All published articles of this journal are available on ScienceDirect.
Osteochondroma-Related Pressure Erosions in Bony Rings Below the Waist
Abstract
This article investigates the clinical and radiological features of four cases of osteochondroma-related bony pressure erosion in adults. Rare imaging features of extrinsic pressure erosions on adjacent bones caused by solitary and familial forms of osteochondroma are presented. Although described to occur uncommonly in the paired bones of the lower leg, pressure erosion in the pelvic girdle is poorly understood. In this article, we discuss clinical contexts for management of osteochondroma-related bony pressure erosion in the mature skeleton.
INTRODUCTION
Osteochondroma is the most common benign bone tumor and represents a developmental exostosis rather than a true neoplasm. The metaphysis of long bones is the most frequent site [1, 2]. The majority are sporadic and solitary in nature, although multiple tumors present in hereditary multiple exostoses (HME), the less common familial form. The tibia has an incidence of 15 to 20% and is second only to the femur as the most common bone. By contrast, osteochondromas occur only 5% of the time at the pelvis and arise most frequently at the iliac crest [3-5].
There are several well-known osteochondroma-related bony complications. Most patients present with a cosmetic deformity related to a painless and palpable benign osteochondroma, although the most feared complication to rule out is malignant transformation to chondrosarcoma [3]. Painful fractures also occur and subsequent non-union has been described as a cause of persistent symptoms [4, 6]. Osteochondromas also cause developmental problems unique to children and adolescents. Leg length discrepancy, angular deformity, and abnormal joint motion are bone- related complications of the growing skeleton [4].
Osteochondromas also cause impingement upon adjacent structures. Soft tissues are more commonly affected than bones, and vascular compromise, nerve compression, and reactive bursal formation are well-known complications [3, 6]. By contrast, direct mechanical pressure effects on other adjacent bones are uncommon. The osseous structures most likely to sustain an extrinsic pressure erosion from an adjacent osteochondroma are the bones of a ring structure, since a tumor arising from one bone will impress the surface of the opposing bone [7]. The lower leg and pelvic girdle are two such ring structures below the waist. The tibia and fibula form a ring structure and are directly bound by strong proximal and distal ligamentous complexes at the lower leg. Overall, osteochondroma-related bony pressure erosions are uncommon events, but occur most frequently at the paired bones of the lower leg [3]. The pelvic girdle is another ring of bones with three major articulations connected by strong ligamentous complexes. Posteriorly, the sacroiliac joints are formed by articulations between the sacrum and iliac bones. Anteriorly, the pubic bones articulate at the symphysis pubis, where the pubic bodies are directly opposed. Osteochondroma- related bony pressure erosion at the pelvis is rare.
In this article we present four cases of osteochondroma- related bony pressure erosion in adults. We describe clinical contexts for conservative management at the lower leg and pelvis in the mature skeleton.
CASE REPORT
Case 1
A 27-year-old male with no significant past medical history presented to his primary care physician with a three- week history of intermittent left anterior shin pain. He played soccer regularly three times a week, and stated that he had been recently kicked several times in his lower legs. He denied edema, erythema, paresthesias, or difficulty walking. The patient did admit to awareness of a painless lump at the lateral aspect of his knee for several years. On physical examination he had full range of motion and strength of his left lower extremity. A firm, non-tender palpable mass was present on palpation of the fibular head. Radiographs revealed a large tibial osteochondroma at the knee which was associated with a large fibular erosion (Fig. 1a, b). The patient was referred to orthopaedics and magnetic resonance imaging (MRI) was obtained to further characterize the abnormality (Fig. 2a-c). Besides the erosion, no other feature worrisome for malignant transformation was present. The cartilage cap of the osteochondroma showed no abnormal thickening. The absence of edema in the fibula also signaled that the erosion was chronic in nature, and that an active erosive process was not present. Since his pain was most attributable to a recent soccer injury and not to malignant transformation, the patient was not offered further intervention or surgical management. Following a trial of conservative management, the patient returned to his normal activity level with a resolution of pain. He has remained asymptomatic after 3 years of follow up.
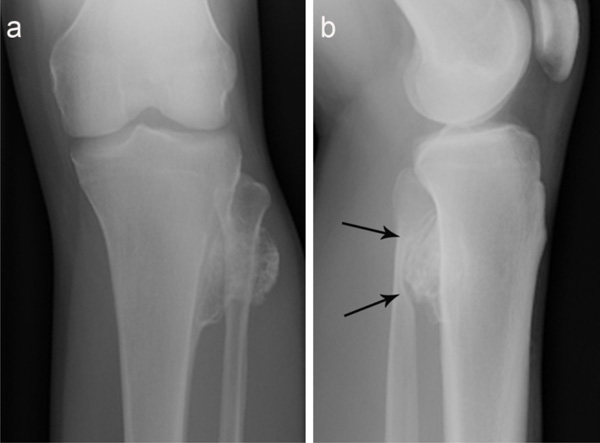
(a) Anteroposterior radiograph of the left knee shows a large solitary broad-based osteochondroma arising from the metadiaphysis of the tibia and projecting towards the proximal fibula. (b) Lateral radiograph of the left knee demonstrates abnormal contact between the osteochondroma and the fibula which created a large pressure erosion involving > 50% the width of the fibular metadiaphysis (arrows).
(a) Axial Intermediate-weighted turbo-spin echo (TSE), (b) sagittal T2-weighted TSE fat suppressed, and (c) axial STIRweighted magnetic resonance (MR) images of the left knee show a tibial osteochondroma producing a large chronic-appearing pressure erosion involving > 50% the width of the proximal fibular metadiaphysis (long arrows). No bone marrow edema is present at the fibula. The maximum thickness of the cartilage cap of the osteochondroma was 1 cm. Nonspecific feathery edema is identified in the anterior muscular compartment of the lower leg (short arrow).

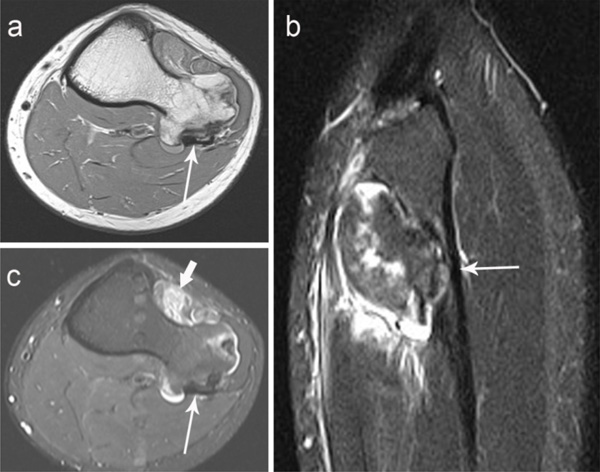
(a) Anteroposterior and (b) oblique radiographs of the right ankle show a distal tibial osteochondroma associated with a smooth-appearing pressure erosion at the medial cortical surface of the adjacent fibular diaphysis (long arrows). (c) Anteroposterior of the left knee of the same patient demonstrates a synostosis from “kissing” tibial and fibular osteochondromas (short arrow). There is a transverse lucency with peripheral callus formation at the base of a distal femoral osteochondroma (asterisk) resembling an old nondisplaced fracture.
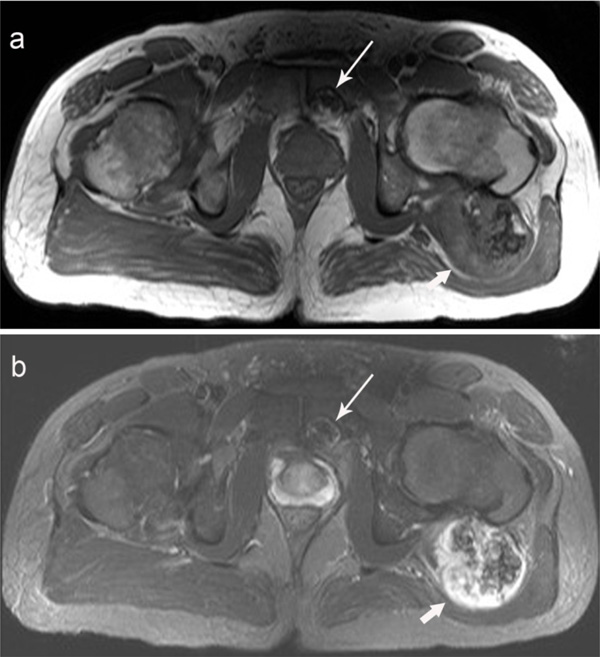
Anteroposterior radiograph of the pelvis shows a large mineralized mass superimposed over the left proximal femur and a widened appearance of right femoral neck consistent with osteochondroma formation. In addition, a small round mineralized mass projects over the left pubic body with an associated pressure erosion (arrows).
(a) Axial T1-weighted spin echo and (b) axial T2- weighted TSE fat suppressed MR images demonstrate the large symptomatic osteochondroma arising from the posteromedial aspect of the left proximal femur (short arrow) which displaces the left gluteus maximus muscle. Also seen is a small osteochondroma causing a pressure erosion on the posterior surface of the left pubic body (long arrow). No bone marrow edema is associated with the left pubic body erosion.
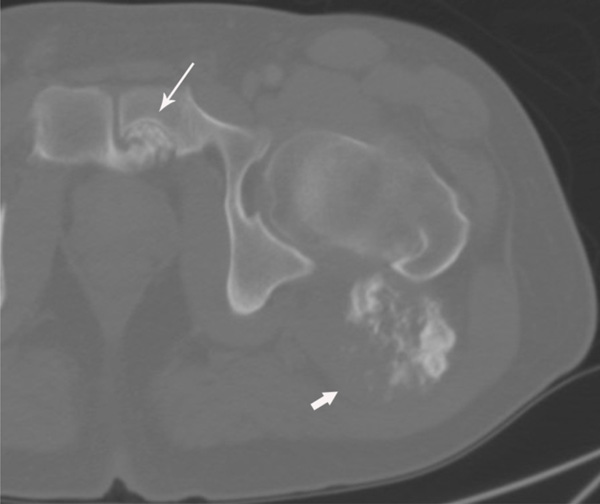
Axial non-contrast computed tomography (CT) image of the left hip shows the smooth bony pressure erosion of the left pubic body (arrow) is caused by an osteochondroma extending from the right pubic body. The large symptomatic osteochondroma is associated with the posteromedial aspect of the left proximal femur (short arrow).
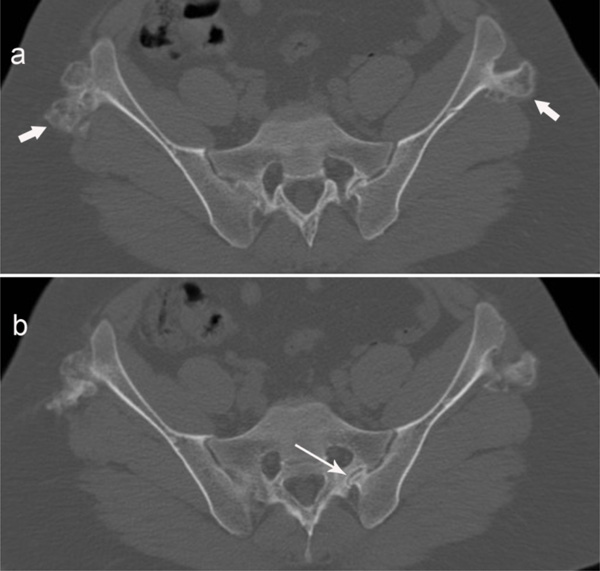
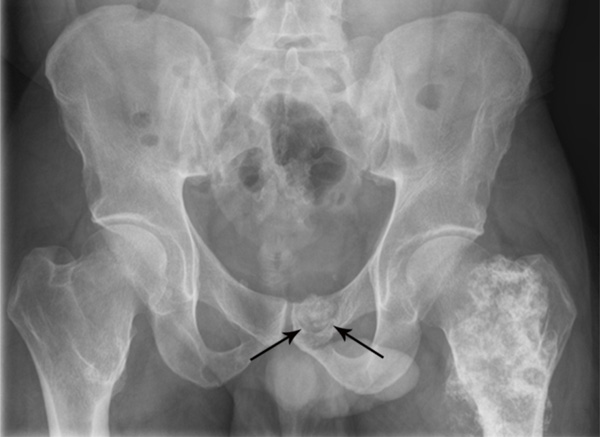
(a) and (b) show two sequential axial non-contrast CT images through the pelvis in a patient with hereditary multiple exostoses. A small osteochondroma from the left ilium crosses the left sacroiliac joint and creates a small pressure erosion with welldefined margins at the sacrum (long arrow). Additional osteochondromas are seen near both iliac crests (short arrows).
Case 2
A 21-year-old male with a history of HME and acute lymphoblastic leukemia presented to the oncology clinic with a two-day history of fever and polyarthralgia. He complained of pain, redness, swelling and stiffness in his wrists, hands and hips initially, which quickly progressed to involve his shoulders, elbows, knees and ankles. He had a past history of prior excision of symptomatic osteochondromas in childhood, but did not report any recent tumor-related complications as an adult.
On physical exam, the patient had a temperature of 39.2oC and shaking chills. His elbows, wrists, knees and ankles were edematous, erythematous, warm and tender to palpation. He had decreased range of motion secondary to pain in his elbows, wrists, hands, hips and ankles. The patient received a dose of vancomycin and meropenem at the oncology clinic and was admitted to the hospital. Radiographs of his upper and lower limbs revealed multiple osteochondromas consistent with HME. Radiographs of the right ankle showed a tibial osteochondroma adjacent to a chronic-appearing pressure erosion with smooth margins at the distal fibula (Fig. 3a, b). The osteochondroma otherwise lacked the aggressive features of associated soft tissue component calcifications or internal bony ill-defined areas of radiolucency or mineralization. Radiographs of the left knee also showed other atypical bone-related complications presenting in this patient (Fig. 3c). During the hospital admission, orthopaedic and infectious disease consultations were performed. The osteochondromas were found to be non- contributory to the patient’s symptoms. The patient received antibiotics for one week during his inpatient stay, during which time his fever, global joint pain and stiffness resolved. At the time of discharge he was without joint complaints. The osteochondroma-related bony pressure erosion was considered an incidental finding of a chronic nature and treatment was conservative. The patient remains without complaints or physical limitations at the right lower leg after 9 months of follow up.
Case 3
A 41-year-old male with a history of HME presented to his neurosurgeon with new-onset of left buttock pain, following recent craniotomy and surgical excision of a right cerebellar pontine angle schwannoma. He had a past surgical history of prior removal of symptomatic osteochondromas from both lower limbs as a child. He had neither left hip, pelvic or buttock pain, nor limited physical activity as an adult prior to his recent brain surgery. He had been aware of a bony prominence at his left buttock for many years, and this mass was otherwise without symptoms for as long as he could remember. His pain began following the craniotomy, during which time he had been placed in the left lateral decubitus position for the procedure. The patient was referred to orthopaedics for further evaluation of his buttock pain. On physical examination, he had a large firm left buttock palpable mass, which was tender to gentle percussion. The mass also moved in concert with the left femur, with limited left hip internal and external rotation. A radiograph of the pelvis showed a large mineralized mass associated with the left femur, and also the incidental finding of a small osteochondroma and pressure erosion at the left pubic body (Fig. 4). Follow up MRI (Fig. 5a, b) and computed tomography (CT) (Fig. 6) characterized further the extent of the osteochondromas. The MRI and CT showed no aggressive features of the pubic osteochondroma. The cartilage cap was only a few millimeters thick, and the margin of the erosion was smooth with an absence of bone marrow edema in the left pubic body. The symptomatic left femur osteochondroma was resected. The right pubic body osteochondroma, however, was treated conservatively, and the patient has remained asymptomatic at the symphysis pubis after 6 years of follow up.
Case 4
A 29-year-old male with a history of HME presented for tumor surveillance of his upper and lower limbs two years after the removal of a symptomatic osteochondroma. He had a past surgical history of multiple osteochondromas removed from his right lower leg, left ankle and right wrist. He had no known symptoms on the day of imaging. CT showed multiple osteochondromas in his upper and lower limbs, with an intra-articular left ilium osteochondroma extending across the left sacroiliac joint and causing a left sacral wing pressure erosion (Fig. 7). The erosion was well-defined, with no other signs worrisome for malignant transformation. The bony impingement of the osteochondroma at the left sacral wing was diagnosed as a chronic incidental finding, and management was conservative. The patient has remained asymptomatic after 5 years of follow up.
DISCUSSION
Osteochondroma-related bony pressure erosions are a diagnostic dilemma when initially discovered. However, our case presentations highlight that conservative management is a reasonable alternative to surgical intervention when these abnormalities present incidentally at the pelvic girdle and lower leg in asymptomatic adults.
Osteochondromas are tumors which develop from ectopic cartilaginous precursors in the subperiosteum following the anomalous separation of these cells from the edge of an immature growth plate [2]. The metaphysis of the long bone is by far the most common site for this to occur due to the proximity of the physis and the biology of the growing skeleton [1]. Osteochondromas enlarge during childhood and adolescence through the process of endochondral ossification of the cartilage cap during skeletal maturation, in a fashion parallel to the growth of a long bone from an epiphyseal growth plate [3].
Symptomatic osteochondroma-related bony pressure erosions of adjacent bones are uncommon, but proximal or distal tibial osteochondromas producing pressure erosions on the fibula, or vice versa, have been described [7-9]. Osteochondroma-related bony pressure erosions occur least often at the proximal fibula and most often at the distal fibula and proximal tibia [7]. If two opposing osteochondromas directly abut one another, a synostosis is formed instead of a pressure erosion. These types of lesions are referred to as kissing osteochondromata and occur most frequently in HME [7]. In the case of bony pressure erosions, continued enlargement of the causative osteochondroma is expected to occur in the growing immature skeleton, and surgical intervention is indicated to alleviate pain and to prevent growth disturbance and joint deformation [8-10].
The behavior of benign osteochondromas in adulthood differs from those encountered in childhood and adolescence. Typically, osteochondromas do not enlarge following the closure of growth plates and the arrival of skeletal maturity [2, 7, 11]. Many asymptomatic osteochondromas are discovered incidentally in adults, and even patients with HME may be unaware of the presence of their osteochondromas if they are without symptoms [5]. In general, routine follow up is not indicated for asymptomatic osteochondromas discovered after skeletal maturity [4].
Malignant transformation occurs in 1% of solitary tumors and up to 5% in patients with HME, and worrisome features include pain, tumor enlargement, cartilage cap proliferation, suspicious mineralization, extraosseous soft growth and bone destruction [3]. Pain and enlargement of an osteochondroma after skeletal maturity is suspicious for malignant transformation, since growth of a benign osteochondroma is rare in adults [3, 6, 10, 11]. Abnormal proliferation of the cartilage cap to a thickness greater than 1.5 cm is also concerning, since cartilage caps typically regress after skeletal maturity [3, 7].
Adults who present with osteochondroma-related bony pressure erosions require careful evaluation for other symptoms and signs of malignant transformation. The isolated finding of a bony pressure erosion in an otherwise asymptomatic patient initially may create confusion when found incidentally, but the discovery of a bony pressure erosion in an adult with pain presents a greater diagnostic dilemma even when all other imaging features of the osteochondroma are otherwise benign [12]. In these contexts, clinical history plays an important role in determining whether or not an isolated osteochondroma-related bony pressure erosion is an incidental finding versus a worrisome development. Symptoms directly attributable to an osteochondroma without any other explanation are highly suspicious for malignant transformation in the mature skeleton, and surgical resection is indicated [3, 6, 10, 11]. However, care should be taken when deciding to remove asymptomatic tumors, since the surgical excision of benign osteochondromas is associated with a 12.5% complication rate [13]. The most common complication is neurapraxias, following iatrogenic nerve injury. Compartment syndrome, vascular injury and fracture are additional reported surgical complications [13].
Non-malignant bony complications of osteochondroma in the lower leg, although uncommon, include pain, pressure erosion, synostosis formation, pathologic fracture, altered joint motion, tibiofibular diastasis and growth disturbance [7-1, 14]. However, osteochondroma-related mass effects on adjacent bones at the pelvis are rare, and only a few case reports exist in the literature. Guner et al. and Gaillard both reported cases of osteochondromas with associated intra-articular mass effect at the sacroiliac joint treated with surgical excision [15, 16]. Two other case reports described symptomatic extra-articular bony erosions at a sacral wing and sacral neuroforamen, respectively [17, 18]. In contrast to the posterior pelvis, reports of osteochondroma-related symphysis pubis complications describe impingement of only soft tissue structures and not bony pressure erosion [6].
We present four cases of osteochondroma-related bony pressure erosion treated with conservative management. Each tumor lacked any additional aggressive imaging features to suggest malignant transformation. Only Case 1 had symptoms attributable to the location of the osteochondroma, and this case highlights the need to correlate clinical history with symptoms. The patient’s pain in Case 1 was secondary to being kicked in the leg while participating in sports and resolved with time.
CONCLUSION
We have described rare osteochondroma-related bony pressure erosions in adults at the pelvic girdle and lower leg. Our case presentations highlight that conservative management is a viable alternative to surgical intervention for the mature skeleton in the setting of asymptomatic bony pressure erosions. Osteochondroma-related bony pressure erosion, found incidentally without symptoms and additional aggressive imaging features, most likely develop before skeletal maturity is reached and are chronic in nature. Surgical intervention remains a future option for adults who later develop pain, pathologic fracture or additional imaging features worrisome for malignant transformation.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


