RESEARCH ARTICLE
Preoperative Periarticular Knee Bone Mineral Density in Osteoarthritic Patients Undergoing TKA
Yoshinori Ishii1, *, Hideo Noguchi1, Junko Sato1, Koji Todoroki1, Nobukazu Ezawa1, Shin-ichi Toyabe2
Article Information
Identifiers and Pagination:
Year: 2016Volume: 10
First Page: 396
Last Page: 403
Publisher ID: TOORTHJ-10-396
DOI: 10.2174/1874325001610010396
Article History:
Received Date: 2/2/2016Revision Received Date: 10/6/2016
Acceptance Date: 15/7/2016
Electronic publication date: 19/08/2016
Collection year: 2016

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution-Non-Commercial 4.0 International Public License (CC BY-NC 4.0) (https://creativecommons.org/licenses/by-nc/4.0/legalcode), which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Background:
Preoperative periarticular bone quality is affected by joint loading. The purpose of this study was to determine the periarticular bone mineral density of the knee joint of patients undergoing total knee arthroplasty, and whether the location of the load-bearing axis correlates with the measured bone mineral density.
Materials and Methods:
The bone mineral densities of the medial and lateral femoral condyles and the medial and lateral tibial condyles were analyzed in consecutive 116 osteoarthritic patients (130 knees) by dual energy x-ray absorptiometry.
Results:
The median bone mineral density values in the condyles were 1.138 in femoral medial, 0.767 in femoral lateral, 1.056 in tibial medial, and 0.714 in tibial lateral. The medial condyles showed significantly higher bone mineral densities than the lateral condyles in both the femur and tibia. In addition, the femoral medial showed significantly higher bone mineral density levels than the tibial medial, and the femoral lateral condyle had higher bone mineral density levels than the tibial lateral. The bone mineral density Medial/Lateral ratio was significantly negatively correlated with the location (tibial medial edge 0%, lateral edge 100%) of the load-bearing axis in the femur and tibia.
Conclusion:
Preoperative bone mineral density values may provide against the changes in bone mineral density after total knee arthroplasty by reflecting the correlation with joint loading axis. These results help explain why total knee arthroplasty has such good long-term clinical outcomes with a low frequency of component loosening and periarticular fractures despite a high degree of postoperative bone loss.
INTRODUCTION
The most common cause of revision arthroplasty is reported to be aseptic loosening [1], which occurs when the periprosthetic bone undergoes resorption. The quality of the osteotomized aspects of the subchondral trabecular bone during total knee arthroplasty (TKA) is considered to be the critical biological determinant for the fixation of components in the femur and even more so in the tibia. Measurements of bone mineral density (BMD) using dual energy x-ray absorptiometry (DEXA) allow the noninvasive, in vivo evaluation of the mechanical properties of the trabecular bone. Such measurements as well as the architecture of the trabecular patterns, enable the quantitative evaluation of the variations in bone biomechanical characteristics of the knee before a TKA procedure [2, 3].
The loss of peri-prosthetic bone after knee arthroplasty has been shown to adversely influence the migration of implants [3]. Despite this effect, the preoperative bone quality of the knee joint is not routinely assessed during pre-operative planning [4]. In addition, although joint loading is related to the periarticular BMD of osteoarthritic knee joints [5, 6], the normal subchondral bone remodeling appears to be deteriorated in the knees of patients with end-stage osteoarthritis (OA) undergoing TKA, as reported with early-stage OA [7]. Therefore, the purpose of the present study was to determine (1) the periarticular BMD of the knee joint of patients undergoing TKA, and (2) whether the location of load-bearing axis (LBA), which is related to joint loading, correlates with the measured BMD. The hypothesis of this study was that the periarticular BMD of the knee is higher on the load-bearing side and correlates with joint loading (i.e. the location of the mechanical axis) in patients undergoing TKA.
MATERIALS AND METHODS
The protocol for this study was approved by the Research Board of Healthcare Corporation Ashinokai, Gyoda, Saitama, Japan, and informed consent was obtained from all patients. One hundred sixteen primary OA patients (130 knees) undergoing TKA were evaluated. The mean age at the time of surgery was 71 years (range: 39-88 years). The pre-operative diagnosis for all patients was OA, and their clinical characteristics are summarized in Table 1.
| Parameter | Mean ± S.D. |
|---|---|
| Knees / Patients | 130 / 116 |
| Male (# of knees)/ Female (# of knees) | 13 (14) / 103 (116) |
| Mean age (years); [range] | 71 ± 8; [39–88] |
| BMI | 26 ± 4 |
| Pre-op. HSS Score | 43 ± 11 |
| Osteoarthritis Grade* | IV: 130 |
| LBR<50% / 50% ≤ LBR | 123 / 7 |
Measurement with DEXA
DEXA scans of the periarticular knee joint were acquired using a Lunar Prodigy densitometer (GE Medical Systems, Lunar, Madison, WI, USA) on the day before surgery. A single operator (K.T.) scanned all the knees. For the distal femur and proximal tibia scans, patients were laid in a supine position on a coach, and each knee in turn was positioned within a supportive brace allowing the patella to face upward. Patients who had flexion contracture were measured at their position of maximum knee extension.
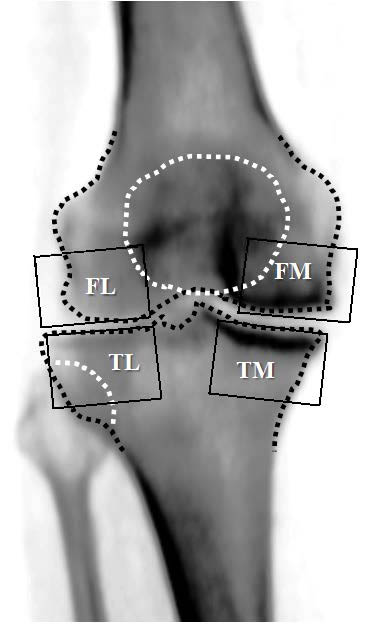
The Lunar Prodigy software was used to determine bone mineral content (g) and BMD (g/ cm2) for the proximal medial and lateral regions of interest (ROI) in both the femur and tibia. The BMD values of the femoral and tibial condyles were measured and are referred to as follows: medial femoral condyle: FM; lateral femoral condyle: FL; medial tibial condyle: TM; and lateral tibial condyle: TL. The height of each ROI was 2 cm below the joint line because the osteotomy during TKA surgery is usually performed within a depth of 2 cm. The external border of each ROI extended to the subperiosteal surface of the femur and tibia as determined manually by a single technician (K.T.). The patella served as the inner border for the medial and lateral proximal femoral ROIs, and the intercondylar eminences served as the inner border for the medial and lateral proximal tibial ROIs. In the femoral ROIs, care was taken to avoid including the patella in the measurement. In the lateral ROIs, care was also taken to avoid including the fibula in the measurement (Fig. 1). The medial-to-lateral BMD (BMD M/L) ratio was calculated by dividing the BMD in the medial ROI by the BMD in the lateral ROI in both the femur and tibia. The precision was calculated as the coefficient of variation (% CV) between scan BMD values. The precision of the measurements were 2.6% in FM, 5.5% in FL, 4.3% in TM, and 5.0% in TL.
Definition of the Load-bearing Mechanical Axis
Full-length load-bearing anteroposterior computed radiography (CR) images of the lower extremities were obtained before TKA. The mechanical axis was defined by a line connecting the center of the femoral head and the center of the ankle [9]. The load-bearing ratio (LBR) was calculated by measuring the distance from the medial edge of the proximal tibia to the point where the mechanical axis intersected the proximal tibia (tibial plateau level), and then dividing that measurement by the entire width of the proximal tibia and multiplying the ratio by 100%. Therefore, the percentage value can be negative (-) when the axis intersected more medially than the medial edge of the proximal tibia, and more than 100% when it intersected more laterally than the lateral edge.
Statistical Analysis
The BMD values in each condyle were compared using the Friedman test and Scheffé’s multiple comparison test. Spearman’s correlation of rank coefficients was used to evaluate the relationships between the BMD values in each condyle and between the BMD M/L ratio and the mechanical load-bearing axis. The strength of the correlation of the rank coefficients was defined as strong for values of 0.7-1.0; moderate for 0.4-0.7; and weak for 0.2-0.4. The BMD value is expressed using the median (25th percentile, 75th percentile). Statistical analyses were performed using SPSS software (ver. 14.0 J; SPSS, Tokyo, Japan). In all tests, p values less than 0.05 were considered statistically significant.
RESULTS
The median BMD values in the condyles were 1.138 (0.976, 1.287) in FM, 0.767 (0.647, 0.916) in FL, 1.056 (0.894, 1.216) in TM, and 0.714 (0.600, 0.843) in TL (Table 2). The medial condyles showed significantly higher values than the lateral condyles in both the femur and tibia (FM vs. FL: p<0.001; TM vs. TL: p<0.001). In addition, we found that the FM showed significantly higher BMD levels than the TM (p=0.009), and the FL had higher BMD levels than the TL (p=0.004).
| FM | FL | TM | TL | M/L Femur | M/L Tibia | |
|---|---|---|---|---|---|---|
| Median | 1.138 | 0.767 | 1.056 | 0.714 | 1.469 | 1.481 |
| 25 percentile | 0.976 | 0.647 | 0.894 | 0.600 | 1.269 | 1.326 |
| 75 percentile | 1.287 | 0.916 | 1.216 | 0.843 | 1.754 | 1.683 |
Strong correlations were found between the BMD levels in the FM and TM (p<0.0001, r=0.842), and between the FL and TL (p<0.0001, r=0.847). Additionally, a weak correlation was found between the BMD levels in the FM and FL (p<0.0001, r=0.364), and a moderate correlation was found between the TM and TL (p<0.0001, r=0.490).
In 123 out of the 130 knees (95%), the LBA passed through the medial side at the tibial plateau level (Tables 1 and 3). There were moderate, negative correlations between the BMD M/L ratio and LBR in the femur (p<0.0001, r=−0.408) and tibia (p<0.0001, r=−0.427) (Fig. 2a and b).
| LBR | LBR < 0 | 0 ≤LBR<50 | 50≤LBR<100 | 100≤ LBR |
|---|---|---|---|---|
| Number of knees | 84 | 39 | 5 | 2 |
DISCUSSION
Three important findings in the present study should be highlighted. First, the BMD levels were significantly higher in the medial than lateral condyles of the femoral and tibial bones. The main reason for this might be that the LBA of 95% of the knees studied here passed through the condyles at less than 50% of the tibial plateau level. Because OA usually develops first on the medial condyle, progressing to the lateral condyle as the condition worsens, our data support the conclusions of previous studies that reported a positive correlation between OA grade and BMD values [6, 10-13]. Second, the BMD values of the femoral sides were higher than those of the tibial sides. Because the femur is characterized by a convex geometry and the tibia by a concave geometry in this study, there may be anatomy- and geometry-specific bone characteristics that account for the differences in the BMD values between the femur and tibia. Third, the BMD M/L ratios in each femur and tibia in end-stage OA before TKA surgery were significantly correlated with the location of the LBA, confirming a previous report in osteoarthritic knees in various stage OA [5, 6].
 |
Fig. (2). The bone mineral density medial / lateral ratio and load-bearing ratio were moderately negatively correlated in both the femur (A) and tibia (B). |
The preoperative BMD values from patients undergoing TKA surgery were previously reported at the proximal femur and lumbar spine [4, 14-16]. In some cases, the periarticular BMD of the knee joint was evaluated on the femoral side [14, 17], the tibial side [15, 18-20], or on both sides [21-23]. The preoperative BMD values of the femur and tibia measured in the present study were within the range of previously reported values [12, 14, 15, 17-19, 22, 23] in the femur (0.512-1.70) and tibia (0.500-1.366). In addition, the BMD M/L ratio was also within the range of previously reported values [5, 6, 10] for osteoarthritic knee joints. Because there were significant correlations of the preoperative BMDs both between the femur and tibia for the medial and lateral compartments, and between the medial and lateral compartments for the femur and tibia, similar subchondral bone remodeling under various load-bearing conditions may occur in each compartment of the femur and tibia in each patient. Akamatsu et al. [10] also showed a significant positive correlation between the femoral and tibial condyles in 2 groups according to joint space narrowing in the following parameters: medial condyle BMDs, lateral condyle BMDs, and medial versus lateral condyle BMD ratios, supporting our results.
After TKA surgery, the postoperative BMD values are known to decrease, which is believed to affect prosthetic fixation. Such decreases in BMD were reported in the femur [17, 24], tibia [25-27], and in both sides [21, 22, 28]. Abu-Rajab et al. [28] demonstrated less reduction in bone density around the tibial component than around the femoral component. Levitz et al. [25] reported that eight years after TKA, there was a 36.4% decrease in tibial BMD, on average. Additionally, Petersen et al. [24] reported that BMD decreased by an average of 36% behind the anterior flange of the femoral prosthesis after only 2 years.
Despite of such large and faster decreases in BMD in the femur than in the tibia, periprosthetic fractures, such as supracondylar fractures of the femur, following TKA are not common. The higher preoperative BMD values in the femur than in the tibia indicated by the present study might play an important role in maintaining enough subchondral bone density to prevent component loosening and fractures around the component despite the rapid bone loss in the femur. We believe it is reasonable to think that the BMDs in the femur and tibia may approach similar values after TKA surgery.
Soininvaara et al. [29] reported similar medial and lateral BMD values in knees corrected for varus and valgus deformities due to bone remodeling after alignment correction through TKA. Additionally, Petersen et al. [20] reported that for tibial condyles in which the change in knee alignment indicated that the load was reduced postoperatively, a fast bone loss of 7-20% was seen during the first 6 months after surgery. A small, but significant increase in BMD of 2-7% was seen in tibial condyles in which the experienced load was increased after uncemented TKA. These studies, including our own, suggest that the bones become equally strong in both compartments of the metaphysis of the femur and tibia after TKA surgery. Such adaptation of the subchondral bone beneath each component may prevent clinical failures induced by the collapse of the trabecular bone. Soininvaara et al. [29] also concluded that the resultant equilibrium in bone density and strength potentially helps increase the longevity of TKA by creating more optimal loading conditions. In addition, Petersen et al. [20] concluded that a portion of the bone loss after TKA may represent a return to the normal, relatively high density arthritic bone that helps to make the long-term outcomes after TKA satisfactory, with a low revision rate and fractures of the proximal tibia rarely occurring.
Finally, considering that 123 out of the 130 knees (95%) showed less than 50% of the LBR passing through the tibial plateau level in this study, it is reasonable that the medial condyles of the femur and tibia had significantly higher BMD levels than the lateral condyles because joint loading may correlate with the periarticular BMD, as previously reported in both mild and severe osteoarthritic knee joints [5, 6]. The present study revealed that joint loading was correlated with the periarticular BMD of the knee joints of end-stage OA patients undergoing TKA. In addition, there was a significant correlation between the BMD M/L ratio in the femur and tibia and the LBR. Based on this data, orthopedic surgeons should consider, while performing TKA surgeries, that large differences in the load-bearing mechanical axis in the knee joint may indicate large differences in BMD values between the medial and lateral condyles, if the BMDs were not measured during pre-operative planning.
The LBR was positively correlated with the BMD M/L ratio of the femur and tibia before TKA surgery. Additionally, higher preoperative BMD values were found in the load-bearing side (i.e. the medial side in this study), while the femur showed larger and faster decreases in BMD than the unloaded side (i.e. the lateral side) and the tibia showed less loss. The distribution of preoperative BMD values reported in the present study may provide against the loss of BMD following TKA.
Several limitations of this study should be discussed. First, the results cannot be generalized to all osteoarthritis patients. Based on the results of LBR that over 95% of the patients showed less than 50%, most of them were the predominance of the varus knee with a few valgus knee. Second, because the height of each ROI reached to 2 cm below the joint line, variations in the degree of deformity of the condyles and in the level of the femoral and tibial scans at the time of measurement may have been sources of bias in this study. Third, the LBA was evaluated only with the coronal plane because of the study protocol. A three-dimensional approach using the load-bearing mechanical axes in both the anteroposterior and mediolateral directions would be more accurate for identifying the load distribution on the knee joint compared to a 2-dimensional approach using either individual axis [30]. Finally, because the evaluation of the BMD in the femur was performed 2 cm below the joint line in the coronal plane, no follow-up study can be performed to compare the pre- and post-operative BMDs, as is reported by most previous studies that were performed in the sagittal plane [14, 17, 21, 24, 28].
Despite these limitations, the strengths of the study include that we showed the preoperative periarticular BMD of knee joints including the osteotomized level, which is often considered to be the critical biological determinant for the fixation of components in the femur and tibia.
CONCLUSION
In conclusion, the results of the current study help explain why TKA has such good long-term clinical outcomes with a low frequency of component loosening and periarticular fractures despite a high degree of postoperative bone loss. The evaluation of the preoperative periarticular bone quality might be recommended during pre-operative planning before TKA routinely, since the quality of the osteotomized aspects of the subchondral trabecular bone during TKA is considered to be the critical biological determinant for the fixation of components in the femur and even more so in the tibia.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
This work was performed at Ishii Orthopaedic and Rehabilitation Clinic, Gyoda, Saitama, Japan.