter femoral head, long modular neck, patient size and probably activity level may lead in creating an environment susceptible to a fatigue fracture [39, 40].
The use of metal ion tests allows to identify patients at risk, thereby it could accelerate the time frame of their care and conversion surgery with dual-mobility head if acetabular component is in the correct position. There is sufficient evidence of significant linear relationship between the concentration of cobalt/chromium in blood/serum and wear rates appeared in explanted prosthetic components [10, 41]. The normalitzation of blood ions concentration occurs during the first year after revision [17].
| BMI | Diagnostig primary THA | Prosthesis |
Age of 1º THA (years) |
Revision Age (years) |
Follow up (months) |
Diagnostig of revision | Ions pre-revision | Ions last control | Acetabular position | Size of acetabular component | Size of femoral Offset | Size of head | HHS before revision | HHS last control | Approach |
Time of hospitalization (days) |
Blood transfusion (units) |
Complications | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 27,5 | Coxartrosis | THA* | 58 | 61 | 45 | Femur neck fracture | 4,6Co / 0,9Cr | Co<1 Cr<0,5 |
38º | 52 | +6 | 46 | 75 | 99 | Postlat.* | 17 | 4 | no |
| Patient 2 | 28,7 | Coxartrosis | THA | 50 | 53 | 43 | Femur neck fracture | 13Co / 11Cr |
Co<1 Cr<0,5 |
55º | 52 | +6 | 46 | 87 | 89 | Postlat. | 62 | 7 | no |
| Patient 3(right) | 24,2 | Coxartrosis | THA | 62 | 66 | 29 | Pain and raised ion level | 157Co / 140Cr |
Co<1 Cr15 |
48º | 50 | 0 | 44 | 95 | 99 | postlat | 5 | 0 | no |
| Patient 3(left) | 24,2 | Coxartrosis | THA | 64 | 66 | 29 | Pain and Raised ion level | 157Co / 140Cr |
Co<1 Cr15 |
50º | 48 | 0 | 42 | 95 | 99 | postlat | 9 | 0 | no |
| Patient 4 | 32,1 | AVN* | THA | 34 | 39 | 27 | Raised ion levels | 98Co / 55Cr |
Co<1 Cr6,2 |
54º | 50 | 0 | 44 | 82 | 85 | postlat | 7 | 0 | Superficial infection |
| Patient 5 | 36,5 | AVN | THA | 34 | 42 | 26 | Femur neck fracture | Co<1 Cr0,5 |
56º | 60 | 54 | 76 | 79 | Antlat* | 28 | 0 | no | ||
| Patient 6 | 28,3 | AVN | THA | 46 | 52 | 20 | Raised ions levels | 16Co / 18Cr |
Co<1 Cr3,5 |
54º | 62 | +6 | 56 | 88 | 99 | postlat | 5 | 0 | no |
| Patient 7 | 29,4 | Coxartrosis | HR* | 56 | 59 | 20 | Pain and raised ion levels | 10Co / 10Cr |
Co<1 Cr<0,5 |
42º | 52 | 44 | 58 | 96 | postlat | 5 | 0 | no | |
| Patient 8 | 30,4 | Coxartrosis | THA | 56 | 63 | 11 | Raised ion levels | 13Co / 7Cr |
Co 1 Cr1,9 |
53º | 58 | 0 | 52 | 71 | 91 | postlat | 5 | 0 | no |
| Patient 9 | 38,7 | Coxartrosis | HR | 53 | 59 | 6 | Raised ion levels | 16Co / 12Cr |
Co<1 Cr1,9 |
39º | 54 | 48 | 95 | 93 | postlat | 4 | 0 | no |
*THA. Total Hip Arthroplasty
*HR. Hip Resurfacing
*Postlat. Postero-lateral approach
*Antlat. Antero-lateral approach
CONCLUSION
According to our findings, the use of dual-mobility head can be an acceptable option to revise MoM arthroplasties correctly oriented with abscence of loosening signs. Besides presenting a lower morbidity, this kind of revision preserves host bone stock and decreases the risk of dislocation. Contraindications are likely to be related to malposition of components, suspected infection and obvious signs of loosening of the acetabular component. The main limitations of this work are the reduced size of our series and the relatively short duration of follow-up.
LIST OF ABBREVIATIONS
| ALTR | = Adverse local tissue reactions |
| ALVAL | = Aseptic limphocyte vasculitis associated lesions |
| BMI | = Body index mass |
| HHS | = Harris hip score |
| (MoM) | = Metal-on-metal |
| RSA | = Radiostereometric analysis |
| SECCA | = Sociedad española de Cirugía de la Cadera |
| THA | = Total hip arthroplasty |
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


