All published articles of this journal are available on ScienceDirect.
Management of the Floating Knee in Polytrauma Patients
Abstract
Ipsilateral fracture of the femur and tibia, or floating knee, is a rare injury that is found almost exclusively in polytrauma or high-energy trauma patients. It presents a combination of diaphyseal, metaphyseal and intra-articular fractures of the femur and tibia, with a high incidence of neurovascular, ligamentous and soft-tissue injuries. The functional outcome and, in some cases, the life, of such polytrauma patients depends largely on a correct therapeutic approach being taken. In general, the treatment decided upon will depend on the individual characteristics present, regarding aspects such as the patient’s general condition, the fracture line and the state of the soft tissues. The treatment provided may be the same as when single fractures are presented, but it is often necessary to consider whether certain techniques or surgical approaches may interfere with other lines of treatment. It is essential at all times to take into consideration the associated injuries and complications before deciding upon a treatment strategy. Ligamentous injuries play an important role in these injuries, much more so than when fractures occur singly. Therefore, these injuries require management by an experienced multidisciplinary team.
INTRODUCTION
Floating knee is a term used to refer to fractures affecting the ipsilateral tibia and femur. These fractures can affect the diaphysis, the metaphysis and even the articular complex, such that the knee becomes "disconnected" from the rest of the limb. Although its exact incidence is unknown, this condition is generally rare, although it is been increasing in recent years in the same proportion as the number of polytrauma patients affected by high-energy trauma. Being almost always caused by such trauma, floating knee is commonly suffered by patients who also present with severe injuries to the chest, head, abdomen and/or limbs [2]. Characteristically, floating knee presents associated injuries that can sometimes be life threatening. It is almost always associated with soft-tissue injuries, including ligament injuries. Vascular injuries are more commonly associated with this type of injury when the fractures present singly, which in some reported studies occurs in up to 29% of cases [3] although other authors believe these complications are less frequent [4, 5]. Some reports have described the presence of open floating knee in 60-80% of cases [6]. It is also associated with neurological injuries and fat embolism.
In this chapter we present the general characteristics of floating knee and the treatment approach that is most commonly recommended.
CLASSIFICATION
Various classifications of floating knee have been proposed. The one that is most commonly employed is that of Fraser et al. [5], who distinguished two types of injury; one with diaphyseal fractures in both bones, and the other with articular fractures, in one or both bones (Fig. 1).
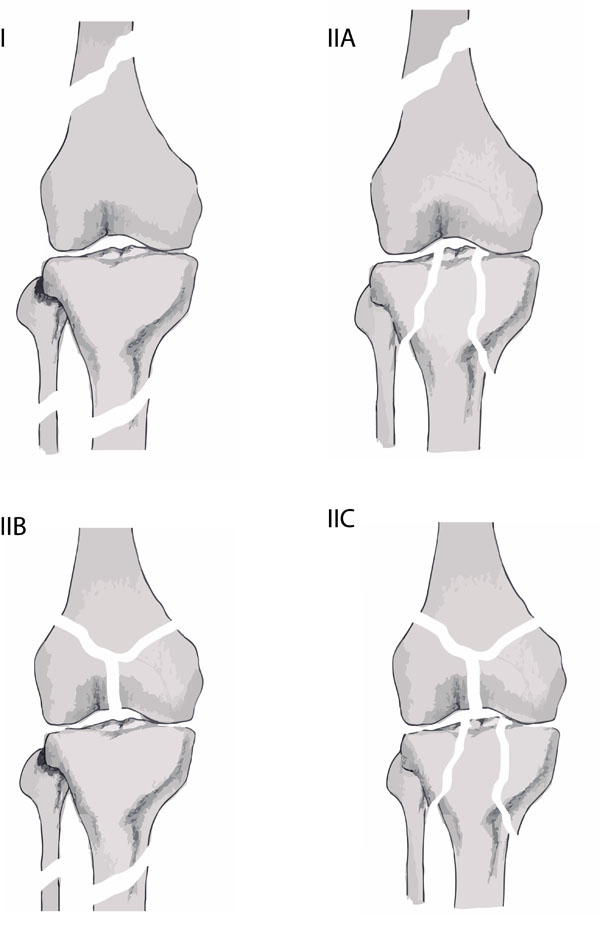
Fraser’s classification of floating knee.
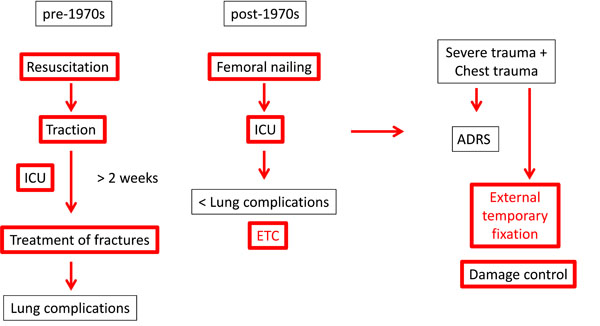
Historical evolution of management of femoral fractures in polytrauma patients.

(a) Fraser type IIb floating knee. (b) Damage control by external fixation in each segment.

(a, b, c) Fraser type I floating knee. (d, e, f) Nailing in the two segments: final result.
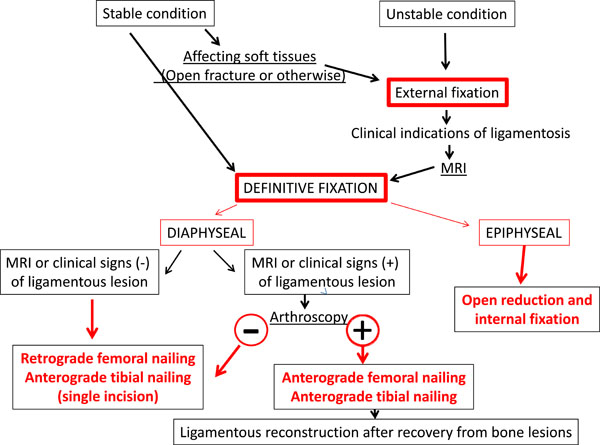
Algorithm for treatment of floating knee.
Mangled extremity severity score (MESS) [21].
| Mangled Extremity Severity Score (MESS) | |||
|---|---|---|---|
| Type | Characteristics | Injury | Points |
| 1 | Low Energy | Stab wound, simple closed fracture, small-calibre GSW | 1 |
| 2 | Medium Energy | Open/multilevel fracture, dislocation, moderate crush | 2 |
| 3 | High Energy | Shotgun, high-velocity GSW | 3 |
| 4 | Massive Crush | Logging, railroad, oil-rig accidents. | 4 |
| Shock Group | |||
| 1 | Normotensive transiently | BP stable | 0 |
| 2 | Hypotensive prolonged | BP unstable in field but responsive to fluid | 1 |
| 3 | Hypotension | SBP <90mm Hg in field and responsive to IV fluids in OR | 2 |
| Ischaemia Group | |||
| 1 | None | Pulsatile, no signs of ischaemia | 1 |
| 2 | Mild | Disminished pulse without signs of ischaemia | 2 |
| 3 | Moderate | No dopplerable pulse, sluggish cap refill, paresthaesia, diminished motor activity. | 3 |
| 4 | Advanced | Pulseless, cool, paralysed, numb, without cap refill | 4 |
| Age Group | |||
| 1 | < 30 years | 0 | |
| 2 | 30-50 years | 1 | |
| MESS Score: | |||
| Six or fewer points: consistent with a salvageable limb | |||
| Seven or greater: amputation generally the eventual result | |||
GSW: gun shot wound, BP: blood pressure. SBP: Systolic blood pressure. IV: intravenous. OR: Operation room.
Ran et al. recently proposed a modification of this classification, to take into consideration, in addition, the impact on the patella and the complexity of the articular fracture [7]. The purpose of these classifications, in principle, is to contribute to establishing a prognosis, because a priori diaphyseal fractures present fewer complications and functional recovery is better than those affecting the joint. However, Ran’s classification does not take into account diaphyseal fractures associated with a fractured patella, and neither of these classifications considers associated soft-tissue injury or ligament injuries. Nevertheless, these questions should be addressed because they may influence treatment planning and can provoke multiple post-surgery complications [8].
TREATMENT
Ipsilateral femoral and tibial fractures are almost always produced by high-energy trauma. In addition, these injuries are often associated with other life-threatening conditions, as well as other fractures and varying degrees of soft-tissue lesion. In consequence, patients are usually haemodynamically unstable and require close monitoring and resuscitation during the initial post-injury period. Meticulous attention to life-threatening injuries is necessary, identifying those that might jeopardise the ABCDE’s. Therefore, advanced trauma life support protocols should be followed rigorously and the patient stabilised before orthopaedic treatment can be considered [9].
Damage Control Orthopaedics
The management of fractures, especially of the femur and pelvis in polytrauma patients, has always been a controversial issue. In view of the high mortality presented by these patients when their immobilisation is delayed, treatment approaches have changed, from the concept of Early Total Care (ETC) – which was associated with a significant rate of complications in unstable patients – to the currently prevailing concept of Damage Control Orthopaedics (DCO), i.e. immobilising the fracture by means of external fixation (Fig. 2) [10]. DCO focuses on the procedures that must be performed immediately in order to save the patient’s life; only subsequently, after admission to the intensive care unit, is the question of definitive treatment addressed. This concept, therefore, calls for minimally invasive surgery for the primary stabilisation of major fractures, especially the long bones. This approach helps control bleeding and minimises the "second hit" phenomenon [11]. Therefore, DCO involves not only stabilising the limbs but also conducting emergency management of associated injuries such as compartment syndrome or vascular lesions.
Which patients will benefit from the application of DCO and which from ETC is a question that has yet to be clarified. In stable patients, it seems clear that ETC is more appropriate, while haemodynamically unstable patients equally clearly require DCO. However, considerable doubt remains with respect to borderline patients; some authors recommend caution with ETC and use serum bicarbonate levels as an indicator of hypoperfusion to determine when DCO should be performed [12]. Others argue the benefits of ETC in most cases, except the most critical ones, in the belief that this early treatment of fractures can reduce hospital stay, facilitate recovery, prevent articular stiffness and enable early mobilisation, which indirectly decreases the risk of deep vein thrombosis and promotes healing [13, 14]. Other authors, such as Pape et al., advise sequential treatment, delaying the definitive fixation until the patient’s recovery is well advanced [15]. In summary, in most cases treatment should be individualised after carefully assessing the benefits of rapid, definitive skeletal stabilisation versus potential life-threatening risks of systemic complications such as fat embolism, acute lung injury or multiple organ failure [16].
Orthopaedic surgeons still differ on the question of the optimum timing for surgery to be performed for injuries to the extremities. There is also controversy as to which fractures present a true emergency and in which cases it is better to delay definitive treatment in order to minimise physiological trauma to the patient. Various studies have considered the question of the most appropriate sequence to be adopted in treating patients with multisystem injuries, but only recently has a detailed study been made of the role of complex musculoskeletal injuries and of the optimum time for fixation in patients with multiple lesions [17]. However, existing data are often difficult to compare, given the diversity of definitions and protocols proposed. Furthermore, the information reported is often contradictory, which makes it very difficult to determine an optimum time window. Similar problems arise with long bone fractures of the lower extremities.
It is essential to consider the lesions affecting other organs in order to synchronise their treatment with the fixation of floating knee fractures. This is especially so in the presence of lung injury, as polytrauma patients with associated chest trauma present a significantly higher incidence of posttraumatic organ dysfunction than is the case of trauma patients with the same severity of injury but no chest trauma. The latter trauma, thus, appears to be a precursor to other complications, such as multiple organ failure [17].
In the early phase of care for polytrauma patients with fractures of the pelvis and/or long bones, it is particularly important to determine the extent of the injury associated with the soft tissues and the presence of vascular injury and compartment syndrome, as these lesions require immediate, urgent treatment and their outcome will directly depend on the delay or otherwise in this respect [18].
The traditional approach in evaluating polytrauma patients is to consider their haemodynamic stability. The "triad of death" is a term coined to describe the decompensation caused by acute blood loss, resulting in hypothermia, coagulopathy and acidosis. The prevention or reversal of these factors may prevent death from exsanguination. More recent studies have highlighted the influence of orthopaedic injuries on this triad [17].
The correct time to treat a fracture depends on appropriate resuscitation having been conducted. Markers of the appropriate response to resuscitation are provided by easily-accessible data, namely serum lactate levels below 2.5 mmol/L and base deficit of less than 8 mEq/L. Other markers that are frequently used include diuresis, pulse rate and blood pressure. Ideally, all these parameters should be normalised prior to undertaking the fixation of fractures. It is of particular importance to reverse any coagulopathy and to correct the core body temperature. Gentilello et al. observed a mortality rate of 100% if the core body temperature is not restored during the first phase of care [19]. In accordance with the ability to restore these parameters, patients are divided into four categories during the resuscitation phase: stable, borderline, unstable, and in extremis.
When considering the surgical treatment to be applied to orthopaedic injuries, a number of priorities must be taken into account. The first of these is to save the patient's life and, where feasible, the extremity, and to limit the time spent in the operating room to less than two hours [17]. Within this surgical window, open fractures should be debrided and stabilised with an external fixator. A splint may be sufficient for upper extremity lesions. Negative pressure therapy plays a crucial role in the treatment of orthopaedic injuries. An initial amputation can save the life of a patient in extremis due to the fracture of an extremity or an open fracture with vascular injury. Specific criteria cannot be indicated for every situation, as diverse variables must be considered in every case.
The use of external fixation as an initial approach avoids the need for more time-consuming procedures that can worsen the "triad of death". In this respect, procedures lasting more than six hours are particularly dangerous, as they are associated with higher rates of acute respiratory distress syndrome and multiple organ failure. Some factors, directly relevant to the work of orthopaedic surgeons, are associated with adverse outcomes; these include multiple long bone fractures, pelvic trauma in the presence of haemorrhagic shock, surgical time exceeding six hours, and pulmonary artery pressures above 6 mm/Hg during intramedullary nailing, which is indicative of significant lung damage [20].
After examining indicators of adverse outcomes, we identify four physiological factors that result in decompensation in patients with multiple lesions. In addition to the "triad of death" described above, soft-tissue injuries constitute a fourth, and equally important, factor affecting polytrauma patients [15].
The need for a thorough secondary survey should not be underestimated. In cases of floating knee, the extremity is usually very swollen and deformed, and this can represent an important "distracting factor" and it is not uncommon for other significant injuries go unnoticed.
As mentioned above, associated injuries (head, chest or vascular injuries and other fractures) play a significant role in surgical decision-making regarding the timing and sequence of surgery.
It is essential to diagnose the lesions associated with floating knee because they may be life threatening. Therefore, the impact on the extremity systems (soft tissue, nerves, vasculature and bone) must be determined. When they are severely affected, the surgeon must decide between initial amputation or salvage. The MESS (Mangled Extremity Severity Score) scale takes into account: (1) skeletal and soft-tissue injury; (2) limb ischaemia; (3) shock; (4) the patient's age [21]. This tool has proven to be useful in the clinical and legal management of such lesions (Table 1).
Many other assessment protocols have been proposed, but none has been definitively accepted in decision making regarding limb salvage versus amputation in the management of patients with severe limb trauma. Therefore, further research is needed to determine more precisely the factors that can help decision making, and to reduce the frequency of fruitless salvage attempts. Medical and surgical advances in recent years have enhanced the ability to reconstruct severely injured limbs, such that limbs which years ago would have been amputated are now routinely managed and salvaged. Nevertheless, most studies carried out to evaluate such reconstruction techniques have been small scale and retrospective, and so the results obtained are not definitive.
Although conflicting results have been reported, some researchers suggest that the functional outcome is often worse after successful reconstruction of the limb than after early amputation and appropriate fitting of a prosthesis [22-24]. In this respect, Bosse et al. carried out a prospective observational study comparing the functional results of a large cohort of Level I trauma patients from eight hospitals who underwent reconstruction or amputation. These authors found that patients who underwent amputation presented functional outcomes similar to those of patients who had undergone reconstruction. Furthermore, the resulting levels of disability at two years were high in both groups. It was also found that the factors associated with a worse outcome, irrespective of the type of injury or treatment, included low levels of education, nonwhite race, low purchasing power, lack of private health insurance, smoking, and involvement in litigation for disability compensation. These findings suggest that further effort is needed to take into account non-clinical aspects of this type of patient as a means of achieving good psychosocial rehabilitation [25].
Damage control treatment for floating knee involves not only bone stabilisation using an external fixator and the treatment of open fractures by wound cleansing and debridement (in addition, in some cases, negative pressure therapy [26, 27] or antibiotic beads can be useful) [28, 29] but also, and fundamentally, the treatment of associated lesions such as vascular injury or compartment syndrome, in which the corresponding fasciotomy must be performed.
In type I floating knees with both tibial and femoral diaphyseal fractures, an independent fixator can be placed in each segment; with the patient under anaesthesia, at this point it is important to explore the stability of the knee because in some cases it may be necessary to protect it, either by a bridge with the fixator itself or by means of a locking brace. In type II floating knees, with articular fractures, an external fixator must be used to bridge the knee, and in these cases it is important to carefully plan the definitive surgery so that the nails of the fixator do not obstruct future routes of approach or the sites for implants (Fig. 3). If the patient is treated by damage control with an external fixator, we recommend using a latest-generation fixator that allows magnetic resonance imaging to be performed [30].
Definitive Treatment
The stage at which the definitive fixation of the fracture should be performed, after a temporary one with external fixation, is a controversial subject, but in general this will depend on the patient’s general condition and on the observed recovery of the soft tissues.
Although several authors have reported good to excellent results with the treatment of these lesions [4, 31], in our experience, the severity of the trauma necessary to produce a floating knee, together with the low incidence of this injury and the presence of other fractures or injuries, is largely responsible for the poor functional results and high rates of complication often seen after this injury.
It seems clear that in type I floating knees, with diaphyseal fractures, the gold standard treatment is that of intramedullary nailing (Fig. 4). On the other hand, type II floating knees, with intra-articular fractures, should ideally be stabilised after a delay of a few days until the surrounding soft tissues are in good condition; then, for the definitive surgery, open reduction techniques are usually necessary for anatomic reconstruction of the joint, while metaphyseal-diaphyseal reduction can be performed indirectly.
Traditionally, ipsilateral femoral and tibial fractures were treated by nailing only the femur and securing the orthopaedic immobilisation of the tibia. However, this approach provoked many complications, including fat embolism [32]. Akinyoola et al. reported the presence of significantly more complications in patients whose treatment was delayed and in those who were not treated surgically [33].
The definitive treatment that is most widely accepted today is that of surgical stabilisation of both bones, individualised for each patient and fracture [1]. The direction and location of each fracture, the soft tissue status, the resources available and the surgical skill employed all play an important role in determining the most appropriate treatment.
Standard practice is for anterograde femoral nailing to be performed first, followed by anterograde tibial nailing. However, many authors believe this technique produces difficulties in positioning the patient; it also requires two surgical approaches and considerable operating time. For these reasons, an alternative method has been considered, in which the two bones are interlocked using a single medial parapatellar approach, through which a retrograde femoral nail and a tibial anterograde nail are inserted [34]. Rios et al. studied 43 patients with floating knee injuries, a treatment group of 25 patients, treated with retrograde femoral nailing and anterograde nailing of the tibia through a single incision, and a control group of 18 patients treated with traditional intramedullary anterograde femoral and tibial nailing. According to the results reported, the femoral retrograde approach requires less preparation, anaesthesia and surgery time than the traditional anterograde femoral method; moreover, it produces less blood loss. These authors conclude that the single incision technique is a safe and rapid procedure that constitutes a valid alternative treatment for type I floating knee [35]. However, the placing of a retrograde femoral nail can be an obstacle to a later repair of the anterior cruciate ligament, an injury that very often accompanies this type of fracture.
Femoral nailing is performed first, while the tibia is temporarily stabilised with a splint or, in cases of severe comminution, with an external fixator. If the tibia were stabilised first, the movement and deformation of the femur during surgery would cause greater damage to the soft tissues and pose an increased risk to the patient’s general condition, including the increased incidence of fat embolism [1, 36]. Although it is generally agreed that the best treatment for diaphyseal fractures is that of nailing, there is no consensus as to the precise technique, and in some studies conducted in the 1990s a femoral distractor was used to maintain the reduction during the nailing (this technique has also been used in the tibia) [37, 38]. On the other hand, some authors recommend manual traction [39]. Nor is there clear agreement on the most suitable type of operating table for carrying out the nailing [39, 40].
In type II floating knee, affecting the joint, it is crucially important to perform anatomic reduction of the articular surface. As discussed above, metaphyseal-diaphyseal stabilisation can be performed indirectly, and minimally invasive fixation achieved by means of locking plates [41, 42].
Ligamentous instability of the knee following ipsilateral femoral and tibial fracture is a common occurrence, with an incidence of over 50%, and more so than in fractures of the femur or tibia alone forming the same pattern [43, 44]. Nevertheless, this condition is relatively frequently omitted from the initial diagnosis [45].
If temporary fixation is needed, it is recommended to use fixators that are compatible with MRI scanning, because after temporary stabilisation, MRI of the knee is recommended, if possible, if a ligament injury is suspected [46]. When the final fixation is performed, either by ETC or after sequential treatment, a clinical examination should be carried out of the ligamentous status of the knee, under anaesthesia. If a lesion is suspected, arthroscopy should be performed in order to obtain a precise diagnose of the injury, because after the definitive fixation MRI will not be possible due to interference by the implants. When injury to the anterior cruciate ligament is diagnosed, an antegrade femoral nail should be inserted, as a retrograde one may hinder subsequent ligamentoplasty. The repair of such ligament injuries can be delayed until the skeletal lesions have healed, although this is a subject of some debate among authors [43, 47]. In any case, it seems advisable for the ligament repair to be performed in a single step procedure [48].
Although there is no clear consensus as to the specific surgical indications, we propose an algorithm for the management of these lesions (Fig. 5).
The vascular lesion of fractures around the knee, primarily of the popliteal artery, is an injury that occurs in up to 29% of fractures, and the incidence of amputation can be as high as 21% [49]. In conducting a neurovascular examination of polytrauma patients, this should include an assessment of the peripheral pulses, from the ankle brachial pressure index, supported by Doppler ultrasound examination and the selective use of angiography. Although the initial physical examination may exclude vascular injury, it may occur during the first 24 hours due to the development of arterial thrombosis or the progression of incomplete injuries. Accordingly, vascular repair surgery should be urgently undertaken after the temporary fixation of unstable fractures [50].
The following neurological injuries may occur in ipsilateral fractures of the femur and tibia: bruising, requiring only observation, as this usually remits spontaneously in 3-9 months, or lacerations, in which case primary repair is recommended [50].
In general, the treatment of floating knees produces mixed results, and rates of complication are high. The most common are systemic, such as fat embolism, renal failure, or head, chest or abdominal lesions, and the sequelae of other trauma. Effects may also be local, directly related to the trauma of the extremity, including pain, ligamentous laxity, decreased articular mobility, limping, delayed union or nonunion, osteomyelitis and even the need to amputate the limb [6]. Type II floating knee seems to be associated with a greater degree of systemic trauma, a higher percentage of open lesions and a much more serious prognosis [51].
Kao et al. found that floating knee injuries are usually associated with high rates of complications and mortality, regardless of the treatment regimen used. These complications are associated with age (more common in patients aged 60-89 years), the type of injury (greater in type II floating knee, according to the Fraser classification) and location (greater in tibial plateau, distal tibia and open fractures) [4].
CONCLUSION
Floating knee, with ipsilateral femoral and tibial fracture, is a serious injury, closely related to high-energy trauma and to many associated injuries, which are often very severe, and both systemic and local. In planning treatment, it is essential to take into account the patient’s overall condition and the local situation of the limb. In some cases, amputation is the best option.
In general, the treatment decided upon will depend on the individual characteristics present, regarding aspects such as the patient’s general condition, the fracture line and the state of the soft tissues. The treatment provided may be the same as when single fractures are presented, but it is often necessary to consider whether certain techniques or surgical approaches may interfere with other lines of treatment.
It is essential at all times to take into consideration the associated injuries and complications before deciding upon a treatment strategy. Ligamentous injuries play an important role in these injuries, much more so than when fractures occur singly. Therefore, these injuries require management by an experienced multidisciplinary team.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The authors thank Dr. Manuel Angel Valdés-Vilchez for his excellent technical assistance in the design and preparation of the manuscript figures.
We also thank the Research and Development Department of the Hospital Costa del Sol for their language review of this manuscript.


