All published articles of this journal are available on ScienceDirect.
Current Controversies of Alignment in Total Knee Replacements
Abstract
Total knee replacement is an increasingly popular operation for end stage knee arthritis. In the majority it alleviates pain and improves function. However up to 20% of patients remain dissatisfied, even with well-aligned and secure implants.
Restoration of a neutral mechanical axis has traditionally been strived for, to improve both function and implant survival and there is historical data to support this. More recently this view has been questioned and some surgeons are trying to improve the function and outcomes by moving away from standard alignment principles in an attempt to reproduce the kinematics of the pre-arthritic knee of that individual. Others are using computers, robots and patient specific guides to improve accuracy. This article aims to review the traditional alignment concept and the newer techniques, along with the evidence behind it.
INTRODUCTION
Over 90,000 primary total knee replacements (TKRs) were performed in the UK in 2013 [1]. Improvements in surgical technique and prosthesis design continue to enhance long-term outcomes. However mechanical demands and patient expectations continue to rise and numerous studies suggest up to a 20% dissatisfaction rate [2, 3]; the causes of which remain poorly understood.
Traditionally it has been widely accepted that one aspect of surgical technique that significantly affects patient satisfaction and implant survival is the correct positioning and alignment of the components [4]. Restoration of the mechanical axis has been strived for, with coronal alignment and its effect on function and survival, being studied more than any other parameter in knee replacement surgery. Despite this controversy still exists in optimal component alignment. The introduction of computer assisted surgery, patient specific designs and kinematic knee alignment has added to this controversy.
MECHANICAL AXIS DEFINITION
The mechanical axis of the femur is defined as a line drawn from the centre of the femoral head to the centre of the knee. The mechanical axis of the tibia is a line from the centre of the proximal tibial plateau to the centre of the talus. Both lines are drawn on long leg weight-bearing radiographs [5, 6] (see Fig. 1). The mechanical axis of the lower limb is defined as a line drawn from the centre of the femoral head to the centre of the talus (Macquet’s line).
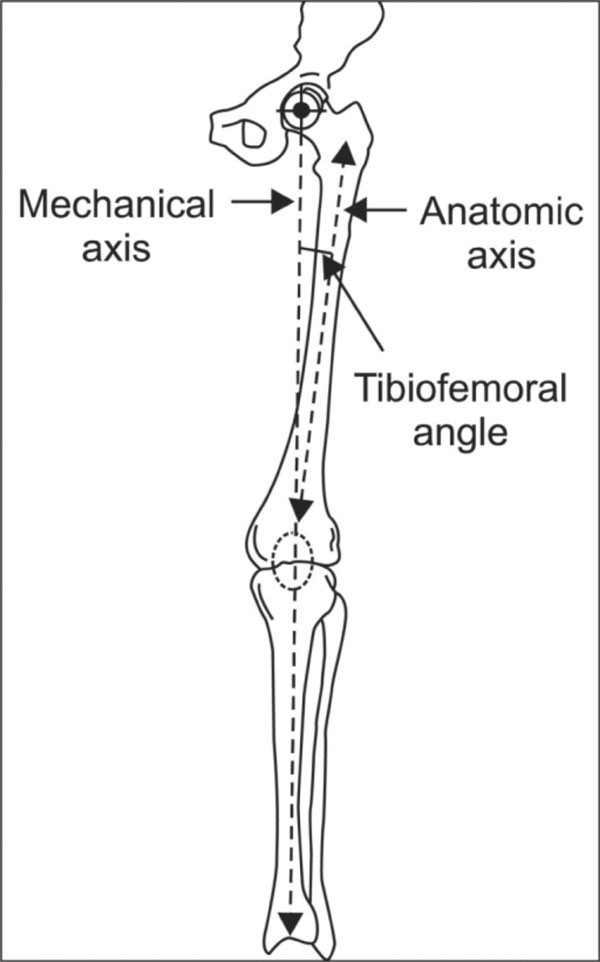
Alignment of the lower limb. (Permission from Knee Surgery and Related Research 2012 June 24(2); 61-69).
Restoration of Macquet’s line to neutral has been the traditional goal of TKR, ensuring the centre of the femoral and tibial components both lie along the mechanical axis of the lower limb in both the coronal and sagittal planes.
NEUTRAL MECHANICAL ALIGNMENT
Most surgeons still agree, and it is traditionally believed, that the postoperative alignment should be to within 0° +/- 3° of the mechanical axis [7]. This is thought to improve the durability of the TKR; the evidence of which has been founded on data from clinical, retrieval and finite element studies.
Historically, varus results fared worse and valgus alignment was often recommended [8-11]. In 1991 Jeffrey et al. [12] popularised the restoration of the mechanical axis to neutral based on long leg radiographs. 115 TKRs were studied: where the mechanical axis was neutral, the incidence of loosening was 3%; where the mechanical axis was in varus or valgus, the loosening rate increased to 24%. Ritter et al. [13] in 1994 confirmed Jeffrey’s findings in a series of 421 consecutive TKRs. The postoperative alignment was categorised into three groups: valgus (≥9° valgus), normal (5-8° valgus), and varus (≤4° valgus to any amount of varus). Varus malalignment fared worst with five failures, compared to three in the neutral group and zero in the valgus group. Kaplan-Meier survival curves of the implants showed a statistically significant difference between the valgus and varus groups and between the normal and varus groups. The authors concluded: “the surgeon should align a knee prosthesis in neutral or slight anatomic valgus to give the patient the best chance for long-term survival.”
All of the studies mentioned above used short-leg x-rays and older designs of components. Many were also limited by small numbers of patients.
More recently Berend et al. [14] in 2004 showed similar findings to Jeffrey and Ritter et al. with an increased rate of failure in TKR where the tibial component was placed in more than 3.9° of varus and this was exacerbated if body mass index (BMI) was >33kg/m2. In a continuation of the same study Fang et al. [15] in 2009 looked at 6070 primary TKRs retrospectively and grouped the patients into varus, neutral and valgus groups. They found the highest rate of implant survivorship in the neutral group (2.4° to 7.2° valgus). The revision rate for this group was 0.5% compared to 1.8% (varus) and 1.5% (valgus) - both significantly different from the neutral group. At 20 years follow up, the implant survival rate remained statistically significant: 99% in the neutral group, 95% in the varus group and 97% in the valgus group.
Collier et al. [16] in 2007 looked at the wear of the polyethylene tibial bearing in TKRs retrieved at the time of revision surgery or death of the patient and found varus alignment of the TKR to be one of the three greatest risk factors for polyethylene wear. The other two were patient age and shelf age of the polyethylene insert.
In a randomised control trial comparing conventional versus computer-assisted TKR [17] the authors found knees aligned with a mechanical axis within 3° of neutral had superior International Knee Scores (IKS) and Short-Form 12 (SF-12) scores post-operatively. Similarly Longstaff et al. [18] looked at alignment of TKRs on a computed tomography (CT) scan at 6 months post-operation and found TKRs with a neutral mechanical axis had better functional scores at one year and a shorter inpatient stay.
IS VARUS ALIGNMENT THAT BAD?
Bonner et al. [19] in 2011 studied 501 consecutive TKRs between 1987 and 1997 using long- leg AP weight bearing radiographs. They stratified the patients into ‘aligned’ (neutral mechanical axis ±3°) and ‘malaligned’ (mechanical axis deviated from neutral by more than 3°). They found that implant survival was slightly higher in the aligned group but the difference was not statistically significant (using Kaplan-Meier survival analysis). They concluded “the relationship between survival of a primary TKR and mechanical axis alignment is weaker than that described in previous reports”.
Parratte et al. [20] studied implant survival in 398 primary TKRs from 1985 to 1990. They also divided the knees into aligned and malaligned groups using the same criteria as Bonner. They found no significant difference between the two groups in the 15-year Kaplan-Meier implant survival rate. They stated that a description of TKRs as aligned versus malaligned was of little use in predicting durability.
Others have suggested the same. Morgan et al. [21] retrospectively studied a series of primary TKRs using long-leg radiographs and classified them according to tibiofemoral angle into: a neutral group (4° to 9° anatomic valgus); a valgus group (9.1° and above) and a varus group (3.9° and below). There was no difference in survival among the 3 groups (using Kaplan-Meier analysis) and the authors state “...aseptic failure of a total knee is multifactorial and that coronal tibio-femoral alignment may not be as important a cause of failure as originally thought.”
Matziolis et al. [22] in 2010 retrospectively reviewed a cohort of 218 patients and identified the most varus malaligned TKRs. They then compared these (30 knees) to a control group matched for implant, age and sex from the rest of the cohort for radiological signs of loosening and clinical outcome (Knee Society Score (KSS), Western Ontario and McMaster Universities Arthritis Index (WOMAC), the Short Form-36 (SF-36); active and passive range of motion of knees). They found no evidence that varus malalignment led to a worst medium-term clinical or radiological outcome than the neutrally aligned knees.
Ritter et al. [23] similarly looked at implant survivorship versus:
- Anatomical alignment of each component
- Overall anatomical alignment
- Neutral alignment but both components malposit-ioned (i.e. tibial component placed in malalignment to compensate for malalignment of femoral component)
They found a statistically significant increase in aseptic failure rates in three groups: where the femoral component is aligned in >8° anatomic valgus, a varus tibial component and when one component was placed in malalignment in order to compensate for the malalignment of the other component. Overall varus alignment was not associated with an increase in failure rate.
Magnussen et al. [24] retrospectively studied 553 primary TKRs performed on patients with pre-operative varus. They found that post-operative lower limb varus malalignment did not produce lower International Knee Society (IKS) scores compared to post-operative neutral or valgus alignment. There was also no significant difference in the revision rate between the post-operative varus and neutral groups, although as the authors point out the revision rate at 4.7 years median follow up was expectedly low and a limitation of the study. They did note that in those with substantial pre-operative varus (more than 10 degrees), residual varus alignment was actually associated with improved IKS scores.
IS VARUS ALIGNMENT GOOD?
Belleman et al. [25] studied 250 asymptomatic adults between the ages of 20 and 27 years and found an incidence of constitutional mechanical varus alignment (more than or equal to 3 degrees) in 32% of men and 17% of women. They found a relationship between varus knees and heavy sports activity (postulating the Hueter-Volkmann principle as a causal mechanism). They point out that there is likely a significant proportion of the normal population with varus lower limb alignment. These patients with so-called ‘‘constitutional varus’’ have been like that since early adulthood and correcting them to neutral mechanical alignment with a TKR may in fact be undesirable and would likely require a significant degree of medial soft tissue release.
Echoff et al. [26] provided further evidence in anatomic variation in lower limb alignment. They looked at 180 normal, asymptomatic knees using a CT scanogram and showed large deviations from a neutral mechanical axis, with nearly 45% of those in varus and almost 29% of those in valgus deviating by more than 3 degrees from neutral.
Vanlommel et al. [27] published a midterm follow-up of 5-9 years in 172 TKRs with pre-operative medial arthritis and varus alignment. Post-operatively the patients were classified into mild varus, severe varus (more than 6 degrees) and neutral alignment). The mild varus group had the greatest improvement in Knee Society Scores (KSS) and WOMAC index, showing a better clinical and functional outcome compared to the severe varus and neutral groups. They suggested that slight undercorrection might be associated with better outcomes when compared with restoration to neutral. They also found no survival disadvantage in the mid-term.
Although a neutral mechanical alignment is still a reasonable target for a successful TKR, the evidence for it is not conclusive and overall varus alignment does not necessarily lead to a lesser outcome, particularly for patients with a preoperative varus knee.
KINEMATIC ALIGNMENT
Kinematic alignment has been popularised by Howell in the USA in an attempt to address the high rate of patient dissatisfaction after TKR and the wide variety of pre-operative alignments described. It involves the individualisation of alignment of components using pre-operative imaging and computer software. The goal is to achieve pre-arthritic leg alignment through the restoration of the axes of rotation. It challenges the traditional alignment principles of restoring a ‘normal’ mechanical axis; using the transepicondylar axis as the flexion / extension axis, which in one report has been recognised to actually lie proximal and anterior to the transepicondylar axis [28]; externally rotating the femoral component and soft tissue balancing.
Kinematic alignment is achieved by obtaining a standardised protocol MRI of the knee with the plane of the oblique sagittal image perpendicular to the primary axis in the femur about which the tibia flexes and extends. Software is then used to create a 3-dimensional knee model. The arthritic model is then ‘normalised’ by filling in articular defects and equalising the articular gaps. Equalising the gaps, in theory, should restore the joint line and the alignment of the knee and lower limb. An algorithm decides on the best-fitting femoral component to the ‘normal’ femur. The software sets the AP axis of the tibial component perpendicular to the flexion-extension axis of the femoral component, which kinematically aligns the two components. Specific guides are created that fit onto the arthritic knee to make the bone cuts. The knee is consequently restored to it pre-arthritic alignment (whether this be neutral, valgus or varus).
Dossett et al. [29] conducted a randomised control trial of kinematically aligned TKRs versus mechanically aligned TKRs with 41 patients in each arm. At 6 months post-operatively they found improved pain relief, function and range of movement in the kinematic group compared to the mechanically aligned group. This is the only randomised control trial to date comparing the two methods.
Howell et al. [30] performed a study on 214 kinematically aligned knees over 31 to 43 months follow up and found an aseptic failure rate of zero and no difference in WOMAC (mean 92) and Oxford Knee Scores (mean 43) between different degrees of alignment (varus, valgus, neutral). The same group [31] also followed up 219 kinematically aligned knees over 6 years and found a failure rate of 2% with no significant difference between valgus, varus or neutrally aligned implants and average Oxford Knee Score of 43 and WOMAC of 91. Howell et al.. concluded that varus alignment in kinematically aligned knees has no adverse effect on outcome and that kinematic alignment is perhaps an alternative to mechanical alignment in TKR.
The major concern with kinematic alignment is the lack of any long-term outcome data. Another concern is whether the process of kinematic alignment consistently delivers accurate kinematic alignment of the limb due to sources of error at each stage of the process: the MRI image (proper alignment, motion artefact, image noise); the computer generation of the 3-D knee models; shape-matching of the femoral component; manufacturing the patient-specific cutting guides; and surgical technique. Reported benefits of kinematic alignment are shorter operating times, reduced number of intraoperative instrument trays and reduced recovery time [32, 33] but these must be weighed against the length of time taken to produce the cutting guides and increased costs.
COMPUTER ASSISTED NAVIGATION
In an attempt to aid surgeons accurately reproduce optimal alignment computer assisted navigation systems have been developed. There are various systems available that utilize fixed markers and techniques to reference the 3-dimensional shape of the bones within the surgical field combined with spatial recognition software to produce a computerized “virtual” model of the limb. Once registered, the computer display will guide the surgeon’s bony cuts to achieve the desired alignment in the sagittal, coronal and axial planes. Theoretical advantages are accurate and reproducible bone cuts and therefore correct implant alignment.
At present, however, the literature contains conflicting results. A number of publications [34-37] confirm more accurate implant positioning on post-operative imaging (utilizing both plain radiographs and CT reconstructions) when performed with intra-operative navigation, in comparison to conventional techniques.
A randomized, multi-centre trial comparing computer assisted versus conventional surgery [38] found that functional results were marginally better at three months and one year and that they were able to achieve more predictable mechanical alignment and tibial slope in the navigated cases. The surgery did take on average 20 minutes longer. However, a similar study, that also showed improved alignment in the navigated cases, showed no functional difference between the cohorts at 2 years of follow-up [39]. Finally, one trial of bilateral TKRs, one performed conventionally and one with navigation, concluded that computer-assisted navigated TKRs did not result in more accurate orientation and alignment of the components than a conventional technique [40].
Recent literature reviews [41-43] conclude that navigated knee replacement provides few advantages over conventional surgery on the basis of radiographic end points and unclear clinical benefits with only a few short and medium- and no long-term studies demonstrating improved clinical outcomes using navigated TKR. They also note that there is an associated higher cost and longer operating time with computer assisted surgery.
The difficulty in proving a difference between the techniques may be due to a lack of long-term follow-up but could also be explained by the generation of knee replacements being used - as the functional mechanics of knee replacement design improve, accurate implant position may become more crucial and hence navigation may become more useful in the future. Currently, further research and long-term studies are required to determine the best indications and uses for navigated surgery.
ROBOTIC SURGERY
This technique combines computer navigation with a robot that performs the bony resection (with a high-speed burr) under the control of a surgeon. This requires pre-operative templating from a CT scan of the knee. The robotic burr will not deviate outside the defined cutting window or axes of resection, theoretically producing more accurate and safer surgery.
A small number of publications [44-46] have looked at robotic-assisted surgery and achieving a consistent mechanical alignment, accurate rotational alignment of the femoral component, individualisation of the distal femoral resection angle and a reduction in the number of mechanical axis alignment outliers. They also noted accurate machining of bone surfaces with the milling device and maintenance of bone temperature during machining to prevent bony injury. These factors are postulated to improve implant survivorship due to reduced implant wear rates; but there remains no evidence to support this at present.
It must also be considered that currently robotic surgery requires an added dose of radiation from the CT scan, increased operating costs, extended operating times and with no current evidence of improved patient functional outcomes, it is difficult to justify its use outside of experimental studies and research institutions.
PATIENT SPECIFIC INSTRUMENTS (PSI)
A heavily marketed technique in which the individual patient anatomy is determined from pre-operative imaging (requiring Magnetic Resonance Imaging (MRI) or CT scans of specific sequences), allowing a unique, disposable cutting block to be manufactured. These blocks utilise the individual anatomy, including osteophytes and bony defects to fit in the correct orientation, theoretically allowing pre-planned bony resection without the need for standard intra-operative cutting guides. Specific blocks should require fewer trays of kit, leading to greater operative efficiency and are expected to reduce operative time and produce accurate, reproducible bone cuts.
At present, there is limited data regarding this technique. Three recent randomized trials [47-49] showed no difference in alignment between PSI and conventional techniques, with a similar number of mechanical axis outliers. A recent systematic review [50] draws similar conclusions and states that PSIs have not clearly been shown to improve overall surgical efficiency or the cost-effectiveness of TKR. Mid- and long-term data regarding PSIs effect on functional outcomes and component survivorship do not exist and short-term data are scarce. Limited available literature does not clearly support any improvement of postoperative pain, activity, function, or ROM when PSI is compared with traditional instrumentation.
With these publications in mind, it is hard to support the widespread use of PSI at present except in cases with extra-articular deformities around the knee [51].
CONCLUSION
Technological advances in knee arthroplasty have led to increasing numbers of joint replacements per year but controversy remains over the optimal alignment, and patient dissatisfaction remains a significant concern. It is well established that sagittal and axial malalignment result in early failure and dissatisfaction. Optimum coronal alignment however continues to be debated. Traditionally, restoration of the mechanical axis has been strived for with historical studies suggesting neutral or valgus alignment is preferable over varus. Computer navigation and robotic surgery may improve alignment but functional and long-term outcome benefits have not been proven. Equally the evidence is lacking for the widespread use of patient specific guides.
Neutral mechanical alignment in native knees is uncommon and some authors have suggested replicating the pre-arthritic knee with kinematic alignment or aiming for overall varus alignment in those with ‘constitutional varus’. There is increasing evidence to suggest that varus malalignment is not as bad as previously thought and does not lead to early failure; in fact functional outcomes may be improved by slight under-correction to neutral in varus knees.
In the absence of good long-term data most authors would still suggest a neutral mechanical axis still remains the optimal alignment and should be the benchmark against which new alignment targets are measured against.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


