All published articles of this journal are available on ScienceDirect.
Preoperative Determinants of Patient-reported Pain and Physical Function Levels Following Total Knee Arthroplasty: A Systematic Review
Abstract
Background:
A sound knowledge of the determinants of total knee arthroplasty (TKA) outcomes could help in patient selection, preparation and education. We aimed to assess the current status of the literature evaluating preoperative determinants of early and medium term patient-reported pain and disability following TKA.
Method:
A search in Medline, Pubmed, Embase and CINAHL until October 2014 was undertaken. Selection criteria included: 1- participants undergoing primary unilateral TKA with a follow-up from 6 months to 2 years, 2- validated disease-specific patient-reported outcome measures assessing pain and/or function used as outcome measure and 3- identification of preoperative determinants obtained via multivariate analyses. Risk of bias was assessed using a modified version of the Methodology checklist for prognostic studies.
Results:
Thirty-three prognostic explanatory studies were included. Mean total score of the methodological quality was 80.7±12.2 %. Sociodemographic and psychosocial determinants included greater socioeconomic deprivation (both studies), greater levels of depression and/or anxiety (7 out of 10 studies) and greater preoperative pain catastrophizing (all 3 studies). Significant clinical determinants included worse pre-operative knee related pain or disability (20 out of 22 studies), presence or greater levels of comorbidity (12 out of 23 studies), back pain (4 out of 5 studies) and lower general health (all 11 studies).
Conclusion:
Several significant determinants of short to medium-term pain and functional outcomes following TKA have been summarized by studies with moderate-to-high methodological quality. No conclusions can be reached regarding the strength of the associations between significant determinants and TKA results because of heterogeneity of study methodologies and results. Further high-quality research is required.
INTRODUCTION
Total knee arthroplasty (TKA) is a common procedure intended at treating patients with knee osteoarthritis (OA) suffering from pain and disability [1]. Its predominant success rendered it the second most common type of orthopaedic intervention [2]. This tendency will likely maintain, as projections suggest a six-fold increase in the number of primary TKAs performed in the next decades [2]. Although TKA is generally a successful intervention, leading to amelioration in pain levels and functional status, it yields suboptimal results in up to one third of patients [3-7]. Sound knowledge of determinants of TKA outcomes can help in patient selection, preparation and education, especially regarding possible risks and benefits of the procedure [8]. This is particularly relevant with respect to medium-term outcomes, as after a significant amelioration three to six months postoperatively, pain and physical function levels vary little subsequently until two years following surgery [9, 10]. During this time, patients are closely monitored by their surgeons, and the medical treatment and rehabilitation can be readily altered if progress is deemed unsatisfactory.
Previous systematic reviews attempted to summarize the determinants of TKA outcomes. Santaguida et al. (2008) identified older age and female gender to be associated with worse function following TKA [8]. However, their results are based on studies published until 2001. Van Jorbegen et al. (2014) focused on protective determinants of anterior knee pain following TKA, and their findings included mostly surgical factors, namely femoral components with a posterior centre of rotation, resection of Hoffa’s pad, patellar rim electrocautery and preventing combined component internal rotation [11]. Vissers et al. (2012) focused their systematic review on psychosocial factors associated with TKA outcomes and identified pain catastrophizing and lower preoperative mental health as significant determinants of poor TKA outcomes [12]. Regardless of the evidence summarized by these systematic reviews, no consensus exists concerning either the identity or the strength of association between TKA determinants and poor outcomes. Consequently, there is an evident necessity of a comprehensive review encompassing the highest quality of evidence, which can be achieved by focusing on studies employing validated patient-reported outcome-measures (PROMs) of pain and function that also gauge the independent effect of determinants via multivariate analyses [13].
The purpose of this systematic review was to assess the current status of the literature evaluating the determinants of poor outcomes in terms of pain and functional levels following TKA. We also aimed to compare the determinants according to the approach of quantifying TKA results, i.e. as a measure of patients’ postoperative status or of postoperative change. Finally, because some studies evaluate pain and function either separately, such as in the case of Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and function subscales, or in a combined manner (total WOMAC score), we intended to parallel determinants according to this categorization.
MATERIALS AND METHODS
Literature Search and Study Identification
A search in four databases (Medline, Pubmed, Embase and CINAHL) from their respective inception dates until October 2014 was undertaken using a combination of keywords and MESH terms (see Appendix A). Manual searches of previously published reviews and reference lists from relevant articles were also conducted. Two authors independently reviewed the titles, abstracts and full texts of the articles in order to evaluate their eligibility.
Study Selection
The following selection criteria were applied:
- Participants were primary unilateral TKA patients with ≤10% of the sample undergoing unicompartmental knee arthroplasty, bilateral TKA or revision TKA
- ≥90% of the study sample was diagnosed with knee OA
- Results are presented for a follow-up between 6 months and 2 years
- The outcome measure was a disease-specific validated PROM assessing pain and/or function
- Identification of determinants was obtained using multivariate analyses
- Article is published in English or French
Data Extraction
A standardized form was employed to extract data. Participants’ characteristics (diagnosis, type of surgery, age and gender proportion), number of patients, follow-up period, outcome measures, statistical methods used and statistical adjustments, as well as significant and non-significant determinants reported by each study were recorded. Each article was extracted by one of the raters and verified by another in order to reduce the risk of extraction errors.
Methodological Quality Appraisal
Two trained reviewers independently performed the appraisal of the methodological quality of the included studies and results were discussed in order to reach consensus. In case of disagreement, a third reviewer was available for mediation of differences.
Description of the included studies.
| Study | Participants | Number of patients | Follow-up period | Outcome Measure | Statistical method | Statistical adjustment | Results | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | Type of Surgery | Mean Age (SD) | Gender (%female) | Significant Determinants | Non-significant Determinants | ||||||
| Alzahrani et al. (2011) [33] | Primary or secondary OA | Primary unilateral TKA | Cohort A: 67.5 (9.6) | Cohort A: 62% | Cohort A: 457 | 1 year | No clinical improvement at 1 year: Minimal Clinically Important Difference WOMAC: ≤ 7.5/100 points OKS: ≤ 5.0/60 points | Logistic regression |
Age, Gender BMI Comorbidity |
Cohort A: Increased age at time of surgery (-): OR 1.06 (95% CI 1.02-1.09) | Cohort A Gender BMI Comorbidity |
| Cohort B: 69.0 (9.1) | Cohort B: 63% | Cohort B: 2720 | Cohort B: Male gender (+): OR 0.72 (95% CI 0.57-0.92) | Cohort B: Age BMI Comorbidity | |||||||
| Overall: 68.2 (9.4) | Overall: 63% | Overall: 3177 | |||||||||
| Ayers et al. (2005) [42] | OA | Primary unilateral TKA | 68.0 (9.8) | 62.4% | 165 | 12 months | 12 month WOMAC-Physical function score improvement (change score) | Blocked multiple regression | NONE | Age (unclear) Gender (unclear) Worse preoperative physical function (WOMAC function) (-) Higher pre-operative mental health (SF-36 mental component score) (+) |
NONE |
| Baker et al. (2012) [16] | OA | Primary unilateral TKA | Not available | Not available | 22691 | 6 - 12 months (median 199 days) |
6 – 12 month OKS improvement (change score) | Stepwise multiple linear regression | NONE |
Higher age (+): estimate = 0.06 (95% CI 0.04 to 0.07) Higher preoperative function and lower pain (-): estimate = -0.66 (95% CI -0.67 to -0.64) Higher number of comorbidities (-): estimate = -0.25 (95% CI -0.39 to -0.12) Presence of self-reported pre-operative disability (-) estimate = -1.49 (95% CI -1.75 to -1.23) Very good self-reported pre-operative general health (vs. excellent) (-): estimate = -1.12 (95% CI -1.78 to -0.45) Good self-reported pre-operative general health (vs. excellent) (-): estimate = -2.78 (95% CI -3.42 to -2.12) Fair self-reported pre-operative general health (vs. excellent) (-): estimate = -5.23 (95% CI -5.93 to -4.53) Poor self-reported pre-operative general health (vs. excellent) (-): estimate = - 8.13 (95% CI -9.09 to -7.16) Presence of depression (-): estimate = -0.95 (95% CI -1.44 to 0.46) Moderate anxiety/depression (vs. no anxiety/depression) (-): estimate = -1.17 (95% CI -1.45 to -0.90) Severe anxiety/depression (vs. no anxiety/depression) (-): estimate = -2.78 (95% CI -3.48 to -2.07) ASA Grade 3 (vs. Grade 1) (-): estimate = -1.00 (95%CI -1.52 to -0.49) PFC prosthesis brand (vs NexGen) (-): estimate = -0.98 (95%CI -1.35 to -0.62) Genesis 2 prosthesis brand (vs NexGen) (-): estimate = -1.50 (95%CI -2.02 to -0.98) AGC prosthesis brand (vs NexGen) (-): estimate = -1.20 (95%CI -1.68 to -0.72) Triathlon prosthesis brand (vs NexGen) (-): estimate = -1.74 (95%CI -2.16 to -1.36) Independent hospital (vs. NHS hospital) (+): estimate = 0.83 (95%CI 0.35 to 1.31) ISTC (vs. NHS hospital) (+): estimate = 1.84 (95%CI 1.23 to 2.45) |
ASA Grade 2 |
| Caracciolo et al. (2005) [37] | OA | Primary TKA | 71.6 (6.6) | 81% | 47 | 6 months | WOMAC function score at 6 months | Logistic regression | NONE | Higher preoperative function (+), OR = 1.15, 95% CI = 1.04 to 1.28, compared to lower preoperative function (worst quartile of WOMAC function score) |
Preoperative osteoarthritis morbidity: Charnley or Modified Charnley Class C |
| Clement et al. (2013) [32] | Primary OA | Primary unilateral TKA | 70.4 (9.4) | 57.5 | 2392 | 1 year | 1 year OKS score | Multivariate linear regression analysis | NONE |
Presence of back pain (-): β = - 2.41 (95%CI -3.18 to -1.64) Presence of depression (-): β = - 4.17 (95%CI -5.42 to -2.92) Better pre-operative levels of pain and function (+): β = 0.45 (95%CI 0.39 to 0.51) Higher pre-operative mental health (+): β = 0.19 (95%CI 0.16 to 0.22) |
Gender Heart disease Hypertension Lung disease Vascular disease Neurological disease Diabetes mellitus Gastric ulceration Kidney disease Liver disease Anemia |
| Clement et al. (2013) [35] | N/A | Primary TKA | 70.4 | 56.6 | 2389 | 1 year | 1 year OKS score | Multivariate linear regression analysis | NONE |
Vascular comorbidity (-): β = -1.91, 95% CI -3.78 to -0.05 Depression (-): β = -4.19, 95% CI -5.44 to -2.95 Back pain (-): β = -2.38, 95% CI -3.14 to -1.61 Better pre-operative levels of pain and function (+): β = 0.45, 95% CI 0.39 to 0.51 Higher pre-operative mental health (+): β = 0.19 (95%CI 0.16 to 0.22) |
Heart disease
High blood pressure Lung disease Neurological disease Diabetes Stomach ulcer Kidney Disease Liver disease Anemia Pre-operative physical health |
| Clement et al. (2013) [40] | Primary OA | Primary TKA | 70.6 (7.0) | 57.6 | 966 | 1 year | Mean OKS improvement after 1 year | Multivariate linear regression analysis | NONE |
Presence of back pain (-): β = -2.53, 95% CI -3.75 –to -1.30 More than 4 comorbidities (-): β = -3.78, 95% CI -6.11 to -1.45 Higher preoperative function and lower pain (-): β = 0.58, 95% CI 0.50 to 0.87 Higher preoperative mental health (+): β =0.16, 95% CI 0.11 to 0.22 |
NONE |
| Davis et al (2008) [34] | Primary OA | Unilateral primary TKA | 71.1 (49 to 85)* | 51.0 | 974 | 12 and 24 months | 12 and 24 month total WOMAC score and WOMAC pain and function scores | Multivariate linear regression analysis |
Age, Gender Number of co-morbid conditions Country Center within country Pre-operative status |
WOMAC pain 12 months Low income (-):p = 0.014 |
WOMAC pain Low income at 24 months Education status at 3, 12 and 24 months WOMAC function Low income at 12 and 24 months Education status at 12 and 24 months |
| Desmeules et al. (2013) [17] | OA (96%), RA (4%) | Primary unilateral TKA | 67 (9.3) | 66% | 138 | 6 months | WOMAC pain and function scores at 6 months | Stepwise multiple regression analysis | NONE |
WOMAC pain (r2 = 0.11) Higher pre-operative pain level (-): β = 0.25, 95% CI 0.08-0.41 Cruciate retaining implant (-): β = -8.21, 95% CI -15.01 to -1.34 |
WOMAC pain Household living status Initial diagnosis (OA/RA) BMI Burden of comorbidities Duration of the disease Use of walking aid Pain contralateral knee Formal education Employment status Household income Size of social network Psychological distress Surgical variables – bearing type, patella resurfacing Marital status Occupational status |
|
WOMAC function (r2 = 0.16) Higher pre-operative function level (+): β = 0.35, 95% CI 0.16-0.54 Marital status (single, separated, divorced or widowed) (-): β = -6.84, 95% CI -14.74 to -0.95 Occupational status (unemployed or retired) (-): β = -7.77, 95% CI -14.70 to -0.87 |
WOMAC function Household living status Initial diagnosis (OA/RA) BMI Burden of comorbidities Duration of the disease Use of walking aid Pain contralateral knee Formal education Employment status Household income Size of social network Psychological distress Surgical variables – bearing type, patella resurfacing Implant type |
||||||||||
| Engel et al. (2004) [51] | OA | TKA | 67.1 (8.3) | 49.3% | 74 | 6 months | WOMAC pain and function scores at 6 months | Multiple hierarchical regression analysis |
Control of other variable (efficacy variables vs. expectancy variables) Adjustment for pre-operative WOMAC variables |
WOMAC pain
Higher coping efficacy (+): β = -0.338, p < 0.01 and High Arthritis Helplessness (-): β = 0.239, p < 0.05 adjusted r2 = 0.053 Expectancy variables: greater pessimism, grater expected chance of recovery, greater expected change in QoL: β not given, adjusted r2 = 0.067 |
WOMAC pain None |
|
WOMAC function Higher coping efficacy (+): β = -0.337, p < 0.05, adjusted r2 = 0.032 |
WOMAC function Arthritis Helplessness Expectancy variables: pessimism, expected chance of recovery, expected chance in QoL |
||||||||||
| Escobar et al. (2007) [24] | OA | Primary TKA | 71.8 (6.7) | 73.6% | 640 | 6 months | WOMAC Pain an function score at 6 months | General linear models | NONE |
WOMAC pain
Higher age (+): Diff β = -0.24, 95% CI -.045 to – 0.03 Presence of social support (+): Diff β = -5.13, 95% CI -9.31 to – 0.95 Absence of back pain (+): Diff β = -5.26, 95% CI -8.24 to -2.27 Charlson Index ≥ 2 (-): Diff β = 6.50, 95% CI 2.0 to 11.0 Higher pre-operative mental health (+): Diff β = -0.10, 95% CI -0.17 to – 0.04 Higher preoperative pain on WOMAC (-): Diff β = 0.26, 0.18 to 0.34 |
WOMAC pain Gender Charlson Index 1 |
|
WOMAC function
Presence of social support (+): Diff β = -7.25, 95% CI -9.31 to – 0.95 Absence of back pain (+): Diff β = -5.26, 95% CI -11.83 to -2.67 Charlson Index ≥ 2 (-): Diff β = 6.60, 95% CI 1.70 to 11.52 Higher pre-operative mental health (+): Diff β = -0.10, 95% CI -0.17 to – 0.03 Lower preoperative function on WOMAC (-): Diff β = 0.29, 0.19 to 0.38 |
WOMAC function Age Charlson Index 1 |
||||||||||
| Fortin et al. (1999) and Fortin et al. (2002) [9, 15] | OA | Primary TKA | 68.1± 9.1 | 56 % | 106 and 81 | 6 months and 2 years | WOMAC pain and function scores at 6 months and 2 years | Multiple linear regression | NONE |
WOMAC pain at 6 months: Higher preoperative pain (WOMAC pain score) (-): β = 0.44 ± 0.11, r2 = 0.25 |
WOMAC pain at 6 months: Age Gender Center Education Comorbidity |
| WOMAC function at 6 months: Lower preoperative function (WOMAC function score) (-): β = 0.61 ± 0.11, r2 = 0.36 |
WOMAC function at 6 months: Age Gender Center Education Comorbidity |
||||||||||
| Similar results for (2002); data not shown | |||||||||||
| Gandhi et al. (2010) [39] | Primary and secondary OA | Primary unilateral TKA | 66.5 | 61 | 889 | 1 year | WOMAC total score at 1 year | Linear regression modelling |
Age Gender Baseline total WOMAC score Comorbidity (excluding hypertension, hypercholesterolemia and diabetes) |
Obesity (BMI > 30) (-): β = 3.6, 95% CI 0.02 to 7.2 | Number of metabolic syndrome risk factors Hypertension Hypercholesterolemia Diabetes |
| Gandhi et al. (2013) [21] | OA | Unilateral TKA | 68.5 (9.4) | 57 | 28 | 2 years | Change in WOMAC pain score at 2 years | Linear regression modelling |
Age Gender BMI Comorbidity count |
Greater synovial fluid TNF- α levels (-): p = 0.001 Greater synovial fluid MMP-13 levels (-): p = 0.03 Greater synovial fluid IL-6 levels (-): p = 0.001 |
Serum levels of: IL-6 IL-1β MMP-9 MMP-13 MIP-1β MCP-1 Adiponectin Leptin TNF- α IFN-γ VCAM-1 |
| Synovial fluid levels of: IL-1β MMP-9 MIP-1β MCP-1 Adiponectin Leptin IFN-γ VCAM-1 |
|||||||||||
| Hanusch et al. (2014) [27] | OA | Primary TKA | 71 (42 to 92) | 45 | 100 | 1 year | 1 year OKS score | Stepwise multiple linear regression | NONE |
Model 1 None |
Model 1 Age Gender Pre-operative OKS score Consequences (patient’s beliefs about impact of illness on their life Emotional representation (patient’s negative emotions caused by their illness) |
|
Model 2 Better pre-operative function and lower pain (+): β = -0.296, p = 0.008 Higher anxiety (-): β = 0.270, p = 0.01 |
Model 2 Age Gender |
||||||||||
|
Model 3 Better pre-operative function and lower pain (+): β = -0.239, p = 0.04 Higher anxiety (-): β = 0.296, p = 0.01 |
Model 3 Age Gender |
||||||||||
| Jones et al. (2001) [41] | Osteoarthritis (93%) | Primary unilateral TKA | 70.6 | 59 | 257 | 6 months | Change in WOMAC pain and function scores at 6 months | Multiple linear regression models | NONE |
Change in pain Higher preoperative bodily pain (SF-36) (-): β = -0.42, 95% CI -0.56 to -0.27 Cementless prosthesis (-): β = -9.48, 95% CI -16.20 to -2.77 |
Change in pain
Age Gender Waiting time Number of comorbid conditions |
|
Change in function Lower preoperative joint pain (WOMAC) (-): β = -0.43, 95% CI -0.57 to -0.28 Higher number of comorbid conditions (-): β = -1.56, 95% CI -2.74 to -0.37 Higher preoperative bodily pain (SF-36) (-): β = -0.21, 95% CI -0.35 to -0.07 |
Change in function Age Gender Waiting time BMI Contralateral joint involvement Living alone |
||||||||||
| Jones et al. (2003) [10] | OA (94%) | Primary TKA | 69.2 (9.2) | 59 | 273 | 6 months | WOMAC function score at 6 months | Multiple linear regression | NONE |
Older age (+): β = 0.35, 95% CI 0.10 to 0.60 Higher preoperative function (WOMAC) (+): β = 0.30, 95% CI 0.16 to 0.43 Greater number of comorbid conditions (-): β = -1.62, 95% CI -2.75 to -0.49 Use of walking devices pre-operatively (-): β = -4.15, 95% CI -7.23 to -1.06 |
Gender |
| Judge et al (2012) [25] | OA (93.7%) | Primary TKA (92%) UKA (8%) | 71.7 (9.1) | 61 | 1991 | 6 months |
Model 1: Total OKS, OKS pain score and OKS function score at 6 months |
Model 1: Multiple linear regression |
Model 1: NONE |
Model 1: Total OKS Higher baseline OKS (+): multivariable coefficient = 1.70, 95% CI 1.43 to 1.96 Female sex (-): multivariable coefficient = -0.88, 95% CI -1.68 to -0.08 Higher preoperative BMI (-): multivariable coefficient = -0.44, 95% CI -0.86 to -0.01 Greater social deprivation (higher log of Index of Multiple Deprivation-IMD 2004) (-): multivariable coefficient = -1.40, 95% CI -1.96 to -0.85 RA diagnosis (vs. Primary OA) (+): multivariable coefficient = 2.90, 95% CI 0.42 to 5.37 Moderately anxious/depressed (vs. Not Anxious/Depressed) (-): multivariable coefficient = -0.85, 95% CI -1.68 to -0.03 Extremely anxious/depressed (vs. Not Anxious/Depressed) (-): multivariable coefficient = -2.21, 95% CI -4.34 to -0.09 |
Total OKS Age Operated side Diagnosis other than OA or RA ASA grade Year surgery was performed |
|
OKS pain score Higher baseline OKS (+): multivariable coefficient = 1.30, 95% CI 1.03 to 1.57 Greater social deprivation (higher log of IMD 2004)(-): multivariable coefficient = -0.64, 95% CI -0.91 to -0.37 RA diagnosis (vs. Primary OA) (+): multivariable coefficient = 1.75, 95% CI 0.61 to 2.89 Moderately anxious/depressed (vs. Not Anxious/Depressed) (-): multivariable coefficient = -0.43, 95% CI -0.83 to -0.03 Extremely anxious/depressed (vs. Not Anxious/Depressed) (-): multivariable coefficient = -1.19, 95% CI -2.19 to -0.18 |
OKS pain score Age Gender Preoperative BMI Operated side Diagnosis other than OA or RA ASA grade Year surgery was performed |
||||||||||
|
OKS function score Higher baseline OKS (+): multivariable coefficient = 1.82, 95% CI 1.58 to 2.06 Higher age (-): multivariable coefficient = -0.21, 95% CI -0.34 to -0.08 Female sex (-): multivariable coefficient = -0.79, 95% CI -1.25 to -0.33 Higher preoperative BMI (-): multivariable coefficient = -0.33, 95% CI -0.57 to -0.09 Greater social deprivation (higher log of IMD 2004)(-): multivariable coefficient = -0.79, 95% CI -1.11 to -0.46 |
OKS function score Operated side Diagnosis other than OA or RA RA diagnosis ASA grade Anxiety/depression level Year surgery was performed |
||||||||||
|
Model 2: PASS score for Total OKS, OKS pain score and OKS function score at 6 months |
Model 2: Logistic regression |
Model 2: NONE |
Model 2: PASS total OKS score Higher baseline OKS (+): OR = 1.52, 95% CI 1.40 to 1.66 Greater social deprivation (higher log of Index of Multiple Deprivation 2004) (-): OR = 0.73, 95% CI 0.62 to 0.87 RA diagnosis (+): OR = 2.17, 95% CI 1.02 to 4.60 |
Model 2: PASS total OKS score Age Gender BMI Operated Side Diagnosis other than OA or RA ASA grade Anxiety/depression level Year surgery was performed |
|||||||
|
PASS OKS pain score Higher baseline OKS (+): OR = 1.81, 95% CI 1.52 to 2.17 Greater social deprivation (higher log of Index of Multiple Deprivation 2004) (-): OR = 0.80, 95% CI 0.68 to 0.94 RA diagnosis (+): OR = 2.33, 95% CI 1.03 to 5.29 Moderately anxious/depressed (vs. not anxious/depressed) (-):OR = 0.67, 95% CI 0.54 to 0.84 Extremely anxious/depressed (vs. not anxious/depressed) (-):OR = 0.51, 95% CI 0.31 to 0.84 |
PASS OKS pain score Age Gender BMI Operated Side Diagnosis other than OA or RA ASA grade Year surgery was performed |
||||||||||
|
PASS OKS function score Higher baseline OKS (+): OR = 2.08, 95% CI 1.82 to 2.39 Older age (-):OR = 0.93, 95% CI 0.87 to 0.99 Greater social deprivation (higher log of Index of Multiple Deprivation 2004) (-): OR = 0.76, 95% CI 0.64 to 0.89 Moderately anxious/depressed (vs. not anxious/depressed) (-):OR = 0.77, 95% CI 0.61 to 0.97 |
PASS OKS function score Gender BMI Operated Side Diagnosis other than OA or RA ASA grade Extremely anxious/depressed (vs. not anxious/depressed) Year surgery was performed |
||||||||||
| Kauppila et al. (2011) [4] | OA | Primary TKA | 70.7 (5.5) | 75 |
88 |
12 months | 12 month WOMAC function change score | Multiple linear regression | NONE |
Multiple linear regression Male gender (-): β = -12.0, 95% CI -23.1 to -0.9 Presence of osteoporosis (-): β = -17.5, 95% CI -32.9 to -2.1 Higher pre-operative function (-): β = 0.31, 95% CI 0.06 to 0.56 |
Multiple linear regression Age Pre-operative function of the opposite knee |
| OMERACT-OARSI responder criteria | Multivariate logistic regression |
Multivariate logistic regression Presence of osteoporosis (-): OR = 14.7, 95% CI 1.1 to 106.1 |
Multivariate logistic regression Data not shown |
||||||||
| Lingard et al. (2004) [26] | OA | Primary TKA | 69.9 | 59.2 | 860 | 12 and 24 months | WOMAC pain and function at 12 and 24 months | Hierarchical linear modelling | NONE | WOMAC pain | WOMAC pain |
|
At 12 months Female gender (-): F = 7.06, p < 0.05, parameter estimate = -3.77, 95% CI -6.55 to -0.99 Lower preoperative pain (WOMAC pain score) (-): F = 29.16, p < 0.0005, parameter estimate = 0.20, 95% CI 0.13 to 0.28 Lower preoperative mental health (SF-36 mental health score) (-): F = 17.53, p < 0.0005, parameter estimate = 0.16, 95% CI 0.09 to 0.24 More comorbid conditions (-): F = 5.85, p < 0.05, parameter estimate = -1.33, 95% CI -2.41 to -0.25 |
At 12 months Age Country |
||||||||||
|
At 24 months Female gender (-): F = 3.98, p < 0.05, parameter estimate = -2.98, 95% CI -5.91 to -0.05 Lower preoperative pain (WOMAC pain score) (-): F = 25.13, p < 0.0005, parameter estimate = 0.20, 95% CI 0.12 to 0.28 Lower preoperative mental health (SF-36 mental health score) (-): F = 9.53, p < 0.005, parameter estimate = 0.13, 95% CI 0.05 to 0.21 More comorbid conditions (-): F = 4.59, p < 0.05, parameter estimate = -1.24, 95% CI -2.38 to -0.11 |
At 24 months Age |
||||||||||
| WOMAC function | WOMAC function | ||||||||||
|
At 12 months Higher age (-): F = 5.62, p < 0.05, parameter estimate = -0.19, 95% CI -0.35 to -0.03 Lower preoperative function (WOMAC function score) (-): F = 51.58, p < 0.0005, parameter estimate = 0.30, 95% CI 0.22 to 0.38 Lower preoperative mental health (SF-36 mental health score) (-): F = 17.04, p < 0.0005, parameter estimate = 0.17, 95% CI 0.09 to 0.25 Higher BMI (-): F = 4.70, p < 0.05, parameter estimate = -0.30, 95% CI -0.57 to -0.03 More comorbid conditions (-): F = 11.96, p < 0.005, parameter estimate = -1.95, 95% CI -3.05 to -0.84 |
At 12 months Gender |
||||||||||
|
At 24 months Lower preoperative function (WOMAC function score) (+): F = 55.75, p < 0.0005, parameter estimate = 0.34, 95% CI 0.25 to 0.43 Lower preoperative mental health (SF-36 mental health score) (-): F = 6.02, p < 0.05, parameter estimate = 0.11, 95% CI 0.02 to 0.20 Restricted knee flexion (-): F = 6.04, p < 0.05, parameter estimate = 0.12, 95% CI 0.02 to 0.21 More comorbid conditions (-): F = 13.96, p < 0.0005, parameter estimate = -2.26, 95% CI -3.45 to -1.07 |
At 24 months Age Gender |
||||||||||
| Lingard et al. (2004) [26] | OA | Primary TKA | 69.9 | 59.2 | 860 | 12 and 24 months | WOMAC pain and function at 12 and 24 months | Hierarchical linear modelling | NONE |
Lower preoperative function (WOMAC function score) (+): F = 55.75, p < 0.0005, parameter estimate = 0.34, 95% CI 0.25 to 0.43 Lower preoperative mental health (SF-36 mental health score) (-): F = 6.02, p < 0.05, parameter estimate = 0.11, 95% CI 0.02 to 0.20 Restricted knee flexion (-): F = 6.04, p < 0.05, parameter estimate = 0.12, 95% CI 0.02 to 0.21 More comorbid conditions (-): F = 13.96, p < 0.0005, parameter estimate = -2.26, 95% CI -3.45 to -1.07 |
|
| Lingard et al. (2007) [38] | OA | Primary TKA | 70.8 | 60.3 | 952 | 12 and 24 months | WOMAC pain and function at 12 and 24 months | General linear models |
Age Gender Number of comorbidities Country Center within country Preoperative scores |
With substitution of missing values | |
|
WOMAC pain
Higher preoperative mental health (SF-36) (+): At 12 months: parameter estimate = 0.128, p = 0.0008 At 24 months: parameter estimate = 0.096, p = 0.0109 |
|||||||||||
|
WOMAC function Higher preoperative mental health (SF-36) (+): At 12 months: parameter estimate = 0.150, p = 0.0001 At 24 months: parameter estimate = 0.106, p = 0.0071 |
|||||||||||
| Lopez-Olivo et al. (2011) [18] | OA | Primary TKA | 65 (9) | 65 | 232 | 6 months | WOMAC pain and function at 6 months | Multiple regression modelling | NONE |
WOMAC pain More education (+): β = -0.17, p =0.01 More comorbidities (-): β = 0.17, p = 0.008 More problem solving-style coping (+): β = -0.14, p =0.03 More dysfunctional coping (-): β = 0.13, p =0.04 More internal belief of control over health (+): β = -0.14, p =0.02 |
WOMAC pain BMI Baseline pain level |
|
WOMAC function More frequent availability of tangible support (+): β = - 0.15, p =0.01 Worse depressive state (-): β = 0.15, p = 0.02 More problem solving-style coping (+): β = -0.20, p =0.001 Lower baseline function level (-): β = 0.25, p =0.0001 |
WOMAC function BMI Comorbidities |
||||||||||
| Neuburger et al. (2013) [23] | OA (90%) |
Primary TKA (95%) Revision TKA (5%) |
N/A | 57% | 62,303 | 6 months | Total OKS score at 6 months | Logistic regression analysis |
Model 1: Age Sex Ethnicity Self-reported comorbid conditions Self-reported general health Primary OA Primary TKA or revision TKA Hospital |
Model 1: More social deprivation (2nd quintile vs. 1st quintile) (-): β = -0.7, 95% -0.9 to -0.5 More social deprivation (3rd quintile vs. 1st quintile) (-): β = -1.1, 95% -1.3 to -0.9 More social deprivation (4th quintile vs. 1st quintile) (-): β = -2.2, 95% -2.4 to -2.0 More social deprivation (5th quintile vs. 1st quintile) (-): β = -3.5, 95% -3.8 to -3.3 |
Model 1: NONE |
|
Model 2: Age Sex Ethnicity Self-reported comorbid conditions Self-reported general health Primary OA Primary TKA or revision TKA Hospital Preoperative OKS Longstanding problems |
Model 2: More social deprivation (2nd quintile vs. 1st quintile) (-): β = -0.4, 95% -0.6 to -0.2 More social deprivation (3rd quintile vs. 1st quintile) (-): β = -0.6, 95% -0.8 to -0.4 More social deprivation (4th quintile vs. 1st quintile) (-): β = -1.5, 95% -1.8 to -1.3 More social deprivation (5th quintile vs. 1st quintile) (-): β = -2.4, 95% -2.7 to -2.2 |
Model 2: NONE |
|||||||||
|
Model 3: NONE |
Model 3: Age < 51 years (vs. 71-80 years) (-): β = -2.9, 95% -3.4 to -2.4 Age 51-60 years (vs. 71-80 years) (-): β = -1.6, 95% -1.8 to -1.3 Age > 80 years (vs. 71-80 years) (-): β = -0.5, 95% -0.7 to -0.2 South-Asian, black or other ethnicity (vs. white ethnicity) (-): β = -2.5, 95% -2.9 to -2.2 Heart disease (-): β = -0.6, 95% -0.8 to -0.3 High blood pressure (+): β = 0.3, 95% 0.2 to 0.5 Stroke (-): β = -0.9, 95% -1.5 to -0.3 Poor circulation (-): β = - 2.3, 95% -2.6 to -2.0 Diabetes (-): β = -0.7, 95% -1.0 to -0.5 Depression (-): β = - 1.8, 95% -2.1 to -1.5 Very good general health (vs. excellent) (-): β = -1.2, 95% -1.6 to -0.9 Good general health (vs. excellent) (-): β = -3.6, 95% -4.1 to -3.3 Fair general health (vs. excellent) (-): β = -7.3, 95% -7.7 to -6.9 Poor general health vs. excellent) (-): β = -11.0, 95% -11.6 to -10.4 Diagnosis of OA (-): β = -0.5, 95% -0.9 to -0.3 Revision operation (-): β = -6.3, 95% -6.7 to -5.8 Longstanding problems (+): β = 0.4, 95% 0.3 to 0.6 Better preoperative pain/function (2nd decile of preoperative OKS score vs. 1st decile – lowest) (+): β = 2.5, 95% 2.0 to 2.9 Better preoperative pain/function (3rd decile of preoperative OKS score vs. 1st decile – lowest) (vs. 1st decile - lowest (+): β = 3.9, 95% 3.5 to 4.2 Better preoperative pain/function (4th decile of preoperative OKS score vs. 1st decile – lowest) (+): β = 4.8, 95% 4.5 to 5.2 |
Model 3: Gender Age 61-70 years (vs. 71-80 years) Lung disease Cancer |
|||||||||
| Papakostidou et al. (2012) [28] | OA (96%) | Primary TKA | 69.17 (6.69) | 79.4 | 204 | 12 months | WOMAC pain and function at 12 months | General linear modelling | NONE |
WOMAC pain Higher pre-intervention pain (-): Diff = 0.10, 95% CI 0.02 to 2.29 |
WOMAC pain Gender Age BMI Education Social support Residence |
|
WOMAC function Lower pre-intervention function (-): Diff = 0.17, 95% CI 0.06 to 0.28 |
WOMAC function Gender Age BMI Education Social support Residence |
||||||||||
| Perruccio et al. (2012) [19] | OA | Primary unilateral TKA | 65 | 65 | 494 | 12 months | WOMAC pain and function at 12 months | Multiple linear regression | NONE |
Pain Symptomatic ankles/feet/toes (-): β = 1.24, 95% CI 0.48 to 2.00 Symptomatic neck (-): β = 1.07, 95% CI 0.17 to 1.98 Higher pre-surgery knee pain (-): β = 0.34, 95% CI 0.24 to 0.45 |
Pain Age Gender Education BMI Comorbidity count Symptomatic contralateral knee Symptomatic hips Symptomatic elbows/wrists/hands Symptomatic shoulder Symptomatic spine/lower back |
|
Physical function Symptomatic ankles/feet/toes (-): β = 3.14, 95% CI 0.69 to 5.59 Symptomatic neck (-): β = 3.46, 95% CI 0.54 to 6.38 Higher Pre-surgery knee function (+): β = 0.41, 95% CI 0.31 to 0.50 |
Physical function Age Gender Education Overweight BMI Comorbidity count Symptomatic contralateral knee Symptomatic hips Symptomatic elbows/wrists/hands Symptomatic shoulder Symptomatic spine/lower back |
||||||||||
| Rajgopal et al. (2008) [20] | OA | Primary TKA (7.1% with history of contralateral TKA) | N/A | 59.3 | 550 | 1 year | Total WOMAC score at 1 year | Multiple linear regression | NONE |
Higher baseline mental health (+): β = 0.210, 95% CI 0.063 to 357 Charnley Class C (-): β = -4.897, 95% CI -8.701 to -1.093 Higher baseline WOMAC score (+): β = 0.301, 95% CI 0.202 to 0.399 BMI ≥40 (-): β = -5.188, 95% CI -9.771 to -0.606 |
Age Gender Prior contralateral TKA BMI |
| Ramaesh et al. (2013) [29] | Arthrosis | TKA | 70.5 | 58 | 205 | 1 year | Oxford Knee Score at 1 year | Multiple linear regression | NONE |
More comorbidity (-): B = -1.77, 95% CI -2.35 to -1.19 Better preoperative function/pain level (+): B = 0.26, 95% CI 0.10 to 0.43 |
Age Gender Personality type |
| Riddle et al. (2010) [22] | OA | Primary TKA | 63.7 | 70.7 | 157 | 6 months | WOMAC pain and function change scores at 6 months | Logistic regression |
Age Gender BMI Comorbidity Rheumatoid arthritis status Race/ethnicity Preoperative WOMAC pain score |
WOMAC pain score | WOMAC pain score |
|
Model 1: change by <50% Greater pain catastrophizing (PCS score ≥ 16) (-): OR = 2.67, 95% CI 1.2 to 6.1 |
Model 1 None |
||||||||||
|
Model 2: change ≤ 4 points Greater pain catastrophizing (PCS score ≥ 16) (-): OR = 6.04, 95% CI 1.75 to 20.82 |
Model 2 Self-efficacy Kinesiophobia |
||||||||||
| WOMAC function score | WOMAC function score | ||||||||||
|
Model 1: change by <50% None |
Model 1: change by <50% None |
||||||||||
|
Model 2: change ≤ 15 points None |
Model 2: change ≤ 15 points None |
||||||||||
| Smith et al. (2004) [52] | OA | Primary TKA | 67.2 (8.3) | 52 | 64 | 6 months | WOMAC pain and function at 6 months | Multiple linear regression analysis |
Gender Education Pre-surgery health measure |
NONE |
WOMAC Pain: Optimism Pessimism Emotionality Purpose in life |
|
WOMAC Function: Optimism Pessimism Emotionality Purpose in life |
|||||||||||
| Sullivan et al. (2011) [30] | OA | Primary TKA | 67 | 60.8 | 120 | 12 months | WOMAC pain and function at 12 months | Hierarchical regression analysis | NONE |
WOMAC pain Greater preoperative pain catastrophizing (-): β = 0.27, p < 0.05 |
WOMAC pain Preoperative pain Preoperative function Age Sex BMI Comorbidites Surgery Duration Surgeon Kinesiophobia Depression |
|
WOMAC function Greater preoperative pain catastrophizing (-): β = 0.34, p < 0.01 |
WOMAC function Preoperative pain Preoperative function Age Sex BMI Comorbidites Surgery Duration Surgeon Kinesiophobia Depression |
||||||||||
| Wylde et al. (2012) [31] | OA | Primary TKA | 70(9) | 62 | 220 | 1 year | WOMAC pain and function at 1 year | Ordinary least square regression | NONE |
WOMAC pain Higher pre-operative anxiety (-): Unstandardized regression coefficient = 1.082, 95% CI 0.283 to 1.881 Higher pre-operative pain severity (-): Unstandardized regression coefficient = 0.183, 95% CI 0.034 to 0.331 |
WOMAC pain Age Gender Other painful joints Number of comorbidities Depression Self efficacy |
|
WOMAC function Worse self efficacy (-): Unstandardized regression coefficient = -0.256, 95% CI -0.478 to -0.034 More painful joints elsewhere (-): Unstandardized regression coefficient = 1.928, 95% CI 0.634 to 3.222 Higher pre-operative anxiety (-): Unstandardized regression coefficient = 0.867, 95% CI 0.128 to 1.623 Worse preoperative function level (-): Unstandardized regression coefficient = 0.289, 95% CI 0.134 to 0.444 |
WOMAC function
Age Gender Depression |
||||||||||
| Yakobov et al. (2014) [36] | OA | Primary TKA | 67 (range 50 to 85) | 61 | 116 | 1 year | WOMAC pain and function at 1 year | Hierarchical regression analysis | NONE |
WOMAC pain Higher perceived injustice (-): β = 0.29, p < 0.01 |
WOMAC pain Age Sex BMI Illness duration Preoperative pain Number of comorbid health conditions Pain catastrophizing Kinesiophobia |
|
WOMAC function Greater preoperative pain catastrophizing (-): β = 0.26, p < 0.01 |
WOMAC function Age Sex BMI Illness duration Preoperative pain Number of comorbid health conditions Kinesiophobia Perceived injustice |
||||||||||
The risk of bias and the methodological quality of the included studies was assessed using a modified version of the Methodology Checklist for Prognostic Studies developed by Hayden et al. (2003) [14]. This tool includes six items: “Study participation”, ‘Study attrition”, “Prognostic factor measurement”, ‘Outcome measurement”, “Confounding measurement and account” and ‘Analysis”. Each item is evaluated according to its risk of potential bias: “yes” indicates a low risk of bias, “no” indicates a high risk of bias and “unclear” indicates an unclear or an unknown risk given the information available. For each item of the checklist, a score of 2 was given if a low risk of bias was present, a score of 1 if the risk was judged unclear and 0 if the risk was high. For the ‘Study participation” item, a score of 1 was attributed if the study was retrospective in nature and that no information was available regarding patients not included in the study because of incomplete data. For the “Study attrition” item, a score of 0 was given automatically if the follow-up proportion at the relevant time-point was inferior to 80%. A score of 0 was given for the “Confounding measurement and account” item if confounding factors such as age, gender and body mass index (BMI) were not accounted for in the multivariate analysis.
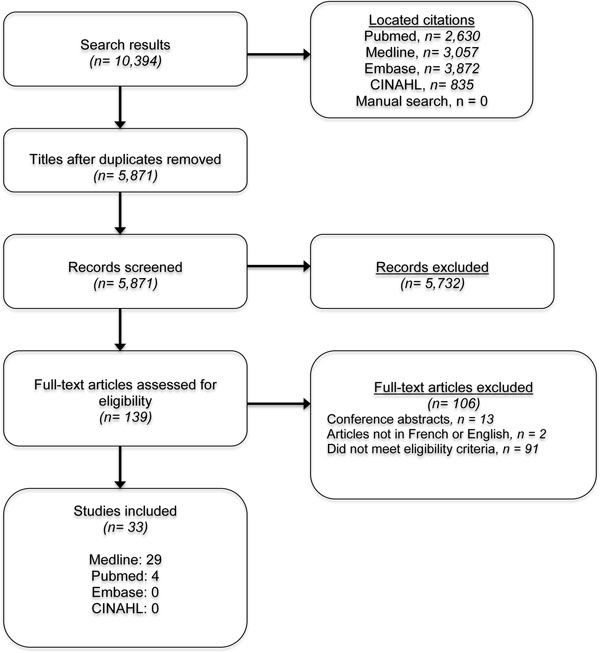
Flowchart of the literature search.
Data Synthesis
Determinants of TKA outcomes were summarized based on whether results were reported as postoperative change or postoperative status, and whether pain and function were assessed as separate or combined constructs. Given the nature of the study designs and the heterogeneity of included studies in terms of depended and independent variables’ constructs and definitions, as well as variations in follow-up periods, only a qualitative synthesis of results was performed.
RESULTS
Description of the Included Studies
Initial literature search yielded 139 full-text articles for assessment of eligibility. After further exclusion of 106 full-text articles for reasons presented in Fig. (1), 33 manuscripts were included. Table 1 indicates relevant characteristics of the included studies. Results from two manuscripts are presented conjointly because of analyses performed on the same cohort [9, 15]. The WOMAC was the validated tool used to measure postoperative pain and/or function in 24 studies, whereas the Oxford Knee Score (OKS) was employed in 9 studies. Nine studies have employed the change in pain and/or function after the surgery as an outcome measure. Postoperative raw scores at follow-up were considered as a measure of outcome in 25 studies. Six studies had a sample size smaller than 100 and 13 had a sample size greater than 500 patients. Only six studies presented a power calculation or considered a way of estimating required sample sizes [16-20].
Methodological Quality of the Included Studies
Table 2 indicates the methodological quality scores of the included studies after consensus. Mean total score for the methodological quality was 80.7% (SD 12.2%). No study received lower than 58.3% and four studies were graded 100% [17, 19, 21, 22]. Overall, these results indicate a moderate-to-high methodological quality.
Three domains of the methodology appraisal (“Prognostic factor measurement”, “Outcome measurement” and “Analysis”) scored on average the maximal possible grade. The domain with the worse mean score (1.00, SD 1.02) was “Confounding measurement and account”, with 17 studies not accounting for age, gender or BMI or other potential confounding factor in the multivariate analyses. A noteworthy number of studies (11 out of 33) reported a follow-up proportion inferior to 80%. This negatively impacted the study attrition domain.
Methodological appraisal of the included studies.
| Included studies (n= 33) | Study participation | Study attrition | Prognostic factor measurement | Outcome measurement | Confounding measurement and account | Analysis | Total score /12 |
|---|---|---|---|---|---|---|---|
| Alzharani et al. (2011) [33] | 2 | 1 | 2 | 2 | 2 | 2 | 11 |
| Ayers et al. (2005) [42] | 2 | 1 | 2 | 2 | 0 | 2 | 9 |
| Baker et al. (2012) [16] | 1 | 0 | 2 | 2 | 0 | 2 | 7 |
| Caracciolo et al. (2005) [37] | 2 | 1 | 2 | 2 | 0 | 2 | 9 |
| Clement et al. (2013) [35] | 1 | 1 | 2 | 2 | 0 | 2 | 8 |
| Clement et al. (2013) [32] | 2 | 2 | 2 | 2 | 0 | 2 | 10 |
| Clement et al. (2013) [40] | 1 | 1 | 2 | 2 | 0 | 2 | 8 |
| Davis et al. (2008) [34] | 2 | 2 | 2 | 2 | 0 | 2 | 10 |
| Desmeules et al. (2013) [17] | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Engel et al. (2004) [51] | 1 | 2 | 2 | 2 | 0 | 2 | 9 |
| Escobar et al. (2007) [24] | 2 | 0 | 2 | 2 | 2 | 2 | 10 |
| Fortin et al. (1999)9 & (2002) [15] | 2 | 0 | 2 | 2 | 0 | 2 | 8 |
| Gandhi et al. (2010) [39] | 2 | 1 | 2 | 2 | 2 | 2 | 10 |
| Gandhi et al. (2013) [21] | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Hanusch et al. (2013) [27] | 2 | 2 | 2 | 2 | 0 | 2 | 10 |
| Jones et al. (2001) [41] | 2 | 1 | 2 | 2 | 2 | 2 | 11 |
| Jones et al. (2003) [10] | 2 | 0 | 2 | 2 | 2 | 2 | 10 |
| Judge et al. (2012) [25] | 2 | 0 | 2 | 2 | 2 | 2 | 10 |
| Kauppila et al. (2011) [4] | 2 | 2 | 2 | 2 | 0 | 2 | 10 |
| Lingard et al. (2004) [26] | 2 | 0 | 2 | 2 | 2 | 2 | 10 |
| Lingard et al. (2007) [38] | 2 | 0 | 2 | 2 | 0 | 2 | 8 |
| Lopez-Olivo et al. (2011) [18] | 2 | 1 | 2 | 2 | 2 | 2 | 11 |
| Neuburger et al. (2013) [23] | 1 | 0 | 2 | 2 | 0 | 2 | 7 |
| Papakostidou et al. (2012) [28] | 2 | 1 | 2 | 2 | 2 | 2 | 11 |
| Perruccio et al. (2012) [19] | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Rajgopal et al. (2008) [20] | 2 | 1 | 2 | 2 | 2 | 2 | 11 |
| Ramaesh et al. (2013) [29] | 1 | 2 | 2 | 2 | 0 | 2 | 9 |
| Riddle et al. (2010) [22] | 2 | 2 | 2 | 2 | 2 | 2 | 12 |
| Smith et al. (2004) [52] | 1 | 0 | 2 | 2 | 0 | 2 | 7 |
| Sullivan et al. (2011) [30] | 2 | 0 | 2 | 2 | 2 | 2 | 10 |
| Wylde et al. (2012) [31] | 1 | 2 | 2 | 2 | 0 | 2 | 9 |
| Yakobov et al. (2014) [36] | 1 | 0 | 2 | 2 | 2 | 2 | 9 |
| TOTAL (mean ± SD) /12 | 1.71 ± 0.46 | 1.00 ± 0.84 | 2.00 ± 0.0 | 2.00 ± 0.0 | 1.00 ± 1.02 | 2.00 ± 0.0 | 9.69 ± 1.47 |
| TOTAL (mean ± SD) /100 | 85.4 ± 23.1 | 50.0 ± 42.1 | 100 ± 0.0 | 100 ± 0.0 | 50.0 ± 50.8 | 100 ± 0.0 | 80.7 ± 12.2 |
Preoperative Determinants of TKA Pain and Function Outcomes
Demographic Determinants
Fifteen studies investigated the association of age at the time of surgery and postoperative status. Neuburger et al. (2012) mention that being less than 60 years old is a significant determinant of poorer total OKS score at 6 months [23]. However, the same study reports that being older than 80 years old was also related to worse total OKS score at 6 months. Four more studies identified older age at the time of surgery as a factor associated with worse functional level following TKA [10, 24-26]. Nevertheless, ten studies report no significant effect of age on postoperative pain and function status [9, 15, 19, 20, 24, 27-31]. Eleven studies did not report a significant relationship between gender and TKA outcomes [9, 10, 15, 19, 23, 24, 27-29, 32, 33]. The two that found a significant association seem to yield more consistent results regarding the deleterious effect of female gender on TKA pain and function outcomes [25, 26].
Only limited evidence can be extracted regarding demographic determinants of postoperative change in terms of pain or function. In regards to gender, one study identified male gender to be associated with a smaller change in the 12-month WOMAC function score [4]. Alzharani et al. (2011) report that male patients were 0.72 times more likely to not achieve the minimal clinically important difference (MCID) for total OKS score 1 year after TKA compared to women, i.e. female gender is a determinant of unsatisfactory outcome [33]. Baker et al. (2012) suggest that younger age is associated with less improvement on the total OKS score recorded 6 to 12 months postoperatively, whereas Alzharani et al. (2011) indicate that older age is associated with lower odds of attaining the MCID of the total WOMAC score 1 year following TKA [16, 33].
Socioeconomic Determinants
Although scarce, the evidence regarding socioeconomic factors seems to point to several significant findings only in the case of the outcomes measured as postoperative status. Greater social deprivation was identified in two studies as a determinant of worse pain and functional limitation when simultaneously controlling for multiple confounding factors [23, 25]. A lower income was linked to a worse WOMAC pain score at 12 months post-operatively [34]. A lower educational status has been associated with better pain levels at 6 months in a study by Lopez-Olivo et al. (2012). However, six studies report no significant effect of education on either pain or function following TKA [9, 15, 17, 18, 28, 34].
Psychosocial Determinants
Several studies that were included in the review were dedicated at exploring the relationship between possible psychosocial determinants and TKA outcomes measured as postoperative status. Presence or higher levels of anxiety and/or depression have been consistently identified as significant determinants of worse TKA outcomes in six of the included studies [23, 25, 27, 31, 32, 35]. Two studies report that greater preoperative pain catastrophizing is linked to worse pain and disability12 months after TKA [30, 36]. Escobar et al. (2007) identified absence of social support to be related to worse 6-month pain and function levels [24]. Other significant psychosocial variables associated to pain and function status following TKA are presented in Table 3.
In terms of postoperative change, Riddle et al. (2010) determined that greater pain catastrophizing was related to higher odds of not achieving an improvement of 50% in the pain domain of the WOMAC at 6 months as well as not attaining a change greater than 4 points out of 20 on the WOMAC pain score at 6 months [22]. A previous diagnosis of depression and higher levels of depression/anxiety as measured by the EuroQ5D questionnaire were related to a smaller change on the 6 to 12 month total OKS score [16].
Significant pre-operative determinants of poor outcomes as measured by pain and/or function status at 6 weeks to 2 years following TKA.
| Determinant type | PAIN | Studies | FUNCTION | Studies | PAIN & FUNCTION combined | Studies |
|---|---|---|---|---|---|---|
| Demographic | Younger age | [24] | Younger age | [10] | Female gender | [23, 25] |
| Female gender | [26] | Older age | [25, 26] | South-Asian, black or other non-white ethnicity | [23] | |
| Female gender | [25] | Younger age | [23] | |||
| Single, separated or divorced | [17] | Older age | [23] | |||
| Socioeconomic | Low income | [34] | Unemployed or retired | [17] | Greater social deprivation | [23, 25] |
| Greater social deprivation | [25] | Greater social deprivation | [25] | |||
| Lower education level | [18] | |||||
| Psychosocial | Lower coping efficacy | [51] | Lower coping efficacy | [51] | Presence of depression | [23, 25, 32, 35] |
| High arthritis helplessness | [51] | Absence of social support | [24] | Higher anxiety level | [25, 27] | |
| Higher pessimism | [51] | Higher anxiety | [25, 31] | |||
| Lower expected chance of recovery | [51] | Higher depression level | [18, 25] | |||
| Lower expected change in quality of life | [51] | Less frequent availability of tangible support | [18] | |||
| Absence of social support | [24] | Less problem-solving coping style | [18] | |||
| Higher anxiety level | [25, 31] | Greater pain catastrophizing | [30, 36] | |||
| Higher depression level | [25] | Worse self-efficacy | [32] | |||
| Less problem-solving coping style | [18] | |||||
| More dysfunctional coping | [18] | |||||
| Less internal belief of control over health | [18] | |||||
| Greater pain catastrophizing | [30] | |||||
| Greater perceived injustice | [37] | |||||
| Clinical | Worse pain level | [9, 15, 17, 29, 24-26, 28, 32] | Worse function level | [9, 10, 15, 17-19, 24-26, 28, 31, 37] | Presence of back pain | [33, 35] |
| Presence of back pain | [24, 26] | Presence of back pain | [24] | Worse pain/function levels | [20, 23, 25, 27, 29, 35] | |
| Greater comorbidity | [18, 24, 26, 38] | Greater comorbidity | [10, 24, 26] | Worse mental health | [20, 33, 35] | |
| Worse mental health | [25] | Worse mental health | [10, 26, 38] | Worse general health status | [23] | |
| OA diagnosis | [19] | Use of walking devices | [10] | Vascular comorbidity | [23, 26] | |
| Symptomatic ankles/feet/toes | [19] | Higher BMI | [25, 26] | Obesity | [39] | |
| Symptomatic neck | [19] | Symptomatic ankles/feet/toes | [19] | Higher BMI | [20, 25] | |
| Symptomatic neck | [19] | OA diagnosis | [23, 25] | |||
| More painful joints elsewhere | [31] | Greater comorbidity | [20, 29] | |||
| Restricted knee flexion | [26] | Heart disease | [23] | |||
| Absence of high blood pressure | [23] | |||||
| Stroke | [23] | |||||
| Diabetes | [23] | |||||
| Revision surgery | [23] | |||||
| Shorter duration of symptoms | [23] | |||||
| Surgical | Cruciate-retaining implant | [17] | NONE | NONE | NONE | NONE |
Clinical Determinants
The investigation of the association between clinical characteristics and TKA outcomes measured as postoperative status has received a great deal of attention. One of the most studied potential determinants of knee pain and function following TKA is the baseline, preoperative levels of the respective variables. Seventeen studies linked a poor preoperative status to a worse postoperative status in terms of pain and function [9, 10, 15, 17-20, 23-25, 27, 28, 31, 32, 35, 37, 38].
Poor preoperative mental health, as measured by the SF-36 questionnaire, has been associated to worse outcomes in seven studies [18, 20, 24, 26, 32, 35, 38]. Even if TKA is performed predominantly for patients with primary OA, two studies seem to point to a diagnosis of primary gonarthrosis as a determinant of worse outcomes, when compared to rheumatoid arthritis or other diagnoses [23, 25]. Higher baseline BMI has been linked to poorer functional results as well as to worse outcomes of pain and function combined in four studies [20, 25, 26, 39]. Five studies identified the presence of back pain before surgery to be related to substandard pain and function status after TKA [19, 24, 28, 32, 35]. Regardless of whether comorbidity was measured as the influence of individual comorbidities, of the number of comorbidities per patient or when considering their severity and impact on patients’ life, seven studies suggests it to be a significant determinant of worse outcomes in terms of pain and function following TKA [10, 20, 23, 24, 26, 29, 35]. More symptomatic joints, including ankle, feet, toes and neck were associated with greater level of pain and worse function 12 months after TKA in two studies [19, 31]. Other significant clinical determinants of TKA outcomes measured as postoperative status can be found in Table 3.
Regarding outcomes measured as postoperative change, four studies report that better baseline levels of function and/or pain are related to lower levels of improvement following TKA. Jones et al. (2001) reported that lower preoperative pain was associated with smaller changes in functional abilities 6 months after the surgery [10]. A better preoperative total OKS score was related to a smaller change 6 to 12 months following TKA in two studies [16, 40]. Better preoperative function level was found to be a significant determinant of lower gains in functional abilities [4].
Greater comorbidity was shown to significantly determine lower changes in pain and functional status [16, 40, 41]. In particular, Kauppila et al. (2011) showed that presence of osteoporosis was associated with a smaller level of change in function and with decreased odds of attaining the OMERACT-OARSI set of responder criteria 12 months after surgery [4]. A study by Gandhi et al. (2013) revealed that a greater level of synovial fluid levels of three inflammatory markers (TNF- α, MMP-13 and IL-6) were related to poor gains in physical function 2 years after TKA as measured by the WOMAC function score [21]. Other miscellaneous clinical determinants identified in the included studies were worse general health status (as measured by the American Society of Anaesthesiology grade), presence of self-reported disability and lower self-reported general health [16], greater preoperative bodily pain [41], worse mental health [40, 42] and presence of back pain [40].
Surgical Determinants
Only one of the included studies identified a significant surgical determinant of poor postoperative status as measured by pain levels at 6 months: cruciate-retaining implant [17]. Sullivan et al. (2011) studied the effect of surgery duration and of the identity of the surgeon on the 12-month WOMAC pain and function scales, but their analysis yielded non-significant results [30].
In terms of postoperative change, findings by Jones et al. (2001) indicate that cementless prosthesis is associated with a lower change in the WOMAC pain score 6 months after TKA [41]. A British study by Baker et al. (2012) evaluated the effect of different types of prosthesis brands on the improvement of the total OKS score 12 months following the intervention. They found that the NexGen prosthesis brand is related to greater improvements when compared to all the other brands used in their study (PFC, Genesis 2, AGC and Triathlon) [16]. The same study evaluated the effect of the type of hospital where the surgery was performed. They showed that surgeries performed at a National Health Services hospital are more likely to be associated with poor improvement than surgeries performed at an independent hospital or an Independent Sector Treatment Centre.
DISCUSSION
Because TKA clinical results are still suboptimal in a large percentage of patients, a better knowledge of determinants of pain and function following the intervention could help improve outcomes. The aim of our study was to systematically assess the literature reporting the determinants of pain and functional outcomes following primary unilateral TKA in patients with knee OA. Thirty-four studies with a moderate-to high mean methodological quality (80.7%, SD 12.2%) were included. Even if several significant determinants of pain and functional outcomes following TKA have been summarized by studies, no conclusions can be reached regarding the strength of the associations between significant determinants and TKA results because of heterogeneity of study methodologies and results.
Strengths and Limitations of the Review
The main strength of the present systematic review is the rigorousness of the inclusion criteria ensuring high quality of evidence of determinants compiled from four important databases. Moreover, focus on all types of determinants provides a comprehensive overview of all relevant variables with a significant relationship to TKA outcomes.
The main limitation is the inability to pool the results into meta-analyses, resulting in the failure to conclude on the strength of association between patient factors and TKA outcomes due to the heterogeneity of the methodologies of the included studies. Moreover, the findings of the review do not necessarily apply to all patients undergoing TKA, namely those with a diagnosis different from OA, or undergoing bilateral or revision surgery. Also, the study does not review determinants of long-term outcomes. Finally, two studies had to be excluded because they were published in languages not mastered by the reviewers.
Main Findings
It is difficult to conclude to a significant association of any demographic determinant with TKA pain or functional outcomes based on the results of the included studies. Although female gender and older age were found significant in several studies, there is an overwhelming amount of evidence pointing to either an association in an opposite direction or to no relationship at all. These findings contrast the ones by Santaguida et al. (2008) in their systematic review. We therefore suggest that according to the available evidence, patients should not be denied surgery based on gender or age.
Regarding socioeconomic determinants, greater social deprivation achieved statistical significance in both studies evaluating its association with TKA outcomes among patients in the United Kingdom [23, 25]. Patients with greater social deprivation may experience worse TKA outcomes because of an inequality in the continuity of care following discharge compared to patients with less deprivation [23]. Caution should be warranted regarding the generalizability of these findings however, as they may not apply to other countries, although the impact of social deprivation in terms of pain and function on other musculoskeletal disorders is well established [43, 44].
Psychosocial determinants with considerable evidence include the presence or a greater level of depression and/or anxiety. The previous review by Vissers et al. (2012) did not find definite evidence that supports the significance of this association. However, all of the seven studies included in our review that conclude to such a relationship were published after the beforementioned systematic review. The causes behind the significant association are not well understood; depressed patients might be less likely to participate actively in the rehabilitation process, thus experiencing worse outcomes [18]. Greater preoperative pain catastrophizing was also significantly associated to pain and functional outcomes after TKA, a finding consistent with the review by Vissers et al. (2012). It has been suggested that pain catastrophizing is linked with neurophysiological processes related to modulation of pain, and that greater levels of catastrophizing promote sensitization to pain [30].
The greatest amount of evidence is available for clinical determinants, the frontrunner being the relationship between worse or better preoperative levels in the respective dimensions (depending on the outcome being measured as postoperative patient state or change) and pain or functional outcomes. Although studies consistently refer to this relationship as a well-known fact, to our knowledge, this is the first systematic review underlining this fact. Our findings suggest that in the case of measuring outcome as a change in status, a higher preoperative status is related to a lower chance of improvement. In the case of measuring outcome as health status postoperatively, lower preoperative status is related to worse outcome. The importance of these concepts relies in the dilemma encountered when employing this information clinically: should intervention be undertaken in patients with worse preoperative state in order to obtain greater gains or should TKA be performed in patients as early as possible before they deteriorate considerably in order to guarantee better status after the surgery? Unfortunately, there does not seem to be a consensus regarding this predicament, and our review only emphasizes its importance, as other authors have done as well [45].
Presence or greater levels of comorbidities were also related to a worse outcome after TKA. The reasons behind such a relationship are unclear. Patients with other comorbidities may not meet the demands of the intensive rehabilitation process following TKA, thus explaining their increased risk of poor surgical outcomes [26]. Several studies advocate that patients should receive appropriate counselling from their surgeon preoperatively according to the identity and number of their comorbidities [26, 39]. Of interest, presence of back pain was associated to poor TKA outcomes as well. The mechanism behind this association is however uncertain. Back pain may impede postoperative recuperation and rehabilitation or it may directly affect how patients rate their condition in terms of knee pain and function on the WOMAC, or on other outcome measures [24].
Worse measures of general health were significantly related to poor TKA outcomes in a surprisingly consistent manner. Among the included studies, general health was mainly measured with the SF-36 questionnaire, and a poorer mental health domain in particular was consistently related to poor pain and function after TKA. This may underlie the importance of the overall health status, especially the extent of psychological distress, in selecting individuals for knee arthroplasty.
Limited evidence has been identified regarding surgical determinants of poor TKA outcomes. This may be due to the fact that surgical factors are traditionally investigated by studies employing a clinical trial methodology, whereas this review encompasses prognostic cohort studies. Association of surgical and technical factors with TKA outcomes is clearly a complex issue, and a different approach than the one employed by this review may be required to identify significant determinants.
No variable was consistently identified as non-significantly related to TKA outcome. The amount of evidence for certain significant determinants is nevertheless countered by numerous studies stating their non-significance and this inconsistency represents a limitation of the available literature. Several reasons behind this discrepancy can emerge. Firstly, a low sample size can impact the ability to detect a truly present statistically significant relationship; type II errors may effectively limit the findings. Also, the duration of follow-up may lead to a disagreement as a significant relationship may arise at a critical time-point following the surgery. Finally, the methodological quality of the studies can lead to heterogeneous results.
It has previously been suggested that the determinants of pain and function after TKA are not the same [25]. We attempted to appraise this by capturing the results of the included studies based on whether determinants were assessed for pain and function as separate dependent variables or part of a combined construct (Tables 3 and 4). On several occasions, individual studies that evaluated significant determinants of pain and function separately concluded that they indeed presented different determinants. However, when viewing the overall picture, the determinants of pain and function seem to be similar regardless of the method of measurement. This is most probably due to the overlap between the findings of the studies.
Significant pre-operative determinants of poor outcomes as measured by change in pain and/or function status 6 weeks to 2 years following TKA.
| Determinant type | PAIN | Studies | FUNCTION | Studies | PAIN & FUNCTION combined | Studies |
|---|---|---|---|---|---|---|
| Demographic | NONE | NONE | Male gender | [4] | Younger age | [16] |
| Older age | [33] | |||||
| Female gender | [33] | |||||
| Socioeconomic | NONE | NONE | NONE | NONE | NONE | NONE |
| Psychosocial | Greater pain catastrophizing | [22] | NONE | NONE | Presence of depression | [16] |
| Greater depression level | [16] | |||||
| Clinical | Greater levels of inflammatory markers • Greater synovial fluid TNF- α levels • Greater synovial fluid MMP-13 levels • Greater synovial fluid IL-6 levels |
[21] | Better pain level | [41] | Better pain/function levels | [16, 40] |
| Higher bodily pain levels | [41] | Greater comorbidity | [41] | Worse general health status | [16] | |
| Higher bodily pain levels | [41] | Greater comorbidity | [16, 40] | |||
| Worse mental health | [42] | Presence of self-reported disability | [16] | |||
| Presence of osteoporosis | [4] | Lower self-reported general health | [16] | |||
| Better function level | [4] | Presence of back pain | [41] | |||
| Worse mental health | [4] | |||||
| Presence of osteoporosis | [4] | |||||
| Surgical | Cementless prosthesis | [42] | NONE | NONE | PFC prosthesis brand | [16] |
| Genesis 2 prosthesis brand | [16] | |||||
| AGC prosthesis brand | [16] | |||||
| Triathlon prosthesis brand | [16] | |||||
| Healthcare-related | NONE | NONE | NONE | NONE | Surgery performed at a National Health Services Hospital (United Kingdom) | [16] |
As mentioned previously, outcomes after TKA are generally evaluated as a function of health change or of health state postoperatively [46-50]. In our review, we identified fewer studies evaluating determinants based on postoperative change. Generally, from the available evidence, determinants are similar between the two approaches, with the exception of the preoperative status as discussed previously.
CONCLUSION
Moderate-to-high methodological quality of included studies suggests that preoperative determinants of pain and function outcomes following TKA include greater social deprivation, the presence or a greater level of depression and/or anxiety, greater preoperative pain catastrophizing, preoperative pain or function levels, presence or greater levels of comorbidity, presence of back pain and lower general health. Consensus is however limited by contradictory results regarding the importance of several determinants. The heterogeneity in the measurement of the outcome limits the ability to generalize the magnitude of association of determinants with TKA outcomes. Further high-quality research and a more standardized reporting of results is required in order to elucidate with greater precision the identity of determinants of pain and function following TKA in order to provide the best possible care for patients with severe knee OA.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


