All published articles of this journal are available on ScienceDirect.
Comparing Transtibial and Anteromedial Drilling Techniques for Single-bundle Anterior Cruciate Ligament Reconstruction
Abstract
Background:
Among the many factors that determine the outcome following anterior cruciate ligament (ACL) reconstruction, the position of the femoral tunnel is known to be critically important and is still the subject of extensive research.
Objective:
We aimed to retrospectively compare the outcomes of arthroscopic ACL reconstruction using transtibial (TT) or anteromedial (AMP) drilling techniques for femoral tunnel placement.
Methods:
ACL reconstruction was performed using the TT technique in 49 patients and the AMP technique in 56 patients. Lachman and pivot-shift tests, the Lysholm Knee Scale, International Knee Documentation Committee (IKDC) score, Tegner activity scale and visual analog scale (VAS) were used for the clinical and functional evaluation of patients. Time to return to normal life and time to jogging were assessed in addition to the radiological evaluation of femoral tunnel placement.
Results:
In terms of the Lysholm, IKDC, Tegner score, and stability tests, no significant differences were found between the two groups (p > 0.05). Statistical analysis revealed reduced time to return to normal life and jogging in the AMP group (p < 0.05). The VAS score was also significantly reduced in the AMP group (p < 0.05). The position of the femoral tunnel was anatomically appropriate in 51 patients in the AMP group and 5 patients in the TT group.
Conclusion:
The AMP technique is superior to the TT technique in creating anatomical femoral tunnel placement during single-bundle ACL reconstruction and provides faster recovery in terms of return to normal life and jogging at short-term follow-up.
INTRODUCTION
Surgical reconstruction is now widely accepted as the treatment of choice for functional knee instability due to anterior cruciate ligament (ACL) deficiency especially in young patients who are involved in physically high demanding activities [1]. This procedure is well-known for its ability to allow an individual to return to preinjury activity levels, which may not be achieved with non-surgical treatment [2]. In spite of the considerable research focused on ACL reconstruction, the increased risk of early knee osteoarthritis and the presence of rotational instability post-surgery have not been fully investigated yet. As a result, controversy remains regarding the best technique for reconstruction; thus, it is still the subject of extensive research [3, 4]. Among the many factors that determine the outcome following ACL reconstruction, the position of the tunnels created for graft fixation is known to be of critical influence, and malpositioning of the femoral tunnel occurs 3 times more frequently than malpositioning of the tibial tunnel [3, 5, 6]. Femoral tunnel position is more critical because it is closer to the central axis of knee rotation, and malpositioning of the femoral tunnel has been reported to be the most frequent cause of graft failure [7, 8]. A non-anatomically placed graft can create abnormal tensile and compressive forces, which affect graft healing and re-integration processes [9].
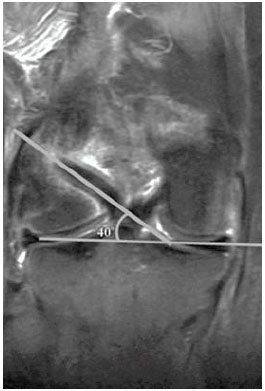
Anatomical reconstruction of the ACL involves the placement of the femoral tunnel at the center of the original femoral footprint [10]. Recent studies have shown that anatomic positioning of the femoral tunnel best restores native knee kinematics by allowing appropriate graft tension throughout the range of motion, and results show increased rotational stability, as well as translational and tensioning patterns similar to the native ACL [11, 12]. The transtibial (TT) technique is the most widely used method for drilling the femoral tunnel during ACL reconstruction, but positioning the femoral tunnel anatomically is difficult and constrained by the position of the tibial tunnel. As a result, the graft is oriented in a relatively vertical direction, in the footprint of the anteromedial bundle of the ACL [13]. Thus, over the past decade, there has been a trend transitioning from use of the TT drilling technique toward the anteromedial portal (AMP) drilling technique in order to achieve more anatomical femoral tunnel placement. The AMP technique requires independent drilling through an additional anteromedial portal in a more horizontal direction [3, 14] (Fig. 1).
According to anatomical studies, the AMP technique currently allows for a more anatomical femoral tunnel position within the native ACL femoral footprint compared with the TT technique. However, no adequate studies exist that compare the clinical and functional outcomes of these two techniques [2, 9]. Thus, this study aimed to retrospectively compare the radiological and clinical outcomes of arthroscopic ACL reconstruction using the TT and AMP drilling techniques for femoral tunnel placement.
MATERIALS AND METHODS
Patients
Among the patients who underwent single-bundle ACL reconstruction between February 2011 and July 2014 using an autologous hamstring graft, 105 eligible patients were included in this retrospective study. ACL reconstruction was performed using the TT technique in 49 patients (4 female, 45 male; mean age, 26.8 years, range 18-40) and the AMP technique in 56 patients (4 female, 52 male; mean age, 25.5 years, range 17-35). The inclusion criteria for this study were as follows: less than 6 months between injury and surgery, at least 24 months of follow-up, a healthy contralateral knee, and patient age between 16 and 40 years. Patients who underwent concomitant surgery during ACL reconstruction for other combined injuries, such as collateral ligament injury, posterior cruciate ligament injury, or posterolateral corner injury were excluded from the study. All patients were operated by two senior surgeons. This study was approved by our institutional ethics committee and informed consent was obtained from all patients for the use of their demographic and radiological data.
Surgical Technique
Arthroscopic examination was performed and ACL rupture was confirmed before harvesting the graft. Quadruple-strand semitendinosus and gracilis autografts were used in all patients. The standard technique was performed to place the tibial tunnel in both the TT and AMP groups [15]. The tibial tunnel was prepared in the footprint of the ACL at an angle of 45° to the tibial shaft. In the TT group, the standard aiming guide with a 7-mm offset was placed through the tibial tunnel at the 11 o’clock position of the right knee and the 1 o’clock position of the left knee, and a pin was advanced to determine the femoral tunnel position. A cannulated reamer was then used transtibially to create the femoral tunnel. In the AMP group, a three-portal technique (anterolateral, central anteromedial, and low anteromedial) was used. The low AMP was created under arthroscopic visualization; a spinal needle was advanced into the joint just above the anterior horn of the medial meniscus and 1.5 cm medial to the medial border of patellar tendon and to create the femoral tunnel independently from the tibial tunnel. It is important to keep a security distance at least 2 mm from the cartilage of the medial femoral condyle once the drill passes through this portal [16]. The midpoints of the remnants of the anteromedial and posterolateral bundles of the ACL were marked with a thermal device. The lateral intercondylar ridge and lateral bifurcate ridge served as the bony landmarks for the femoral attachments. The lateral intercondylar ridge is an osseous landmark in the medial wall of the femoral lateral condyle that runs from proximal to distal and anterior to posterior in the anatomic position. There is no ACL attachment anterior to this ridge. Lateral bifurcate ridge is an osseos landmark that runs from anterior to posterior and separates the AM and PL bundles femoral attachment site [17]. The knee was flexed to 120°-130°, and the guidewire was placed in the center of the two insertion areas via the low AMP. Femoral drills were selected according to the graft diameter, and the tunnel was drilled with a cannulated reamer using a freehand technique. An endobutton continuous loop device was used for femoral fixation of the graft. Pre-tensioning of the graft was performed by flexing and extending the knee through the range of motion. The absence of graft impingement was confirmed by arthroscopic examination. Tibial fixation was performed in 20° of flexion using a bioabsorbable screw and a U staple with a posterior drawer.
Postoperative Care
The same postoperative accelerated rehabilitation protocols were used for both groups. Knee braces or sleeves were not employed in any of the patients. All patients were allowed weight-bearing as tolerated with crutches on the day of surgery. After three weeks, weight-bearing without crutches was permitted.
Clinical and Radiological Assessment
At the last follow-up, all patients were examined by an orthopedic surgeon who was blinded to the relevant study details and who was not the operating surgeon. Lachman and pivot-shift tests were performed to evaluate the anterior-posterior and rotational stability, respectively. The Lysholm Knee Scale, International Knee Documentation Committee (IKDC) scoring system, Tegner activity level, and visual analog scale (VAS) for patient satisfaction were used for the clinical and functional evaluation of patients before surgery and at the last follow-up [18, 19]. The time to return to normal life and time to return to jogging were assessed. For the radiological evaluation of tunnel placement, in order to determine whether the reconstructed ACL fell outside of the anatomical range, the criteria developed by Illingworth et al. were used [20].
Statistical Analysis
Statistical analyses were conducted using SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL). When the numerical values for the two independent groups were normally distributed, Student’s t test was used, and when normal distribution was not achieved, a Mann-Whitney U test was performed to compare the groups. For categorical variables, the ratios between the groups were analyzed by chi-square test. As the conditions for parametric tests were not met, a Monte Carlo simulation was used to evaluate the numerical variables. A p value < 0.05 was considered statistically significant.
RESULTS
Statistically significant differences were not found between the groups with regard to age, sex, body mass index (BMI), mean follow-up period, and time from injury to surgery (p > 0.05) (Table 1). The mean follow-up periods for the AMP and TT groups were 30.5 months (range, 24-42 months) and 28.6 months (range, 26-38 months), respectively. The mechanism of injury involved sports activities in 32 patients (65%) in the TT group and 41 patients (73%) in the AMP group. Assessment of the preoperative and postoperative IKDC and Lysholm scores showed a significant improvement in both groups (p < 0.05). In terms of the Lysholm and IKDC scores and Tegner activity levels, no significant differences existed between the groups at the last follow-up evaluation (p > 0.05) (Table 2).
| TT Group | AMP Group | p Value | |
|---|---|---|---|
| Patients (n) | 56 | 49 | |
| Sex (male: female, n) | 52:4 | 45:4 | 1 |
| Age (mean ± SD, years) | 25.5 ± 5 | 26.8 ± 5.7 | 0.406 |
| BMI (mean ± SD, kg/m2) | 24.9 ± 2.9 | 25.1 ± 2.7 | 0.735 |
| Follow-up (mean ± SD, months) | 30.1 ± 5.4 | 30.9 ± 5.6 | 0.441 |
| Time from injury to surgery (mean ± SD, weeks) | 10.3 ± 5.1 | 10.6 ± 4.7 | 0.415 |
| Parameters | Anteromedial | Transtibial | p Value |
|---|---|---|---|
| IKDC score | 93.1 | 91.4 | 0.614 |
| Lysholm score | 95.4 | 93.9 | 0.545 |
| Tegner activity level | 6.3 | 6.1 | 0.415 |
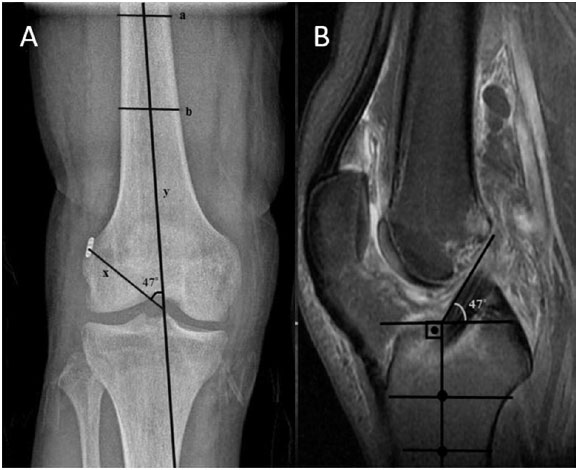
Lachman and pivot-shift tests showed no significant differences between the groups (p > 0.05) (Table 3). Statistical analysis revealed that a reduced time was needed to return to normal life and jogging in the AMP group than in the TT group (p < 0.05), and a statistically significant difference was observed between the two groups (p < 0.001). Moreover, higher patient satisfaction was achieved for the AMP group following surgery according to analysis of VAS scores (p < 0.05) (Table 4). AMP technique was found to be superior to the TT technique in creating femoral tunnels within anatomical range, according to the radiological evaluation method of Illingworth (p < 0.001). The reconstructed ACL fell within an anatomical range in 51 patients (91%) in the AMP group and 5 patients (10.2%) in the TT group (Fig. 2).
| Parameters |
Anteromedial n (%) |
Transtibial n (%) |
p Value |
|---|---|---|---|
| Pivot-shift test | 0.056 | ||
| 0 | 42 (75.0) | 29 (59.2) | |
| 1 | 14 (25.0) | 19 (38.8) | |
| 2 | 0 | 1 (2) | |
| 3 | 0 | 0 | |
| Lachman test | 0.059 | ||
| 0 | 42 (75.0) | 29 (59.2) | |
| 1 | 14 (25.0) | 17 (34.7) | |
| 2 | 0 | 3 (6.1) | |
| 3 | 0 | 0 |
| Anteromedial | Transtibial | p Value | |
|---|---|---|---|
| VAS score (mean ± SD) | 9.4 ± 0.8 | 8.9 ± 0.8 | 0.002 |
| Time to normal life (mean ± SD, weeks) | 7.5 ± 0.9 (8) | 9.1 ± 1.3 (9) | < 0.001 |
| Time to jogging (mean ± SD, weeks) | 12.4 ± 1.6 (12) | 14.4 ± 2.2 (14) | < 0.001 |
DISCUSSION
The principal finding of this comparative study is that the AMP technique is superior to the TT technique in achieving anatomical femoral tunnel placement. The patients in the AMP group began jogging and returned to normal life significantly earlier at short-term follow-up compared with patients in the TT group.
The most frequent technical flaw resulting in the failure of ACL reconstruction is the non-anatomical placement of the femoral tunnel [5-11]. In a cadaveric study by Gadikota et al., improved outcome after ACL reconstruction was notably related to the maximum femoral ACL footprint coverage achieved by the surgical tunnel [21]. Creation of a femoral tunnel with the TT technique requires a relatively short operative time and has been commonly performed with successful results for a long time [22]. However, when using the TT technique, the femoral tunnel is typically placed anteriorly and higher in the intercondylar notch compared with the original ACL femoral footprint [23, 24]. Only the anteromedial bundle of the ACL may be covered by the TT drilling technique, which results in better restoration of sagittal plane stability than rotational stability, which may remain inadequate [25]. The abnormal femoral tunnel placement observed in the TT technique is attributed to the dependency of the femoral tunnel position on the antecedently drilled tibial tunnel [26]. In an attempt to achieve anatomical femoral tunnel position via the TT technique, Golish suggested a far medial entry into the tibia [27]. Controversially, many authors have concluded that attempting to create an anatomical femoral tunnel position through a medial entry into the tibia would require a starting point too close to the tibial joint line, resulting in a relatively short medial tibial tunnel and a tunnel length-graft length mismatch [23, 26]. Youm et al. used a modified TT technique, positioning the tibia in internal rotation and varus alignment while creating the femoral tunnel. They noted that adjusting the guidewire within the native ACL site using the modified TT technique is easily possible [28].
On the other hand, numerous studies have suggested that the AMP technique facilitates a more anatomic and horizontal femoral tunnel, independent of tibial tunnel placement within the native ACL femoral attachment site, and provides greater rotational stability. Furthermore, these studies suggest that a more horizontal placement of the graft decreases the risk of graft impingement [10, 29, 30]. However, there are several potential surgical difficulties with regard to the AMP technique, including a short femoral tunnel, blow out of the back wall of the lateral femoral intercondylar notch, and difficulty with visualization and graft passage [31]. Nevertheless, in the present study, the AMP technique was found to be superior to the TT technique in creating femoral tunnels within anatomical range, according to the radiological evaluation method of Illingworth. Illingworth confirmed with 3D computed tomography that a femoral tunnel angle greater than 32.7° (100% sensitivity and 85% specificity) on an anteroposterior radiograph of the knee and an inclination angle less than 55° (100% sensitivity and 87.5% specificity) on sagittal magnetic resonance imaging (MRI) determine whether the reconstructed ACL is within the anatomical range [20]. We consider this to be an easy and beneficial method to determine whether the reconstructed ACL is within the anatomical range.
Although evaluation of the functional outcomes based on IKDC and Lysholm scores and Tegner activity levels revealed higher values in the AMP group, significant differences between the groups were not observed. This result is similar to the results of other studies with more than a year of follow-up time [11, 29, 32, 33]. Conversely, there are studies with significantly higher IKDC and/or Lysholm scores following ACL reconstruction using the AMP technique [34]. As a result, no definitive evidence has been found to conclude that one technique is superior to the other in terms of functional outcomes based on scoring systems, such as the IKDC scoring system, Lysholm score, and Tegner activity level, in clinical studies [35].
Knee stability with respect to the ACL can be measured by the amount of anterior tibial translation identified using the Lachman and pivot-shift physical tests or using an arthrometer [34]. Although patients with TT ACL reconstruction obtain good anteroposterior stability, numerous biomechanical studies have demonstrated that the AMP technique restores the translational and rotational stability better and provides more anatomic graft placement [36-40]. In this study, anterior translation of the tibia was evaluated using both Lachman and pivot-shift tests, and no statistically significant difference was found between the groups. This finding may be due to the subjective nature of the tests. However, we performed stability tests at the last follow-up, which was at least two years after surgery.
Several clinical and biomechanical studies have demonstrated improved knee stability with the AMP technique, particularly during the first months [34, 38, 39, 41]. Earlier return to daily activities and jogging may be explained by the effect of the transverse orientation of the femoral tunnel and graft using the AMP technique on the early postoperative period. We speculate that increased rotational stability in the early period after surgery enables aggressive rehabilitation and faster recovery.
This study has certain limitations. First, this was a retrospective study with no randomization. Second, it was a short-term study and thus could not assess the long-term results. Third, we did not assess knee stability objectively. Future randomized clinical trials directly comparing both techniques over long-term follow-up will help to clarify which technique provides the best clinical outcome.
In conclusion, the AMP technique is significantly superior to the TT technique in creating anatomical femoral tunnel placement during single-bundle ACL reconstruction. There is no evidence to support the superiority of either technique in terms of clinical outcomes. However, the AMP technique provides faster recovery in terms of return to normal life and return to jogging in the short-term.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors thank Ibrahim Azboy, MD, for his contribution to this study.


