All published articles of this journal are available on ScienceDirect.
Treatment of Unstable Intertrochanteric Fractureswith Proximal Femoral Nail Antirotation II: Our Experience in Indian Patients§
Abstract
Introduction:
Unstable intertrochanteric fractures are difficult to manage and the choice of implant is critical for fracture fixation. The purpose of this study was to evaluate the functional and radiological outcome of proximal femoral nail antirotationII (PFNA II) in the treatment of unstable intertrochanteric fractures.
Materials and Methods:
We reviewed 45 patients of unstable intertrochanteric fractures, who were treated with the PFNA II between 2011 and 2013. Of which, 3 patients were died within 6 months of follow up. Hence, 42 patients were available for the study including 26 men and 16 women. The mean age was 61 years (range, 35 -90). Clinical evaluation was done using Harris hip score. The position of the blade in the femoral head was evaluated using Cleveland zones and tip apex distance. The fracture reduction was assessed using the Garden Alignment Index and postoperative fracture gap (mm) measurement.
Results:
The mean follow up period was 15.3 months (range, 9-27). Excellent to good results were accounted for 78% of cases according to Harris hip score. No cases of cut out or breakage of the implant noted. Implant removal was done in 2 patients due to persistent anterior thigh pain.
Conclusion:
We recommend PFNA II for fixation of unstable intertrochanteric fractures with less operative time and low complication rate. However, proper operative technique is important for achieving fracture stability and to avoid major complications.
INTRODUCTION
Intertrochanteric fractures commonly occur in elderly patients with osteoporosis and its incidence will continue to rise due to the increasing life expectancy. The main aim of surgery is to mobilize the patient early. It is crucial to use an implant that is minimally invasive, allows early weight bearing, and has low complication rates [1, 2]. The types of implant used in these fractures have been divided into extramedullary implants and intramedullary nails. The choice of implant is mainly determined by the fracture pattern (stable or unstable). Unstable intertrochanteric fractures are those with major disruption of the posteromedial cortex because of comminution or are fractures with reverse oblique patterns or fractures with subtrochanteric extension. Fractures without posteromedial cortex disruption or subtrochanteric extension are considered stable [3, 4].
The purpose of this study was to evaluate the functional and radiological outcome of proximal femoral nail antirotation II in the treatment of unstable intertrochanteric fractures in Indian patients.
MATERIALS AND METHODS
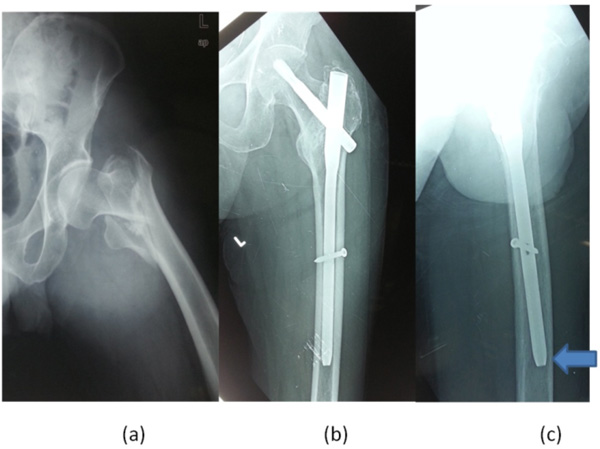
From January 2011 to March 2013, 45 unstable intertrochanteric fractures treated with the PFNA II (Synthes, Solothurn, Switzerland), were followed retrospectively. Three patients were died within 6 months of follow up. There were 26 men and 16 women with mean age of 61 years (range, 35 - 90). Right hip was involved in 30 patients and left in 12 patients. In 25 patients fractures were caused by trivial fall and the rest were caused by road traffic accidents or fall from height. AO classification was used to classify these fractures [3]. 18 fractures were classified as 31.A2 and 24 fractures as 31.A3 based on pre-operative radiograph. All surgeries were carried out at our tertiary care level 1 trauma centre within a mean of six days (range 2-12 days) from date of injury. All surgeries were done over fracture table in supine position. Closed reduction of the fracture under fluoroscopic guidance was possible in 25 cases. Rest were reduced with minimal opening of the fracture site using various reduction manoeuvres like strategically placed hohmann retractors (Fig. 1) and reduction clamps. Mean operative time (skin to skin) was 32 minutes (range 18 - 90 minutes). All patients received prophylactic antibiotic (cefazolin) within 1 hour of skin incision. The sizes of PFNA II nail used are depicted in Table 1. Commonly used nail diameter was 10 mm, which was used in 33 patients. In remaining patients, 9 mm nail was used. Most commonly used nail size was the smaller version (200 mm length) and commonly used blades were between 90-105 mm. Cleveland zones [5] and tip apex distance (TAD) [6] was used to evaluate the placement of helical blade in the femoral head. The fracture reduction was evaluatedon the first post-operative radiograph using the Garden Alignment Index (GAI) [7] and fracture gap (mm) measurement. The results were classified using GAI as very good (anteroposterior 160°); good (anteroposterior 180°-160°); acceptable (anteroposterior 160°-150°); or poor (anteroposterior < 150°/lateral not 180°[8]. The fracture gap was classified as good (0-3 mm); acceptable (3-5 mm); or poor (> 5 mm) (Fig. 2). The active range of motion exercises and partial weight bearing mobilisation was started on the firstpost-operative day as tolerated. The proximal end of nail was protruded from the tip of greater trochanter in 4 patients (Fig. 3). The placement of helical blade was notable to be in central in both AP and lateral views in 30 patients. Intra operative fracture of greater trochanter was noted in 6 patients and there were no femoral shaft fractures. The mean hospital stay was 6 days (range, 3 - 15). Suture removal was done on 14th post-operative day.
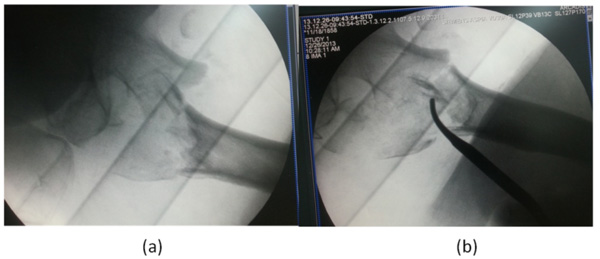
(a, b) Intra operative images showing fracture reduction using strategically placed hohmann retractors.

70 year old female patient, who sustained intertrochanteric fracture (31.A2) after a trivial fall (a). Post-operative radiographs showing good fracture reduction (b, c).

Mismatch between proximal end of nail and greater trochanter (solid arrow) noted even after placing blade in the inferior position (a, b).
65 year old male patient, who sustained unstable intertrochanteric fracture (a), 9 months follow up radiographs (b, c) shows fracture union with nail tip impinging on anterior femoral cortex (solid arrow) causing persistent thigh pain.
Nail sizes used in our series.
| Nail Size | Number (n) | Percentage (%) |
|---|---|---|
| Small (200 mm) | 22 | 52.38 |
| Standard (240 mm) | 5 | 11.9 |
| Very small (170 mm) | 4 | 9.5 |
| Long | 11 | 26.19 |
Assessment of fracture gap and GAI.
| Number (n) | Percentage (%) | ||
|---|---|---|---|
| Fracture gap | Good (0-3 mm) | 34 | 80.9 |
| Acceptable (3-5 mm) | 6 | 14.2 | |
| Poor (>5 mm) | 2 | 4.7 | |
| GAI | Very good | 10 | 23.8 |
| good | 22 | 52.3 | |
| acceptable | 8 | 19 | |
| poor | 2 | 4.7 | |
Intra- and post-operative frequencies of complications.
| Complications | Number (n) |
Percentage (%) |
|
|---|---|---|---|
| Intra-operative | Fracture of greater trochanter | 6 | 14.2 |
| Femoral shaft fracture | 0 | 0 | |
| Post-operative | Nail mismatch at the proximal end | 4 | 9.5 |
| Anterior thigh pain | 3 | 7.1 | |
| Fascia lata pain | 2 | 4.7 | |
| Secondary varus development | 2 | 4.7 | |
| Persistent limp | 6 | 14.2 | |
| Heterotopic ossification | 1 | 2.3 | |
Functional assessment using Harris hip score.
| Harris Hip Score | Number (n) | Percentage (%) |
|---|---|---|
| Excellent | 15 | 35.7 |
| Good | 18 | 42.8 |
| Fair | 6 | 14.2 |
| Poor | 3 | 7.1 |
The mean follow up period was 15.3 months (range, 9 - 27). All patients were evaluated clinicallyusing Harris hip score [8] and radiologicallyat 6 weeks, 12 weeks, 6 months, 9 months and thereafter every 6 months. Mean time for full weight bearing was 6 weeks. Anteroposterior and lateral plain radiographs were obtained at each visit to look for the fracture union, tip apex distance, cut-out or lateral migration of helical blade.
RESULTS
At the final follow up, all fractures were united. Three patients were died within first 6 months of follow up and hence, not included in the study. 80% of cases showed fracture gap of less than 3 mm and Garden Alignment Index (GAI) was graded as very good to good in 76% of cases (Table 2). In 71% of cases, tip of the helical blade was within Cleveland zone 5. TAD was less than 25 mm in 66% of cases. Two patients had persistent distraction at the fracture site while passing the nail intra-operatively.
Intra and post-operative complications are depicted in Table 3. There were no cases of infection, cut out or breakage of the implant. No femoral shaft fractures were noted in the follow up period. Two cases of fascia lata pain were noted due to laterally protruding helical blades. Implant removal was done in two patients due to persistent anterior thigh pain (Fig. 4). The mean Caput-collum-diaphyseal angle was 135.5° (range, 126° - 145°). Secondary varus was detected in two patients (4.7%) on final follow up radiographs.
Clinical evaluation was done using Harris hip score (Table 4). Excellent and good results were accounted for 78% of cases.
At the latest follow up, 32 patients (76.1%) were able to walk independently, 8 (19%) needed walker or crutches and 2 patients (4.7%) were unable to walk. Walking ability to pre-operative levels was restored in 36 (85.7%) patients. Out of 2 patients who were not ambulatory, one had severe Parkinson’s disease and the other had heterotopic ossification.
DISCUSSION
The incidence of unstable intertrochanteric fractures is increasing and this trend is likely to continue. These fractures are challenging for an average orthopaedic surgeon. Treatment modalities include osteosynthesis with dynamic hip screws and cephalomedullarynails and in selected cases, arthroplasty. However, the choice of implant for unstable intertrochanteric fractures is still debatable. PFNA II are now favoured in west and there are multiple studies coming from that region to support this [9-11]. Very few studies exist on this subject from Indian population. In our study of unstable intertrochanteric fractures treated by PFNA II, we found good outcome with very few complication rate and high union rate with short operative time and early post-operative mobilization. Our complication rate is comparable to previous studies [12].
The change to helical blade was aimed to decrease the risk of cut out. However, the cut out of helical bladestill remains to be the common cause of failure. There were no cases of cut outs in our study. The various studies have reported wide range of cut out rates varying from 2 - 25% [13-16]. The design of helical blade was quoted as a possible reason for cut out and medial perforation of subchondral bone [13].
Baumgaertner et al. [6] documented that the optimal placement of the lag screw was in the centre/centre position. The correct placement of the lag screw and helical blade at the centre of the femoral head and neck is important in both the antero-posterior and axial views. TAD is one of the most important predictive factors for the occurrence of a cut out [17, 18]. Geller et al. reported 44% of cut outs in intertrochanteric fractures fixation with TAD of > 25 mm and did not cut out with TAD of < 25 mm [19]. We did not observe blade cut outs in our series; even 14 patients were fixed with TAD > 25 mm. We agree with Jin et al. and preferredusing a blade that is shorter than usually recommended to prevent inadvertent femoral head perforation due to collapse at fracture site [20]. Nikoloski et al. hypothesized that the helical blade behaved in different way to a screw in the femoral head and recommended the TAD to be kept between 20-30 mm [21].
Jin et al. [20] preferred long over the shorter PFNA nail when there is excessive anteriorcurvature of the femur. In our study, we noticed impingement of tip of nail (240 mm length) to the anterior cortex in four cases due to excessive bowing and short femur length in Indians. There is mismatch between design of shorter nails and anatomy of femoral canal in Chinese population [12]. It is better to use longer nail to bypass the curvature or relatively shorter nail to prevent this complication especially in patients with excessive anterior bowing of femur.
No cases of intra operative femoral shaft fractures were noted in our study. Yaozeng et al. reported 6 (5.6%) intra operative femoral shaft fractures in their series of 107 intertrochanteric fractures [22]. Adequate reaming of the femoral canal especially when using longer nails can decrease the incidence of this complication.
Boopalan et al. [23] reported 21% incidence of intra operative lateral wall fractures in 31 A1 and A2 pertrochanteric fracture fixation. The fracture union was not affected by the presence of lateral wall fractures in their study. Gotfried [24] reported 24 cases of lateral wall fractures in their study. On radiographic examinations, he observed varusmalalignment with medialisation of femoral shaft in all these cases. This was attributed to the use of a lateral cortex drill of 16 mm diameter for sliding screw [24]. We noted 6 cases of intra operative lateral wall fractures, out of which 2 cases developed secondary varus collapse of 5 degrees. None of these fractures required reoperation.
We noted two cases of intra operative fracture distraction during our earlier days. This occurs most commonly when the broad proximal portion of the nail passes through the intertrochanteric area. The proximal fracture fragment translates along the intertrochanteric line and distal part of the nail pushes the femur laterally giving rise to distraction. This can be associated with varusmal alignment. Varus deformity and distraction also occurs when the guide wire is inserted directly through the fracture site [25]. They advised to use entry reamer after over-distracting the fracture. This will ream the lateral edge of medial fragment, which is the main reason for varus and distraction. We have found the method described by Janardhana Aithala P et al. [26] useful. They have advised to ream the proximal fragment adequately as this assists in easy passage of the nail and also asks the assistant to apply and maintain some pressure over trochanter while passing proximal portion of the nail. Use of long artery forceps or a hohmann retractor in the lesser trochanteric area under the neck of femur to push it up during nail passage also prevents distraction.
In the last 3 years, several studies [27-29] have reported successful outcome with low complication rates with PFNA in unstable per trochanteric fractures. Our study supports this finding, suggesting that PFNA is a reasonable option in unstable trochanteric fractures.
Our study is attributed to all the limitations of retrospective design with relying on operative notes for intra operative details. Our sample size was small with wide variability in the age. Prospective studies comparing different implants in the fixation of unstable intertrochanteric fractures with matched variables are needed.
CONCLUSION
In conclusion, we recommend PFNA II for fixation of unstable intertrochanteric fractures with less operative time and low complication rate. However, proper operative technique is important for achieving fracture stability and to avoid major complications.


