All published articles of this journal are available on ScienceDirect.
Emergency Soft Tissue Reconstruction Algorithm in Patients With Open Tibia Fractures
Abstract
Introduction:
Tactic of emergency closing of soft tissue defect allows to significantly improve the treatment results concerning patients with severe open fractures. However, a number of certain factors make the implementation of this tactic rather difficult. Injured people’s unstable conditions are mong these crucial factors which include, polytrauma in lots of cases, absence of exact recommendations for recovery terms, choice of definite tissue flaps and a type of circulation.
The Aim of Study:
is to develop exact, usable and in practice algorithm of emergency reconstruction of leg soft tissues in patients with severe open tibia fractures, based on the usage of the most foolproof and simple methods.
Data (Patients) and Methods:
85 patients with open tibia fractures complicated by soft tissue defects were included in our study. Patients were divided into two groups. The control group consisted of 56 patients. Soft tissue reconstruction in this group was provided without an exact algorithm, after continuous attempts on local healing. After analyzing the treatment process and the treatment results we have developed the algorithm of emergency soft tissue reconstruction. It was used in 29 patients (the study group). This algorithm allows choosing optimal timing for tissue reconstruction and appropriate method to be applied, depending on the patient’s condition, the mechanism of soft tissue defect formation, and its square and localization.
Results:
We observed a statistical decrease in deep wound infection frequency, partial tibia necrosis frequency, chronic osteomyelitis frequency, duration of hospitalization in patients with severe open tibia fractures because of using our algorithm.
INTRODUCTION
The treatment of patients with open tibia fractures complicated by soft tissue defects is one of the most difficult problems in plastic and reconstructive surgery and emergency orthopedic surgery. We should emphasize a high frequency of amputations, deep wound infection and nonunion after these injuries [1, 2]. The implementation of the concept of emergency soft tissue reconstruction allows considerable decrease in the frequency of complications [3, 4]. Results of this tactic implementation are remarkable, but, in spite of this, it has not become widely applicable [5]. Besides purely managerial issues, such as the absence of communication between plastic and orthopedic surgeons, there are certain objective difficulties, preventing this method from being introduced. A wide application of emergency soft tissues reconstruction after severe open fractures is obstructed by different opinions about wound closing time and necessity of graduated debridement, especially if necrosis develops in several days after a trauma [6-8]. Early closing of soft tissue defects is obstructed by selecting the the flap with particular type of blood circulation and type of tissue which are not exact and these published recommendations are hard to follow in emergency surgery [9-12]. Other complicated questions of emergency soft tissue reconstruction in patients with open tibia fractures are general conditions and presence of polytrauma in 30% of these patients, complicating the implementation of emergency reconstructive operations and in some cases rendering it dangerous for patient’s life [13, 14]. In these cases, we have to use the most foolproof and simple methods of reconstruction [15].
The hypothesis of the study is that the development of exact recommendations of choosing the time and methods of the soft tissue reconstruction in dependence of severity of general condition, square and localization of soft tissue defect of leg after severe open tibia fractures allows to improve the results of treatment greatly in this difficult group of patients. The aim of our study is to develop an exact and easy-to-use algorithm of soft tissue reconstruction for a practical application in patients with severe open tibia fractures, which would be based on most of the simple and foolproof methods for emergency surgery usage.
CLINICAL CASES AND METHODS
85 patients with open tibia fractures complicated by soft tissue defects were included in our investigation. The division of patients by sex and age is shown in Table 1. In the text we only mention the fact that most of them were working-age males. The patients’ division by a type and localization of leg fracture is shown in Table 1. A primary defect, developed by crashing soft tissues in the fracture location is observed in 32 (37.6%) patients. A secondary defect developed by disruption of blood circulation and necrosis of tissues was observed in 53 (62.4%) patients. A polytrauma was diagnosed in 28 (32.9%) patients. Only one third of the patients with open tibia fractures complicated by soft tissue defects were hospitalized in a stable condition, according to the Pape- Krettek classification [16]. The other two thirds of patients were hospitalized in border, unstable or critical conditions.
Characteristics of patients.
| All patients Quantity (percent) |
Study group Quantity (percent) |
Control group Quantity (percent) |
P (comparison between two groups) | |
|---|---|---|---|---|
| Division by age | ||||
| 18-30 | 29 (34.1%) | 10 (34.5%) | 19 (33.9%) | 1 |
| 31-45 | 30 (35.3)% | 9 (31.0%) | 21 (37.5%) | 0.64 |
| 46-60 | 17 (20%) | 6 (20.7%) | 11 (19.6%) | 1 |
| 60 + | 6 (7.1%) | 4 (13.8%) | 2 (3.6%) | 0.17 |
| Division by sex | ||||
| Males | 70 (82.4%) | 25 (86.2%) | 45 (80.4%) | 0.56 |
| Females | 15 (17.6%) | 4 (13.8%) | 11 (19.6) | |
| Severity of fracture by Gustillo-Anderson | ||||
| IIIA | 38 (44.7%) | 9 (31%) | 29 (51.8%) | 0.106 |
| IIIB | 40 (47.1%) | 16 (55.2%) | 24 (42.9%) | 0.36 |
| IIIC | 7 (8.2%) | 4 (13.8%) | 3 (5.4%) | 0.22 |
| Localization of injury | ||||
| Upper third | 10 (11.8%) | 2 (6.9%) | 8 (14.3%) | 0.48 |
| Middle third | 50 (58.8%) | 18 (62.1%) | 32 (57.1%) | 0.81 |
| Lower third | 21 (24.7%) | 7 (24.1%) | 14 (25%) | 1 |
| Polytrauma | 28 (39.2%) | 11 (37.9%) | 17 (30.4%) | 0.62 |
| Condition during addmission | ||||
| Stable | 28 (32.9%) | 8 (27.6%) | 20 (35.7%) | 0.47 |
| Border | 33 (38.8%) | 13 (44.8%) | 20 (35.7%) | 0.48 |
| Unstable | 22 (25.9%) | 7 (24.1%) | 15 (26.8%) | 1 |
| Critical | 2 (2.4%) | 1 (3.4%) | 1 (1.8%) | 1 |
The patients included in the study were divided into two groups. There were no statistically significant differences between control and study group by age, sex, localization and severity of injury, general condition and polytrauma frequency. The control group consisted of 56 patients with open tibia fractures complicated by soft tissue defects. The tactic of treatment was selected by a surgeon according to his experience and the subjective criteria. Most of the surgeons choose a waiting tactic and closing of wound in late time after continuous attempts of topical conservative wound treatment. If necrosis of soft tissues manifested after several days of trauma, staged debridement with topical wound treatment by VAC and hydrogel dressing were provided. The wounds were closed by flap if there was a failure of topical wound treatment. Methods of soft tissue reconstruction are shown in Table 2 in detail.
Methods of soft tissue reconstruction.
| Methods of soft tissue reconstruction | Study group Quantity (percent) |
Control group Quantity (percent) |
|---|---|---|
| Secondary wound healing | - | 7(12.5%) |
| Split thickness skin graft | - | 7(12.5%) |
| Closing by flap | 29 (100%) | 42 (75%) |
| Closing by fasciocutaneous flap | 3 (10.3%) | 14 (12.5%) |
| Medial fasciocutaneous flap of leg | 1(3.4%) | 6(10.7) |
| Lateral faciocutaneous flap of leg | - | 2 (3.6%) |
| Sural flap | 1(3.4%) | 6 (10.7%) |
| Free radial flap | 1 (3.4%) | |
| Closing by muscule flap | 26 (89.7%) | 28 (50%) |
| Local soleus flap | 19 (65.5%) | 12(21.4%) |
| Local gastrocnemius flap | 2 (6.9%) | 4(7.1%) |
| Free latissimus dorsi frap | 3 (10,3%) | 9 (16,1%) |
| Free anterolateral flap | 1 (3.4%) | 2 (3.6%) |
| Free serratus anterior flap | 1(3.4%) | 1(1.8%) |
In the study group (29 patients), we have used the developed algorithm of emergency soft tissue reconstruction (Fig. 1).
If there was a primary soft tissue defect, the tactic of reconstruction depends on the severity of the patient’s general condition. In a stable condition, we preferred the primary reconstruction in the first hours after the admission. In a border condition, we thought that it is possible to use a local flap during the primary operation. A careful observation of vital functions is necessary. In an unstable condition, we closed the defect in a delay of 4-5 days, when the patient’s condition became stable or border. According to our algorithm, it is necessary to fulfil a leg soft tissues reconstruction in up to 15 days after the trauma.
If there was a delayed soft tissues necrosis in the fracture region, we performed an early full debridement in a period of up to 10 days after the trauma with a simultaneous closing of a secondary defect by a flap.
To choose the optimal flap for closing leg’s soft tissue defects, we developed a scheme, in which the leg is divided into 5 levels (Fig. 2). The extension of the level is equal to the width of the patient’s hand on the level of heads of metacarpal bones. If the defect’s square is less than 0.5% of the total square of the body / BSA (body surface area) (1/2 of palmar square of patient’s hand), it is possible to use local flaps. If the defects square is more than this, it is necessary to use free flaps. We thought that usage of muscular flaps is preferred because of good antiinfection activity. A fasciocutaneous flaps application is a reserved method. We used it if the usage of muscular flaps was impossible, due to the patient’s severe general condition of, along with severe atherosclerosis of blood vessels. The scheme of the treatment method choice for every level of a leg is shown in Table 3.
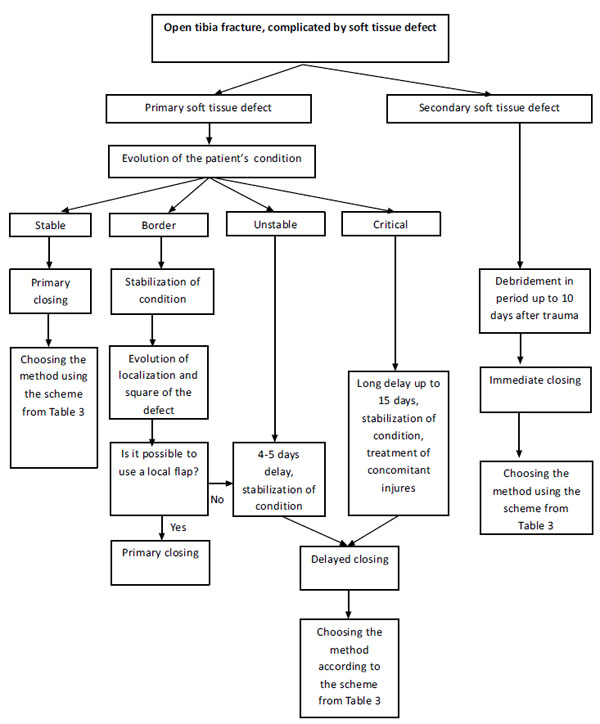
Emergency leg soft tissues reconstruction algorithm.
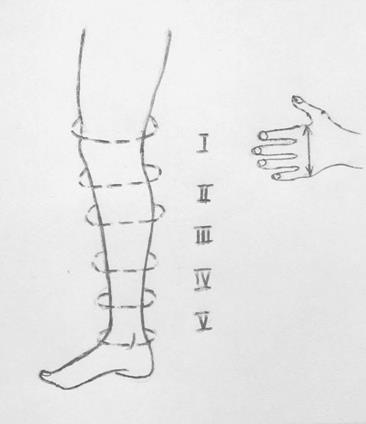
Division of a leg in levels.
Choosing the method of a leg’s soft tissue reconstruction.
| Level of a leg | Defect within one level (not a large defect) | Defects including more than one level (a large defect) |
|
|---|---|---|---|
| Basic method | Reserve method | ||
| I | Flaps from lateral and medial heads of gastrocnemius muscle | Free muscular flaps | Free muscular flaps |
| A medial and lateral fasciocutaneous flap of a leg | |||
| II | Flaps from the medial half of soleus muscle | ||
| III | |||
| A sural fasciocutaneous flap | |||
| IV | Free muscular flaps | ||
| V | |||
Results in the control group were evaluated retrospectively, in the study group-prospectively. We evaluated the frequency of amputations, the necrosis of flap, that had to be operated on, the frequency of deep wound infection and the hospital treatment duration, including repeated hospitalizations. We analyzed the frequency of chronic osteomyelitis and nonunions of tibia. We provided a statistical examination of the difference of qualitative values by Fisher criteria, quantitative values by Student’s criteria.
RESULTS
The developed algorithm allowed us to reconstruct leg soft tissues on the average in 5.14 days after trauma. In the control group, the period was 44.8 days. Muscular flaps were used in 89.6% of patients of the study group (in 10.4% we used fasciocutaneous flaps), according to the developed scheme. In the control group, muscular flaps were used in 50% оf patients. The detailed data concerning the flaps used in our study are shown in Table 2.
The amputation on the level of the upper third of a leg was performed in 1 patient in the control group because of severe deep wound infection. There were no amputations in the study group.
Evaluating the deep wound infection frequency, we should note a major difference between the study group and the control group (10.34% against 42.82%). This difference is statistically significant.
We observed a significant lowering of the segmental tibia necrosis frequency, while using the emergency soft tissue reconstruction algorithm (13.79% in the study group, 50% in the control group).
We noticed a statistically significant lowering of hospitalization duration, while using the developed algorithm (54.82 days in the study group, 91.16 days in the control group).
Processing the follow-up results in the treatment, we noticed the lowering of nonunions frequency, but it was not statistically significant (31.01% in the study group, 42.82% in the control group). We should mark statistically significant lowering frequency of chronic osteomyelitis, while implementing the algorithm of emergency leg’s soft tissues reconstruction (13.89% in the study group, 53.5% in the control group). The comparison of the treatment results in the study group and the control group is shown in detail in Table 4.
Comparison of the treatment results.
| Study group | Control group | P | |
|---|---|---|---|
| Flap necrosis, quantity (percent) | 7 (24.1%) | 15 (26.8%) | 1 |
| Deep wound infection, quantity (percent) |
4 (13.8%) | 24 (42.9% | 0.0076 |
| Necrosis of the tibia segment, quantity (percent) |
3 (10.3%) | 28 (50%) | 0.0003 |
| Duration of hospital treatment, days | 59.96+/-7.15 | 104.92+/-9.08 | 0.0003 |
| Nonunion, quantity (percent) |
7 (24.1%) | 25 (44.6%) | 0.097 |
| Chronic osteomyelitis, quantity (percent) |
5 (17.2%) | 30 (53.6%) | 0.0012 |
We have included two clinical cases from the study group.
Clinical Case 1.
Patient G, a 47 years old (Fig. 3), injured in a car crush. Diagnosis at hospitalization: Polytrauma ISS 18 points. Open craniofacial trauma. Brain contusion with a middle degree of severity. Extensive lacerated wound of the head. Open tibia fracture in the middle third in the right leg IIIb type by the Gustillo-Andersen classification. The patient was admitted in a border condition. Intensive care was provided and an operation was performed after a preparation of the patient in 4 hours. The operation was debridement of the head and leg wounds, along with a fracture fixation by an external fixator. We performed closing of the soft tissue of the III level defect, comprising 0.5% BSA (body surface area) of the leg by flap from the medial half of soleus muscle. In 15 days, we performed closing of a muscular flap surface by a split-thickness skin graft. In 24 days after trauma, we removed the external fixator and prepared a fracture fixation by a locked nail. The wounds were healed without any complications. The patient was discharged from hospital in 43 days after trauma. The fracture was healed in 6 months after trauma. The patient then returned to work.
Clinical Case 2
Patient D, 34 years old (see Fig. 4). Injured in a car crash (a car driver). The patient was brought to our hospital in 2 hours after trauma. Diagnosis: an open tibia and fibula fracture in the lower third IIIB type by Gustillo-Andersen classification. The patient was admitted in a stable condition. We performed a debridement of the wound and a fixation of the fracture with an external fixator. There was a soft tissue defect in the IV and V levels of the leg, 1% of BSA (body surface area), because of this we performed closing with a free anterolateral flap. Covering of the muscular flap by a split thickness skin graft was performed in 13 days after trauma. Removing the external fixator and posteosytesis by a plate was performed in 32 days after trauma. The wounds healed without complications. The patient was discharged from hospital in 53 days after trauma. The fracture healed in 5 months. The patient resumed working as a driver.
DISCUSSION
Soft tissues that surrounded the fracture play the most important role in the processes of infection eradication and fracture consolidation in patients with severe open tibia fracture [17]. Soft tissue reconstruction is the clue stage in treatment of such patients [1, 3]. Because of this (like terms and methods of fracture fixation) the systematic tactic for choosing terms and methods of soft tissue reconstruction in patients with severe open tibia fractures (an algorithm of emergency soft tissue reconstruction) is very important.
We agree with Gopal (2000), that results are better when the reconstruction is performed earlier [4] if there was a primary soft tissue defect (developed at the moment of injury due to the skin and subcutaneous fat crashing) in patients with severe open tibia fractures. There is another opinion in publications that it is necessary to delay the soft tissue reconstruction up to 4-5 days [5]. During this time, the border between necrotic and vital tissues becomes clearly visible, and staged debridement in this period allows cleaning the wound. Nevertheless, we think, that it is possible to perform a full cleaning of the wound as a primary operation. The open wound leads to additional loss of tissues due to drying and contamination with high pathogenic hospital bacteria strains [18]. Because of it, the soft tissue reconstruction in the earliest possible time is the priority in our algorithm.
An open tibia fracture complicated by a soft tissue defect is developed by a high energy mechanism of trauma in most cases. In a stable condition, when an immediate reconstruction of leg soft tissues is possible, only one third of victims are admitted to hospital. Nearly 30% of patients with severe open tibia fractures have concomitant injuries [13]. In these cases, the modified scheme of Pape-Krettek is the basis of our algorithm. The delay of not more than 4-5 days is optimal and not more than 15 days is a deadline of the period, during which a soft tissue reconstruction in a patient with a severe open tibia fracture has to be performed. It must be done before the development of severe wound infection and tibia segment necrosis [16].
Some authors consider a soft tissue reconstruction with a flap is not appropriate for polytrauma patients, and in such cases, it is necessary to make an acute limb shortening followed by a limb elongation in an Ilizarov’s device during the next stage of treatment. However, the major duration of treatment and a high frequency of complications (two in one patient on average) make these methods be reserved only for the most severe cases [14].
In our clinic, we attempt to standardize the most foolproof flap choosing depending on a square and a localization of a soft tissue defect. Such attempts took place earlier, but the schemes were very complicated or only one type of flap was used (fasciocutaneous) [12], or they required calculating the square of defect additionally, that is not possible in emergency care [9]. Being a part of the algorithm, our scheme allows to make decisions concerning a local usage of free flaps depending on a square and a localization of a soft tissue defect. If it is possible to use local flaps, the scheme allows choosing the basic or reserve method of soft tissue reconstruction.
The local muscular flaps is a basic method of closing small defects of a leg in our algorithm. We explain this by certain reasons. First, muscular tissue has a very high osteogenic potential. It was the source of blood vessels and according to some data stromal cells and mediators of growth for growing and remodeling bone tissue [19]. Second, usage of local muscular flaps requires lower operation time as well as lower duration of hospital stay, it does not require a careful control of blood circulation in the flap in postoperative period [20]. Yet there is an opposite opinion stated in some publications emphasizing necessity to use free muscular flaps for closing even small soft tissue defects in patients with open tibia fractures [21]. Authors explain it by the fact that local tissues of a leg are compromised by a high energy trauma mechanism and their usage for defect closing is not effective. In our algorithm, free muscular flaps have to be used when the defect square is more than 0.5% of BSA (body surface area). Their usage is considered the “gold standard” for many years and it has been associated with minimal rate of complications. However, recently some data about the same effectiveness of free fasciocutaneous flap in patients with open fractures and chronic osteomyelitis have been published [11, 22]. Better esthetic appearance of limb, development of full thickness coverage (skin and subcutaneous fat) over the zone of injury, better stability of flap tissue for the second operation are the advantages of free fasciocutaneous flaps usage.
Using the algorithm developed in our clinic (the algorithm of emergency leg soft tissue reconstruction in patients with severe open tibia fractures), we obtain results which are consistent with the results of other studies in frequency flap necrosis and frequency of wound infection (see Table 5) [3, 4, 8, 12, 23]. The stated above proves the standardized approach (algorithm) of treatment patients with severe open tibia fractures to be effective and allow to decrease significantly the complication rate and to improve the treatment results.
Comparison of different author’s treatment results.
| Author | Number of patients | Time of defect closing | Frequency of flap necrosis | Frequency of deep wound infection | Duration of hospital stay |
|---|---|---|---|---|---|
| Godina 1986 | 532 | to 72 hours | 0.75% | 1.5% | 27 |
| from 72 hours to 3 months | 12% | 17.5% | 130 | ||
| more than 3 months | 9.5 | 6% | 256 | ||
| Gopal et al. 2000 | 63 | to 72 hours | - | 3% | |
| 11 | more than 72 hours | - | 19% | - | |
| Hou et al. 2011 | 34 | 10.9 days | 14.8% | 34% | - |
| Kamath et al. 2012 | 94 | to 10 days | 4.2% | 17% | - |
| 38 | from 10 days to 6 weeks | 18.4% | 55.3% | - | |
| 19 | more than 6 weeks | 15.8% | 38.6% | - | |
| Chua et al. 2014 | 30 | to 72 hours | 20% | 27% | 31.4 |
| 59 | more than 72 hours | 9% | 63% | 55.8 |
The limitation of the study is that the number of patients is not large (29 in study group and 56 in control group) and that results in control group were obtained in retrospective manner, but in study group was obtained in prospective manner. Evidence level III.
CONCLUSION
The algorithm developed in our clinic implemented in emergency leg soft tissue defect closing in patients with severe open tibia fractures helps to choose the time of soft tissue reconstruction depending on severity of the patient’s general condition and mechanism of soft tissue defect development. The algorithm allows choosing the method of reconstruction depending on localization and square of an injury zone. This complex of treatment options usage allows decreasing the time from an injury to soft tissue reconstruction, decreasing the frequency of deep wound infection, nonunion of tibia, chronic osteomyelitis, as well as the duration of hospital treatment of patients with severe open tibia fractures.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.











