All published articles of this journal are available on ScienceDirect.
Treatment Algorithm for Patients with Non-arthritic Hip Pain, Suspect for an Intraarticular Pathology
Abstract
Background:
The amount of patients referred with longstanding, non-arthritic hip pain is increasing, as are the treatment options. Left untreated hip dysplasia, acetabular retroversion and femoroacetabular impingement (FAI) may lead to osteoarthritis (OA). Finding the right treatment option for the right patient can be challenging in patients with non-arthritic hip pain.
Purpose:
The purpose of this study was to categorize the radiographic findings seen in patients with longstanding hip pain, suspect for an intraarticular pathology, and provide a treatment algorithm allocating a specific treatment option for each clinical condition.
Material and Methods:
A review of the literature was performed using Public Medline searches of MeSH terms combined with synonyms for femoroacetabular impingement, acetabular retroversion, periacetabular osteotomy and hip arthroscopy.
Results:
Radiographic findings associated with acetabular retroversion described in the literature were the crossover sign, the posterior wall sign and the ischial spine sign, while Wiberg’s lateral center-edge angle (CE-angle) together with Leqeusne’s acetabular index indicate hip dysplasia. A Tönnis index >2 indicates osteoarthritis, however unsatisfying results are documented following joint preserving surgery with a Tönnis index >1. Furthermore, ischial spine sign in combination with the posterior wall sign indicates total acetabular retroversion prone to periacetabular osteotomy in contrast to focal retroversion prone to hip arthroscopy. These findings were used creating a treatment algorithm for intraarticular pathologies in patients with longstanding hip pain.
Conclusion:
Based on the radiographic findings, the algorithm presented in this study can be a helpful tool in the decision-making for the treatment of patients with non-arthritic hip pain, suspect for intraarticular pathologies.
INTRODUCTION
Treating non-arthritic hip pain is of growing importance in clinic practice. There is increasing scientific interest in the pathoanatomy of the hip and in joint preserving surgical procedures.
In the Copenhagen City Osteoarthritis Sub-study (CCHS III) joint deformity was found in 62,4% of the male and 78,9% of the female study population [1]. A main category of these joint deformities is femoroacetabular impingement (FAI) caused by acetabular retroversion creating a Pincer-impingement (Fig. 1). The incidence rate in the general population for FAI and acetabular retroversion, which is believed to be a risk factor for hip arthritis [2, 3], is described to be 5%. However, in people with idiopathic osteoarthritis the incidence of acetabular retroversion is as much as 20% [4].
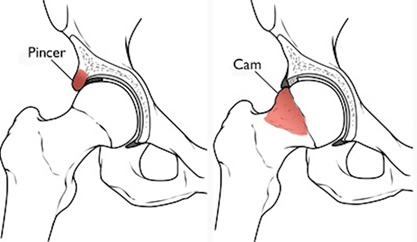
Several studies have shown that FAI and acetabular retroversion, if left untreated, leads to labral lesions, cartilage injuries and finally osteoarthritis [2, 5-7]. Treatment of this pathology is therefore of great interest.
The periactabular osteotomy (PAO) [2, 8-10] and arthroscopic rim trimming (HA) [8, 11-14] are two well-known surgical procedures in the treatment of non-arthritic hip pain caused by focal or global acetabular retroversion. The aim of both procedures is to reduce pain, reestablish a near-normal anatomy and there by delay the onset of secondary osteoarthritis. At 10 years follow up, the PAO has shown results of between 80-90% of hips still preserved, the remainder converted to total hip arthroplasty (THA). At 20 years the survival of PAO is more than 60% [15]. Follow-up of more than 4 years for HA has shown results of more than 90% of hips still preserved and less than 10% converted to THA [16]. As FAI is a common indication for both HA and PAO, deciding which surgical option to choose can be challenging.
The purpose of this article is to provide a helpful treatment algorithm for the selection of patients with FAI and acetabular retroversion for either PAO, HA, or total hip arthroplasty. This was done by critically reviewing the literature, thoroughly describing the radiographic findings and inclusion/exclusion criteria for HA and PAO.
METHOD AND MATERIAL
A critical literature search was performed using Public Medline (PubMed), where MesH-Terms were combined with all possible synonyms for periacetabular osteotomy and hip arthroscopy on June the 1st 2015. All abstracts were reviewed. Only articles in English were reviewed. Research on animals was excluded. All articles involving method of treatment, pre-operative symptoms, acetabular retroversion, radiological parameters, surgical indications and contraindications for PAO and HA were included. The radiographic signs of acetabular retroversion and hip dysplasia where thoroughly reviewed in the literature and described according to their association with the development of osteoarthritis and pain.
Findings and Discussion
47 articles in English regarding acetabular retroversion and/or PAO or HA in humans were reviewed based on the literature search. Included were three systematic reviews; one randomized controlled trial, two comparative studies, and 13 reviews. 10 articles were included for the description of radiographic findings.
Radiographic Signs and Technique
Retroversion of the acetabulum can be difficult to see on a radiograph and it might be over- or underestimated if a standardized technique is not used. A correct anterior-posterior (AP) radiograph is taken with the patient in an upright standing position [17]. Using the technique described by Tannast et al. neutral pelvis tilt and rotation can be achieved [18].
Different radiographic signs, such as the center-edge-angle (CE), crossover sign (COS), posterior wall sign (PWS), ischial spine sign (ISS) and the acetabular index (AI) can be used to evaluate if acetabular retroversion is present. These radiographic findings are shown in Figs. (2 and 3).
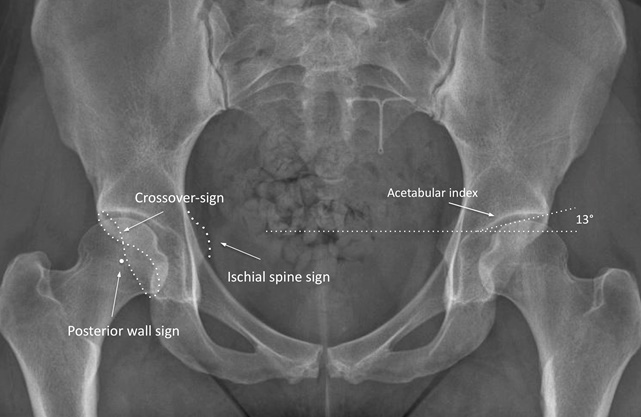
The crossover sign (COS) has been associated with acetabular retroversion [19, 20]. It can be seen on an AP pelvic radiograph when the most proximal anterior acetabular rim appears lateral to the posterior rim, creating a figure eight sign (Fig. 2). Nicolas J. et al. [21] showed that the crossover sign has a sensitivity of 96%, a specificity of 95%, a positive predictive value of 90% and a negative predictive value of 98% to detect acetabular retroversion. Furthermore, the crossover sign in itself is associated with the development of osteoarthritis as shown in a study of 131 patients with idiopathic osteoarthritis where a chi square analysis revealed that there is an association between the radiographic appearance of acetabular retroversion and hip osteoarthritis (p < 0.005) [21].
The ischial spine sign (ISS) is also associated with acetabular retroversion and commonly found when a positive crossover sign is present [22]. It is seen when the ischial spine is projected into the pelvic cavity on an AP pelvic radiograph (Fig. 2). The presence of the ischial spine sign as a predictor of acetabular retroversion has a sensitivity of 91%, a specificity of 98%, a positive predictive value of 98% and a negative predictive value of 92% [22].
The posterior wall sign (PWS) is another sign of acetabular retroversion [20]. It is visible when the projection of the posterior wall of the acetabulum descends medially to the center of the femoral head instead of laterally as seen normally (Fig. 2).
All three radiographic signs mentioned above are indications for acetabular retroversion, which has been associated with the development of osteoarthritis [21, 23].

Wiberg’s lateral center-edge angle (CE) describes the acetabular coverage of the femoral head [24]. The center-edge angle is formed by a line drawn from the center of the femoral head to the outer edge of the acetabular roof, and a vertical line drawn through the center of the femoral head (Fig. 3). It is considered normal between 25-39 degrees [24, 25]. Reduced coverage <25 degrees indicates hip dysplasia, which is associated with the development of osteoarthritis of the hip [24, 25].
The acetabular index (AI) as described by Lequesne [26] describes as well the acetabular coverage of the femoral head. The acetabular index is the angle formed by a horizontal line and a line connecting the medial point of the sclerotic zone with the lateral center of the acetabulum. It is normally zero or negative and an angle of more than 10 degrees is an indication of hip dysplasia [26] (Fig. 2).
Both the acetabular index as well as the center-edge angle can be used to detect hip dysplasia, which is associated with the development of osteoarthritis. Wiberg’s study of 44 patients aged 13 to 60 years with CE-angle in the pathologic range developed osteoarthritis within the 4- to 28-year follow-up period [24]. Another study by Cooperman et al. [25] was not able to show the direct association between CE-angle and osteoarthritis but most of the 32 hips with CE-angles less than 20° developed osteoarthritis within the 22 years they were followed [25].
The Indications and Contraindications For PAO and HA Because of Acetabular Retroversion
At this time, no comparative studies are described in the literature between PAO and HA.
PAO
The indications for PAO because of acetabular retroversion are: Clinical symptoms such as general groin pain and a positive impingement test. Radiological signs of acetabular retroversion such as: a positive crossover sign and a positive posterior wall sign. Additionally the ischial spine sign is a radiographic sign of retroversion of the acetabulum [2]. The global retroversion of the acetabulum, in contrast to the focal over-coverage or retroversion, is an indication for the treatment with PAO [3, 27].
Contraindications for PAO in patients with global acetabular retroversion are: osteoarthritis and age above 50 years. Osteoarthritis can be graded from a plain radiograph or an MRI as a Tönnis grade from 0-3 (0 being no osteoarthritis and 3 being severe osteoarthritis with cysts, joint space narrowing and deformity of the femoral head). Tönnis grades 2-3 are contraindicative for PAO since the conversion to total hip arthroplasty is almost inevitable within a short time [7, 28-30]. In patients over 40 years of age PAO has shown suboptimal if in combined with radiographic pre-arthritic findings [3, 31]. The indication for PAO in the age group between 40 and 50 years of age is therefore relative and depends on motivation in the patient for PAO and Tönnis grade 0. Furthermore, a lack of congruence of the joint as for instance a deformity of the femoral head will also result in a worse outcome post-operatively [3].
HA
The indications for HA in individuals with acetabular retroversion are: Clinical symptoms of hip and groin pain under physical activity, limited range of motion and a positive impingement test. Radiographic signs of FAI as a positive crossover sign and signs of labral and/or cartilage lesions in the MRI [8, 11, 32, 33]. A focal over-coverage or retroversion can be treated by HA whereas global retroversion of the acetabulum has to be approached with caution due to the possible risk of causing iatrogenic hip instability [8, 33].
As for PAO it is essential to evaluate the hip joint pre-operatively. Signs of hip osteoarthritis such as a Tönnis grade of 2-3 [7, 28-30] or joint space narrowing by 50% are contraindications of HA [33]. Furthermore, there is a steep learning curve for HA and the experience of the surgeon is therefore an important factor for the post-operative result, too [33].
Treatment Algorithm
Based on the above-mentioned indications and contraindications for PAO and HA, the algorithm suggested in this article may use as a helpful tool in identifying the different hip pathologies and their respective treatment options (Fig. 4). However, It is essential to understand, that this algorithm is mainly based on radiographic findings. The decision for surgical treatment and the proper procedure has to be made individually by the treating physician.
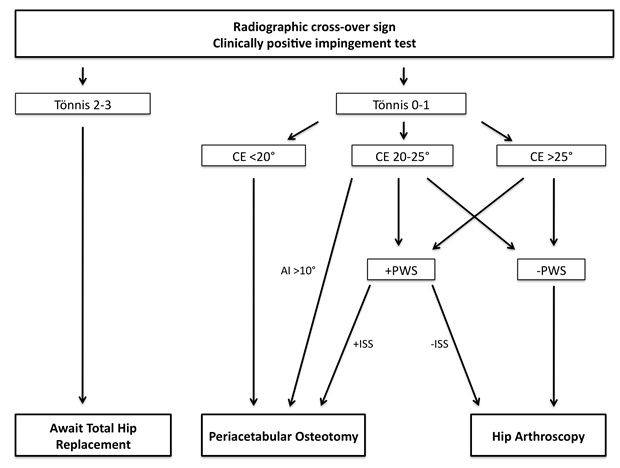
The algorithm is based on the work of Peters et al. [10] and shows patients observed with acetabular retroversion and a clinically positive impingement test. The acetabular retroversion is seen on a plain anterior-posterior radiograph as a crossover sign (Fig. 2). As seen in the findings above, Tönnis grades 2-3 is a contraindication for both the PAO and HA. This pre-operative finding has proven to be strongly associates with failure and conversion to total hip arthroplasty within a short period of time [7, 34].
Hips with a reduced acetabular coverage with a CE-angle <20° are considered dysplastic [24] and PAO is the golden standard of treatment in these cases [35].
For patients with a CE-angle of 20-25° it is important to evaluate the acetabular index together with the posterior wall sign. Patients with a CE-angle of 20-25° and an acetabular index of over 10° and can be considered for PAO due to the presence of dysplasia [26]. For patients with an acetabular index of less than 10° and a CE-angle of 20-25° it is important to evaluate signs of acetabular retroversion, and if positive, consider a PAO. Patients with a CE-angle of 20-25° and no other sign of global acetabular retroversion can be treated successfully with HA.
Patients with a CE-angle over 25° and no signs of acetabular retroversion can be treated with HA [36].
During the arthroscopic rim trimming it is important to keep in mind the possibility of iatrogenic hip dysplasia and instability. Patients with a CE-angle of 20-25° are at risk and should be operated based on the following equation:
Change in CE-angle = 1.8 + (0.64 x Rim Trimming in The 12 o’clock Position in Millimeters) [32].
Patients continuously experiencing hip pain following PAO, may suffer from co-existing intraarticular pathologies such as labral injuries, cartilage damage and/or bony deformities such as CAM-impingement with successfully can be treated by HA.
Limitations
Because of the spares literature regarding the treatment of acetabular retroversion by PAO or HA this article only focuses on the presence or absence of certain radiographic signs such as the posterior wall sign, ischial spine sign, etc. The degree of posterior coverage, which is important for the stability of the hip and thereby the decision of the treatment, is not elaborated. It is therefore relevant with further studies documenting the effect of different degrees of pre-operative posterior coverage on the results of PAO and HA on a long-term basis.
In contrast to PAO with a documented follow-up period of nearly 20 years, hip arthroscopy is a relatively new treatment and the follow-up period rather short. And although literature shows promising results, both functionally and clinically, after HA for FAI within the first years post-operatively [12, 37], long-term studies are needed. Furthermore it is also important to recognize that the cause of the hip pain might lie outside the hip joint itself, even though the radiological signs suggest acetabular retroversion, CAM- or Pincer-impingement.
CONCLUSION
PAO and HA are well-documented techniques in the treatment of non-arthritic hip pathologies, however indications for both procedures are rather similar. The algorithm presented in this article may provide a useful tool in the triage and treatment of patients with non-arthritic hip pain. Further studies are warranted.
LIST OF ABBREVIATIONS
| AI | = Acetabular index |
| CE-angle | = Center-edge angle |
| COS | = Crossover sign |
| FAI | = Femoroacetabular Impingement |
| HA | = Hip arthroscopic rim trimming |
| ISS | = Ischial spine sign |
| OA | = Ost eoarthritis |
| PAO | = Periacetabular Osteotomy |
| PWS | = Posterior wall sign |
| THA | = Total Hip Arthroplasty |
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


