All published articles of this journal are available on ScienceDirect.
Impact of Alprazolam on Comorbid Pain and Knee Functions in Total Knee Arthroplasty Patients Diagnosed with Anxiety and Depression
Abstract
Purpose:
Studies report 19-33% postoperative moderate-severe pain and dissatisfaction in uncomplicated total knee arthroplasty (TKA), even after 1 year. High rates of undiagnosed depression and anxiety may have a strong impact on these unfavourable outcomes. Here we aimed to investigate the efficacy of alprazolam on postoperative analgesic use and knee functions.
Methods:
Seventy-six patients with a mean age of 65 ± 9.3 years (range 46-80) diagnosed with mild-moderate anxiety or depression according to the Hamilton anxiety scale (HAS) and Beck Depression Inventory (BDI) that underwent TKA were evaluated in the study. Group 1 patients were subjected to alprazolam treatment in addition to an analgesic/antiinflammatory drug, whereas Group 2 consisted of patients receiving only the standard postoperative pain management protocol. Visual analog scale (VAS) and postoperative analgesic use (g/day) were calculated to evaluate the magnitude of pain experienced. Preoperative and postoperative knee functions were assessed from the patients’ Knee Society Score and Knee Society Functional Score records.
Results:
A positive correlation was found between the preoperative HAS, BDI, and total postoperative analgesic use in both groups. Although the decrease in VAS was significant in both groups, postoperative analgesic need (4.25 ± 0.30 g) in Group 1 was less compared to Group 2 (4.81 ± 0.41 g) (p=0.01). The mean change in postoperative (1 month) Knee Society Score and Knee Society Functional Score were also significantly improved in Group1 compared to Group 2.
Conclusion:
Alprazolam can reduce postoperative analgesic use and improve knee functions by reducing the pain threshold, and enhancing overall mood via its antidepressive and anxiolytic properties in patients undergoing TKA diagnosed with mild-moderate anxiety/depression.
INTRODUCTION
Approximately one third of individuals older than 65 experience symptomatic osteoarthritis (OA) of the knee and 80% have degenerative joint disease after 70 years of age. Characterized by progressive loss of articular cartilage, functional restrictions, and chronic pain, OA remains a significant burden for patients and health systems. Especially in advanced stages of OA, total knee arthroplasty (TKA) is considered to be the primary care option and the number of patients undergoing TKA has grown dramatically in recent years, which has been paralleled with the advancement of surgical techniques, implant design, and material properties. Although this procedure has proven to reduce pain, increase physical functions, and is generally accepted as a cost- effective and safe method for the treatment of OA, Brander et al. and Murray and Frost reported that 19% and 30% of patients experience postoperative moderate to severe pain and, respectively, while Escobar reported that 33% of patients did not have improvement after surgery and were dissatisfied with their functional abilities at 1 year postoperation [1-3]. In addition to the high percentage of unsatisfactory functional results that have been reported, we have observed that these patients have low mood and poor compliance with rehabilitation, with apparent increased analgesic use irrespective of their operation. Although anxiety and depression have been demonstrated to have unfavourable results on postoperative knee functions, to the best of our knowledge, no study has investigated the impact of psychiatric status on comorbid pain, postoperative knee functions, and its treatment with a benzodiazepine.
Our clinical experience point out that, despite adequate surgical technique and individualized postoperative rehabilitation, patients who are unsatisfied with their results demonstrate increased use (i.e., dose) of analgesics, prolonged hospital stay, and rehabilitation. Though there are numerous proven variables that contribute to analgesic use after TKA, these can generally be classified as either surgeon-dependent or patient-dependent factors. Surgeon- dependent factors are usually technique-dependent and are relatively invariable, whereas patients psychological status remains a strong predictor or increased analgesic use and is mostly underestimated. The strong influence of depression on comorbid pain plays an important role in analgesic use after arthroplasty procedures and warrants attention [4].
Emptage et al. concluded that the principally known symptoms of knee OA (e.g., pain, tenderness, and stiffness, which are often chronic) are often associated with psychiatric disorders and this is due to prolonged conservative treatment [5]. Clinically significant depressive symptoms and anxiety frequently co-occurs with pain among these patients [6]. Patients with chronic pain symptoms are 3- to 5-times more likely to be depressed than patients without pain [7, 8]. Pain and fatigue are the most commonly unexplained physical symptoms in patients with depression and anxiety.
The above findings show that the relation between depression, anxiety, and pain becomes stronger as the severity of either condition increases. Over time, psychiatric disorders predict the onset of physical symptoms, and in turn, physical symptoms, especially pain, predict the onset of depression [9]. These individuals with depression and anxiety often present with physical complaints that are typically associated with medically unexplained pain. Although depression and chronic pain are common comorbidities, their complex molecular interaction is still not fully understood [10].
The mean prevalence rates for major depression in patients identified as having pain by study settings are: 52% in pain clinics; 38% in psychiatric clinics; and 56% in orthopaedic or rheumatology clinics [6]. According to this data the rate of depression and comorbid pain is interestingly higher in orthopaedic clinics than psychiatric clinics. Orthopaedic surgeons must keep in mind that candidates for a major joint arthroplasty may be chronic pain sufferers and experience greater pain sensation intensity, as well as more pain-related disabilities as a result of undiagnosed depression or anxiety [11, 12].
Here we hypothesize that individuals diagnosed with depression or anxiety are more prone to increased analgesic use and that use of a benzodiazepine can improve the psychological status, decrease analgesic need, and regain favourable functional outcomes after TKA.
MATERIAL AND METHODS
Medical records of 76 patients (58 female, 18 male) with a mean age of 65 ± 9.3 years (range 46-80), diagnosed preoperatively with mild-moderate depression-anxiety, with advanced stage OA according to the Kellgren-Lawrence criteria, and that have underwent TKA between the years 2009 and 2012 were analyzed in the current study. Duration of knee OA was not significant in selected patients and all met the criteria of ≥20 points according to the Lequesne Algofunctional Index and Stage 4 according to the Kellgren- Lawrence scale. All patients met the criteria for ≥16 points according to the Hamilton Anxiety scale (HAS) and 10-23 points according to Beck Depression Inventory (BDI), with impaired functional abilities according to the preoperative psychiatric evaluation. Psychiatric recommendations and treatment varied in this patient population due to the physicians’ preference. A group of patients were subjected to medical treatment while the remaining patients were observed only. Medical treatment consisted of alprazolam (Xanax™, p.o 1 g) that was initiated 2 weeks prior to surgery. Patients receiving alprazolam and postoperative intramuscular administration of Diclofenac Sodium (75 mg/3 ml) (Voltaren™) for pain control were defined as Group 1, whereas Group 2 consisted of patients only receiving observation and postoperative Diclofenac Sodium. The Lequesne Algofunctional Index, which is routinely used in our institute has five questions pertaining to pain or discomfort, one question dealing with maximum distance walked, and four questions about activities of daily living. The total questionnaire is scored on a 0 to 24 scale. Regional anaesthesia (combined spinal and epidural anaesthesia) was preferred in all patients and the duration of the surgical procedure was recorded. A posterior cruciate retaining design with cemented femoral and tibial components were used with the same surgical technique by the same surgeon. Sterile disposable tourniquets were used during all procedures. For pain management during the first 24 h postoperative period, patient-controlled epidural analgesia (PCA) was preferred in all patients. Starting from the second day, patients received 75 mg/3 ml intramuscular Diclofenac Sodium administration until the day of discharge (postoperative day 5). In our institute, the dose and frequency of Diclofenac Sodium is designed according to the patients need, with a maximum dose of 200 mg/day. As an institutional policy, knee functions are assessed routinely with the Knee Society Functional Score (KSFS) and Knee Society Score (KSS) at 1 month and 1 year postoperative follow-up, and the pain experienced is evaluated with preoperative and postoperative VAS [13, 14]. Total analgesic use (g/5 day) and correlation between HAS-BDI and postoperative analgesic use was evaluated using patients postoperative medical records. Statistical comparisons were generated using Statistical package for Social Sciences (version 11) for Windows (SPSS, Chicago, IL, USA). All data are expressed as the means ± SD. P-values less than 0.05 were considered statistically significant. The data accumulation was in adherence to the tenets of the declaration of Helsinki (revised in 2000).
RESULTS
Body Mass Index (BMI), which can affect analgesic drug metabolism and duration of OA clinical symptoms, did not vary between groups (BMI: 31 ± 7.6 kg/m2 in Group 1 and 30 ± 4.8 in Group 2, P≥0.05). Although the decrease in VAS was found to be statistically significant in both groups, postoperative total analgesic use in Group 1 was found to be 4.25 ± 0.30 g (range 4.0-5.0), whereas the same parameter was 4.81 ± 0.41 g (range 4.0-5.5) in Group 2 (p=0.01) (Fig. 1 and Table 1).
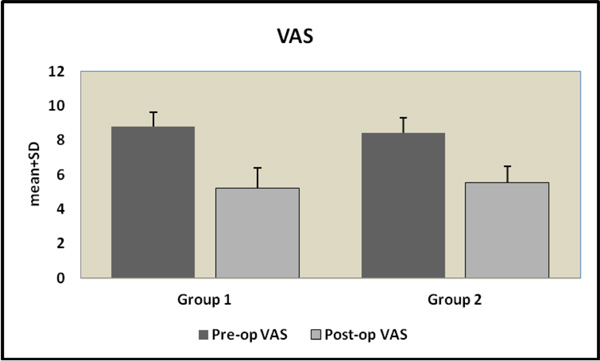
The decrease in visual analog scale was found to be statistically significant in Group 1 compared to Group 2 (p = 0.008).
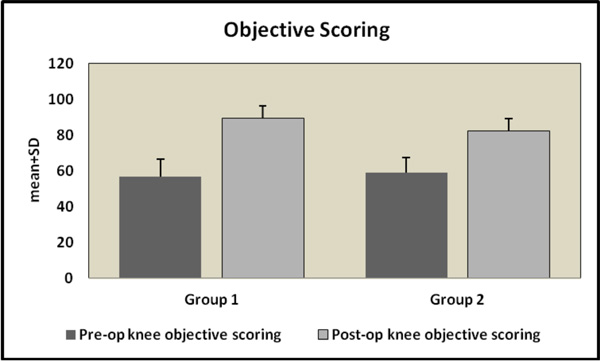
Pre-postoperative knee objective scoring (KSS) in Group 1 and 2. The mean change of KSS scoring in Group 1 patients was found to be significantly higher than in Group 2 patients.

Pre-postoperative knee functional scoring (KSFS) in Group 1 and 2. The mean change of KSFS scoring in Group 1 patients was found to be significantly higher than in Group 2 patients.
Postoperative analgesic use in Group 1 and Group 2 patients.
| Group 1 (n=38) | Group2 (n=38) | ||
|---|---|---|---|
| Postoperative Diclofenac-Sodium (gr) | Mean+SD | 4.2 ± 0.30 | 4.8 ± 0.41 |
| min-max | 4.0-5.0 | 4.0-5.5 | |
| P | 0.001** | ||
A positive correlation was identified between preoperative HAS and BDI scores, and postoperative analgesic use (g/day) in Group 1 (p=0.0001, r=0.558 and p=0.026, r=0.360 respectively). Similarly, preoperative HAS and BDI scores and postoperative analgesic use (g/day) were found to be correlated in Group 2 (respectively; p=0.001, r=0.708 and p=0.05, r=0.348 respectively). There was a significant increase in postoperative knee scores compared to preoperative levels in both groups but the mean change of KSS scoring in Group 1 patients (32.52 ± 9.62) was found to be significantly higher than in Group 2 (23 ± 8.85) ( p<0.01). Similarly, the mean change of KSFS scoring in Group 1 patients (39.34 ± 10.53) was found to be significantly higher than in Group 2 patients (23.37 ± 9.81) (Figs. 2, 3).
DISCUSSION
Stress, anxiety, depression, social support, and attitude have all been proposed as factors that influence outcome after surgical procedures [15-17]. The association between psychological state and comorbid pain in TKA patients warrants attention since it directly influences the patients compliance with rehabilitation and short– to mid-term satisfaction. Unexpectedly, the rate for major depression in patients identified as having pain by study setting in orthopaedic clinics is as high as 56% (21-89%). In the current study, 52% of our patients that underwent TKA were preoperatively diagnosed with mild-moderate depression and anxiety according to psychiatric consultation records. The observed high rate can be considered a consequence of chronic pain unresponsive to prolonged conservative treatment and related decrease in the quality of life. McWilliams et al. found a higher prevalence of depression, panic disorder, and generalized anxiety disorder in patients with arthritis-related chronic pain compared with a representative sample of patients with pain but no arthritis [18].
Similar to McWilliams, our study represents a subsection of this large population that is characterized by severe OA, accompanied by chronic pain and psychiatric disorders. Although knee OA is effectively treated with TKA in these patients, the accompanying depression or anxiety is unfortunately highly undiagnosed and untreated.
The impact of improving mild-moderate depression and anxiety on functional outcomes in patients undergoing TKA has been examined, but its effect on postoperative analgesic use combined with postoperative knee functions had not previously been addressed. The increased analgesic use in this patient population is likely due to the decreased threshold of pain sensation overtime and lack of rehabilitation compliance. We believe that the strong interaction between depression, anxiety, and comorbid pain has to be overcome with appropriate anxiolytic or anti- depressive treatment before the viscous cycle begins. In the current study we have focused on this issue and demonstrated that there was a significant positive statistical correlation between depression-anxiety scores and postoperative analgesic use in both of the study groups.
In the literature several psychological interventions (both medical and behavioural) have been proposed for the treatment of anxiety, depression, and comorbid pain, and have been found to be beneficial in terms of pain and disability [19, 20]. A small number of efficacy trials, conducted among rheumatoid patients with depression, demonstrated that antidepressant medication reduced pain when compared with placebo [21, 22]. In a recent randomized trial, rheumatoid arthritis patients with comorbid depression were treated with either paroxetine or amitriptyline. Both treatment modalities revealed similar effects on pain, depression, and disability [23].
In our institution, benzodiazepines are recommended for patients diagnosed with mild-moderate depression and anxiety accompanied by comorbid pain for two principal reasons: (1) benzodiazepines are known to be safe and effective in the short term; and (2) they enhance the effect of the neurotransmitter gamma-aminobutyric acid (GABA), which has sedative, anxiolytic, anticonvulsant, and muscle relaxant properties. This effect can be considered as an advantageous input in the treatment of both patients’ psychological status and pain in the early postoperative period. Among numerous benzodiazepines, Xanax has the advantage of maintaining an antidepressant effect as strong as tricyclic antidepressants, in addition to its strong anxiolytic effect. To the best of our knowledge, to date no study has been performed to assess the effects of a benzodiazepine to improve depression, anxiety, and postoperative analgesic use in TKA patients.
Even after an uncomplicated TKA, 20% of patients reported dissatisfaction at 1 year follow-up, with prolonged use of analgesics and suboptimal functional recovery. Psychiatric disorders that predict the onset of physical symptoms, and, in turn, physical symptoms (especially chronic pain) that predict the onset of psychiatric disorders, must be well defined in TKA patients. Identifying and treating depression/anxiety before TKA may therefore be an important strategy to improve functional outcomes. In the current study, Xanax had the advantage of affecting anxiety, depression, and related comorbid pain in a short period of time with promising favourable effects for long-term follow- up. Patients treated with alprazolam demonstrated decreased analgesic use with better VAS scores compared to the conventional treatment group. Independent from this beneficial effect, postoperative 1 month KSS and KSFS scores concluded that functional recovery was also improved in patients using alprazolam.
In conclusion, the strong association between depressive symptoms and pain suggests that joint replacement surgeons may need to incorporate into their practice an understanding of, and approach to, these conditions. We conclude that untreated depression or anxiety can be an important risk for postoperative increased analgesic use and unfavourable knee functions. Because of its strength as a predictor of outcome and its ease of use, orthopaedic clinics can incorporate the BDI and HAS into clinical history forms routinely used during the preoperative evaluation or postoperative period in patients undergoing major joint replacement surgeries. Patients who present high BDI and HAS scores can be referred to a psychiatrist for subscription of a benzodiazepine prior to surgery or during the early postoperative period. In the current study, alprazolam, with both its antidepressant and anxiolytic properties, had favourable effects on postoperative analgesic use and knee functions. This is likely due to increasing the pain threshold and overall mood in these patients. This mechanism can be used to block the strong interaction between depression, anxiety, and comorbid pain, since chronic pain is a well-known factor that contributes to prolonged analgesic use with poor functional outcomes, even after a non-complicated TKA procedure.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


