All published articles of this journal are available on ScienceDirect.
Late Anterior Dislocation Due to Posterior Pelvic Tilt in Total Hip Arthroplasty
Abstract
Background:
Excessive pelvic tilt may be one of the factors leading to instability in total hip arthroplasty (THA), even when the acetabular cup is placed properly. To our knowledge, only a few studies have described late anterior dislocation due to posterior pelvic tilt. We present 3 cases with late anterior dislocations possibly due to posterior pelvic tilt.
Cases Presentations:
Case-1: An 84-years-old woman fell and presented with an anterior dislocation 12-years after THA. Her pelvis had tilted to approximately 30° posteriorly in a supine position. After conservative treatment, she presented with 10 recurrent anterior dislocations. She had thoracolumbar kyphosis due to multiple compression fractures. Revision with anterior placement of an elevated liner and a 32-mm head corrected the dislocation, and no further dislocations occurred.
Case-2: A 78-years-old woman fell and presented with an anterior dislocation 4-years after THA. Her posterior pelvic tilt had increased 23° due to a lumbar compression fracture. Revision by decreasing the cup anteversion was performed, but recurrent posterior dislocations occurred. Owing to her worsened general condition, further treatment was abandoned.
Case-3: A 79-years-old woman twisted her body and presented an anterior dislocation 3-years after THA. After manual reduction and conservative treatment, the dislocation recurred. Her posterior pelvic tilt had increased 16°.
Conclusion:
Although minor trauma triggered the anterior instability in these patients, the underlying pathomechanism existed in the progressive pelvic posterior tilt due to thoracolumbar kyphosis. As longer life expectancy as well as implant survivorship is predicted, attention must be paid to the change of pelvic tilt in elderly patients.
BACKGROUND
Dislocations are one of the most frequent complications to occur after total hip arthroplasty (THA), with anincidence of 0.6% to 11% during the early postoperative period [1-3]. Posterior dislocations occur more frequently;
however, anterior dislocations account for approximately 20% of all dislocations [4-6]. The factors that affect dislocation risk include patient characteristics, implant design, and variations in surgical techniques [7-9]. Of these factors, 13% to 30% of dislocations are reportedly caused by implant malpositioning [10, 11].
During THA, surgeons determine where to place the acetabular cup using bony landmarks of the pelvis or planes, such as the anterior pelvic plane (APP), which is formed by the anterior superior iliac spines and the pubic symphysis, for reference [12-15]. However, because the sagittal pelvic tilt can change the version of the cup relative to the stem, any excessive pelvic tilt may lead to subsequent implant malpositioning and dislocation. Previous studies have described large inter-individual variations in pelvic tilt ranging from 20 degrees posteriorly to 20 degrees anteriorly [13, 16]. Other intra-individual variations have also been reported; for example, decreased lumbar lordosis with aging has been shown to result in an increase in posterior pelvic tilt among elderly individuals [17]. Likewise, a high incidence of posterior pelvic tilt has been reported in patients with advanced-stage ankylosing spondylitis [18, 19]. In cases involving posterior pelvic tilt, anterior dislocation is a concern after THA because the tilting is thought to be accompanied by increased anteversion of the cup. To our knowledge, only a few studies have described late anterior dislocation due to posterior pelvic tilt [20].
Here, we present 3 cases with recurrent anterior dislocations caused by minor trauma occurring more than 2 years after THA. We report that the recurrent dislocations appeared to be caused by aging and posterior pelvic tilt.
CASE 1
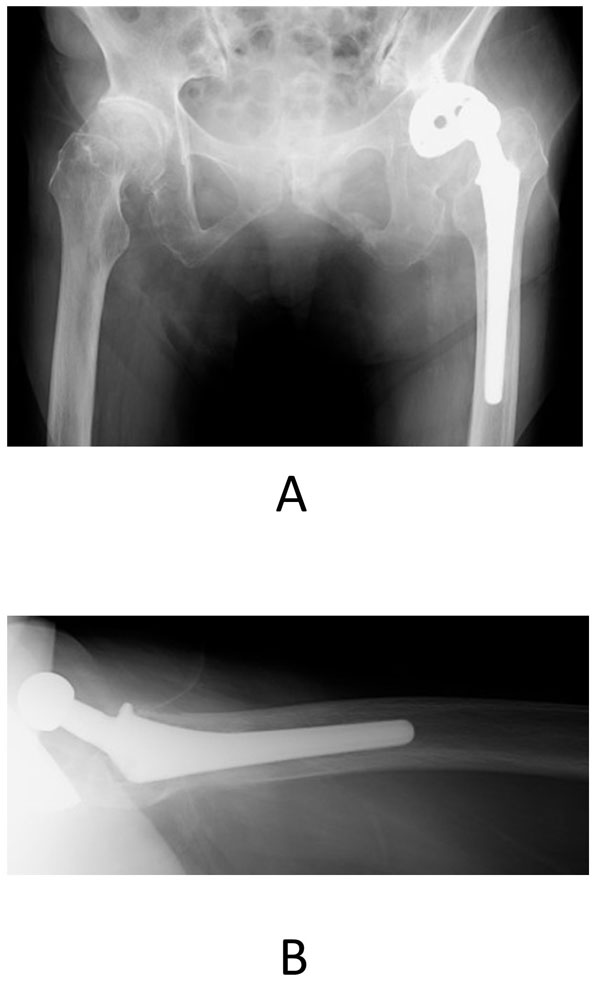
A 72-year-old woman presented with osteoarthritis in her left hip and underwent cementless THA (AMS and PerFix, 46 mm Cup, elevated liner, 22 mm zirconia, Kyocera, Japan). The cup inclination was measured as an abduction angle using the interteardrop line as the baseline. The cup anteversion was calculated using trigonometric function from anteroposterior radiographs following the method of Lewinnek et al. [21]. Cup anteversion was 16.1 degrees and cup inclination was 37.3 degrees. No joint instability was observed during surgery. There were no complications after surgery. The woman fell 12 years after the surgery (when she was 84 years old) and presented with an anterior dislocation of the left hip joint (Fig. 1). Manual reduction and conservative treatment with a brace were performed. However, after treatment, she presented with 10 recurrent anterior dislocations.
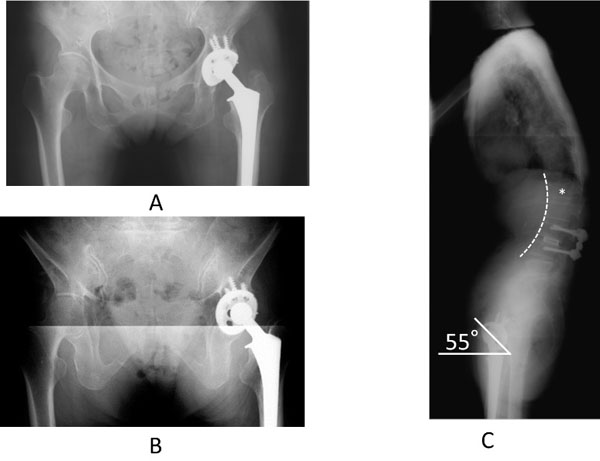
We quantified the changes in pelvic tilt on the sagittal plane using the aspect ratio of the obturator foramen (OF) on anteroposterior pelvic radiographs [22-25] (Fig. 2A). The ratio increased from 1.0 to 1.43 at 12 years after the primary THA, and the pelvis was tilted approximately 30 degrees posteriorly when measured with the patient in a supine position. When measured in a standing position, the pelvis was found to have tilted an additional 13 degrees posteriorly compared to the supine position. Osteoporotic changes were observed in the thoracolumbar spine. Prior compression fractures were also observed in T10, T11, and L1, and the spine showed significant kyphosis. Cup anteversion in the standing position measured from anteroposterior radiograph increased to 48 degrees. Lateral views of the pelvis in the standing position revealed that the APP was tilted 46 degrees posteriorly against the floor and that the anterior opening angle of the acetabular cup was 57 degrees (Figs. 2B and C). Owing to systemic complications, revision of the acetabular cup was not performed. A 15-degree elevated liner was placed in the anterior direction and a 32-mm enlarged femoral head was revised. No dislocations occurred after this procedure.
CASE 2
A 74-year-old woman presented with rheumatoid arthritis and underwent THA (AMS and PerFix, 48 mm Cup, elevated liner, 22 mm zirconia, Kyocera, Japan) (Fig. 3A). Cup anteversion was 15.6 degrees and cup inclination was 47.1 degrees. No joint instability was observed during surgery. When she was 76 years old, L3/4 posterior lumbar interbody fusion was performed for lumbar spinal canal stenosis. After this procedure, she had a compression fracture of the first lumbar vertebra. Two years later (when the woman was 78 years old), she fell and presented with an anterior dislocation of the left hip joint. Manual reduction and conservative treatment with a brace were performed. However, she presented with recurrent anterior dislocations.
Her pelvis was tilted 23 degrees posteriorly in the supine position 4 years after surgery compared to that observed immediately after surgery. When measured in the standing position, the pelvis was found to have tilted an additional 7 degrees posteriorly and cup anteversion measured from anteroposterior radiograph increased to 48 degrees (Fig. 3B). Owing to the compression fracture of the first lumbar vertebra, the thoracic and lumbar vertebrae displayed a convex curvature. The lateral view of the pelvis in the standing position revealed that the APP was tilted 30 degrees posteriorly against the floor, and the anterior opening of the acetabular cup was 57 degrees (Fig. 3C). When revision THA was performed, the anterior opening angle of the acetabular component decreased. However, she started to have recurrent posterior dislocations. Because the general condition of the patient worsened, further treatment was abandoned.

CASE 3
A 76-year-old woman presented with osteoarthritis of her left hip and underwent THA (AMS and PerFix, 48 mm Cup, elevated liner, 22 mm zirconia, Kyocera, Japan). Cup anteversion was 16 degrees and cup inclination was 46.5 degrees. No joint instability was observed during surgery. Three years after surgery (when she was 79 years old), she presented with an anterior dislocation of her left hip when she turned to the right while in an upright position. The dislocation was manually reduced, and conservative treatment with a brace was performed. However, she again presented with an anterior dislocation. In comparison to when the patient first underwent surgery, the pelvis was tilted 16 degrees posteriorly in the supine position. Cup anteversion in the supine position measured from anteroposterior radiograph increased to 48 degrees when the dislocation occurred.
DISCUSSION
We have described 3 cases who presented with recurrent anterior dislocations caused by minimal trauma several years after THA. All the patients were elderly women, and in all cases, the pelvis was greatly tilted posteriorly. As seen in cases 1 and 2, kyphosis can result from aging and compression fractures, and is considered a cause of anterior dislocation.
Aging and Posterior Pelvic Tilt
Aging generally results in posterior pelvic tilt because elderly patients are prone to compression fractures and lumbar spondylolisthesis. All the patients reported here were elderly women and had significant posterior pelvic tilt, especially in standing position. Sato et al. reported that more than 20 degrees of posterior pelvic tilt may cause anterior instability and diminish the optimal range of cup version [20]. Tamura et al. reported that the presence of thoracolumbar compression fractures, lumbar spondylolisthesis, and posterior tilt of the first sacral vertebra could result in greater increase of the posterior pelvic tilt between the supine and standing positions [25]. Shon et al. suggested the placement of an acetabular cup in cases with kyphosis. They reported a case with multiple anterior dislocations occurring 3 months after THA [26]. This case showed decreased sacral tilt by 33 degrees from the supine to the standing position and increased anteversion of acetabular cup by 35 degrees. In Cases 1 and 2 presented here, compression fractures in the vertebrae were observed. They had increased posterior pelvic tilt compared to that observed immediately after surgery in the supine position, and furthermore, the pelvic tilt increased by 13 and 7 degrees from the supine position to the standing position, respectively. This was considered to have increased the risk of anterior dislocation in these patients. Based on these findings, not only the pelvic tilt in the supine position but also that in the standing position should be confirmed prior to surgery for the optimal placement of acetabular cups. To prevent the progression of lumbar kyphosis and the subsequent posterior pelvic tilt, extensive treatment for osteoporosis should be emphasized.
Late and Recurrent Dislocations
In terms of late dislocations, Von Knoch et al. reported that the rate of initial dislocations was 0.19% at 5 years after THA; however, according to a later study, the rate had increased to 0.84%, suggesting increasing incidence of late dislocation [3-27, 28]. This was considered a consequence of the increased durability of the implant and longer life expectancy. We previously reported that late dislocation was significantly associated with recurrent dislocations, which may lead to substantial disability in daily life and sometimes require surgical intervention [29]. Moreover, aging itself is a risk factor for hip dislocation [30].
Thus, extensive care should be paid to the elderly patient with dislocation to avoid recurrence. However, conservative treatment with manual reduction and a brace worked only in Case 3, who had relatively mild posterior pelvic tilt, and not in Case 1 or 2. The use of an elevated liner placed at the anterior portion stopped dislocations in Case 1. However, Case 2 developed a posterior dislocation owing to reduction of cup anteversion, showing the refractory nature of the recurrent dislocation. Hernigou et al. [31] reported the significant reduction of re-dislocation in the patients with constrained liners compared to those without constrained liners in their 7 years-follow-up. Hamadouche et al. [32] reported that a dual mobility cup had provided restoration of hip stability in 96% of patients presenting with recurrent dislocation. Although these specific implants were not available at that time, they could have significant roles in the treatment of these difficult patients to treat.
Limitations
Our case study had several limitations. First, of the 3 cases presented, the pelvic tilt in the standing position could not be determined in case 3, as the necessary radiographs were not available. Second, pelvic tilt was only evaluated using plain radiographs. The OF ratio that correlates with pelvic tilt (r = 0.31) [22-25] was used as an indicator of pelvic tilt. However, if other imaging modalities such as computed tomography had been used, pelvic tilt could have been evaluated in more detail.
CONCLUSION
In this report, we have described 3 patients who developed late anterior dislocations after THA. In elderly patients, it is important to evaluate pelvic tilt using images of different postures before and after THA, and to respond to changes in pelvic tilt that could cause dislocations.
LIST OF ABBREVIATIONS
| APP | = Anterior pelvic plane |
| OF | = obturator foramen |
| THA | = Total hip arthroplasty |
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
This work was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (No. 15K10450).


