All published articles of this journal are available on ScienceDirect.
Autograft Transfer from the Ipsilateral Femoral Condyle in Depressed Tibial Plateau Fractures
Abstract
Introduction :
The rationale for operative treatment of depressed tibial plateau fractures is anatomic reduction, stable fixation and grafting. Grafting options include autogenous bone graft or bone substitutes.
Methods :
The autograft group included 18 patients with depressed tibial plateau fractures treated with autogenous bone grafting from the ipsilateral femoral condyle following open reduction and internal fixation. According to Schatzker classification, there were 9 type II, 4 type III, 2 type IV and 3 type V lesions. The average time to union and the hospital charges were compared with the bone substitute group. The latter included 17 patients who had an excellent outcome following treatment of split and/or depressed lateral plateau fractures, using a similar surgical technique but grafting with bone substitutes (allografts).
Results :
Excellent clinical and radiological results were detected in the autograft group after an average follow-up of 28 months (range 12-37). The average time to union in the autograft group was 14 weeks (range 12-16), while in the bone substitute group it was 18 weeks (range 16-20). The mean total cost was 1276 Euros for the autograft group and 2978 Euros for the bone substitute group.
Discussion :
The use of autogenous graft from the ipsilateral femoral condyle following open reduction and internal fixation of depressed tibial plateau fractures provided enough bone to maintain the height of the tibial plateau and was not associated with any donor site morbidity. Using this method, the surgical time was not significantly elongated and the rehabilitation was not affected. It also exhibited faster fracture healing without postoperative loss of reduction and it was less expensive than the use of bone substitutes.
INTRODUCTION
The early restoration of normal joint function is the goal of treatment of depressed fractures of the tibial plateau. The principles of treatment include arthroscopically assisted or open anatomic reduction followed by stable internal fixation [1-5]. The reduction and internal fixation may be performed through open, limited open or percutaneous incision approaches [6-8]. Arthroscopic reduction may be used in only in the low-energy Schatzker types I to IV, while more complex or higher-energy injury patterns may require open reduction [9]. Indirect reduction associated with external or hybrid fixation may be used in high-energy fracture types with a severe concomitant injury to the soft tissue envelope [10, 11]. Bone grafting using autografts or bone substitutes is concomitantly used to support the reduction and promote fracture healing. Recommendations of bone grafting materials are based on their mechanical and handling characteristics, safety, and cost [12].
The objective of this study was to evaluate the results of bone grafting with autogenous bone derived from the ipsilateral femoral condyle to stabilize the height of thedepressed tibial plateau fracture following open reduction and internal fixation. The advantages and the clinical outcome of the procedure in 18 patients are presented and discussed. In addition, the average time to fracture union and the mean total cost of autograft versus bone substitute reconstruction were estimated.
MATERIALS AND METHODS
The medical records of 18 patients (18 fractures) that had autogenous bone grafting taken from the ipsilateral femoral condyle in depressed tibial plateau fractures, following open reduction and internal fixation, were retrospectively reviewed. They were all included in the autograft group, consisting of 12 men and 6 women aged from 16 to 57 years (average 47.6 years) treated during January 2009 and December 2012. Mechanism of injury included motor vehicle crashes, motor-pedestrian accidents and low-energy falls. There were no polytrauma patients, open injuries and injuries with neurological compromise, vascular deficit or an acute compartment syndrome. Conventional radiographs were used to assess the degree of joint depression preoperatively and the reduction postoperatively, as well as on final reviews. Computed tomography scan was performed in all patients preoperatively for accurate fracture evaluation and classification and, in 3 patients, early postoperatively. According to the Schatzker et al. [1] classification system, 9 fractures were classified as type-II, 4 as type III, 2 as type IV and 3 as type V (Fig. 1a). Mean operating time was 85 minutes. Inpatient hospitalization ranged from 5-8 days (mean 6 days).
Times for autograft incorporation and fracture healing were estimated. The cost billing sheets for the autograft group were extracted from the Hospital computer database. The total cost included cost of inpatient hospitalization and cost of implants.
The average time to fracture union and the cost analysis were compared with the bone substitute group.
The bone substitute group included 17 split and/or depressed lateral tibial plateau fractures treated with open reduction, one-sided internal fixation and grafting with bone substitutes. They were all enrolled from 2003 to 2008. Their mean age was 51.3 years (range 37-58 years). Classification according to Schatzker et al. included 12 type II and 5 type III fractures. Bone grafting using virus inactivated human bone allograft was used in 4 fractures and cadaveric human bone allograft in 13 cases. Mean operating time was 80 minutes. Inpatient hospitalization ranged from 5-8 days (mean 6 days).
The surgical technique in both groups included open reduction and complete bone grafting of the defect followed by internal fixation. Menisci and anterior cruciate ligament were intact in both groups of patients, while no perioperative or postoperative complications were recorded. Union was defined as continuity of both cortices in two radiographic planes. Patient characteristics, outcomes and cost comparison are summarized in Table 1.
Comparison between the two groups.
| Parameters | Number of Patients | Gender | Age (Years) | Schatzker Classification | Donor Site | Mean Operating Time (Min) | Hospitalization (Days) | Fracture Union (Weeks) | Follow- Up (Months) | Total Cost (Euros) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | II | III | IV | V | |||||||||
| Autograft group | 18 | 12 | 6 | 16-57 (mean: 47.6) | 9 | 4 | 2 | 3 | LFC:16 MFC:2 | 85 | 5-8 (mean:6) | 12-16 (mean:14) | 12-37 (mean:28) | 1123-1401 (mean:1276) |
| Bone substitute group | 17 | 11 | 6 | 37-58 (mean: 51.3) | 12 | 5 | Allo- grafts | 80 | 5-8 (mean:6) | 16-20 (mean:18) | 22-48 (mean:32) | 2656-3583 (mean:2978) | ||
M: Male.
F: Female.
LFC: Lateral femoral condyle.
MFC: Medial femoral condyle.
In addition, five elderly osteoporotic patients receiving no drug therapy were also treated with the same operative technique using bone grafts from the ipsilateral femoral condyle, but were not included in the study. All surgeries were performed by the author.
OPERATIVE TECHNIQUE
Patients were placed supine on the radiolucent operating table. Tourniquet was used for all the surgeries. An anterolateral or medial parapatellar incision was used for unicondylar fractures, whereas a midline single-incision approach was used for open reduction and internal fixation of bicondylar fractures. The depressed articular surface was visualized through a submeniscal exposure and the impaction was reduced from below through the anterior portion of the split condyle or using a metaphyseal window (approximately 1x1.5cm) made in the subcondylar region of the respective tibial condyle. Autograft was harvested from the ipsilateral femoral condyle. The synovium and perios-teum were split longitudinally and elevated over the ipsi-lateral femoral condyle. A cortical window (approximately 1x2cm) was created in the femoral condyle. The donor site level was located on the lateral or medial cortex above the physeal scar. At this point the cortical metaphyseal bone is softer and thinner (Fig. 1b). Two techniques were used to remove the cortical window. In the first technique multiple holes were drilled in the periphery using a 1.2mm drill and the cortical window was then removed using a small osteotome. In the second and more recent one, an oscillating saw with a fine blade was used to divide the cortical window which was then detached using a hook inserted from the periphery of the osteotomy. The depressed articular fragments were reduced from below using a bone punch and supported by the cortical femoral window and the metaphyseal tibial bone, when available, that were impacted parallel to the joint line. Malrotation was fixed intraarticularly with the use of a fine hook.
The residual defect was packed with cancellous bone autograft obtained from the ipsilateral femoral condyle until the articular fragments were slightly overreduced.
Autografts were harvested from the lateral femoral condyle in 16 and from the medial condyle in 2 patients.
One-sided internal fixation and stabilization followed using the standard nonlocking plate-fixation techniques in 17 cases, including cannulated screws, buttress or strong condylar plates, while a locking plate was used in one over weighted patient (Fig. 1). Locking plates were used in all the osteoporotic patients. Fluoroscopic control was used in all patients intraoperatively to aid and assess the reduction.
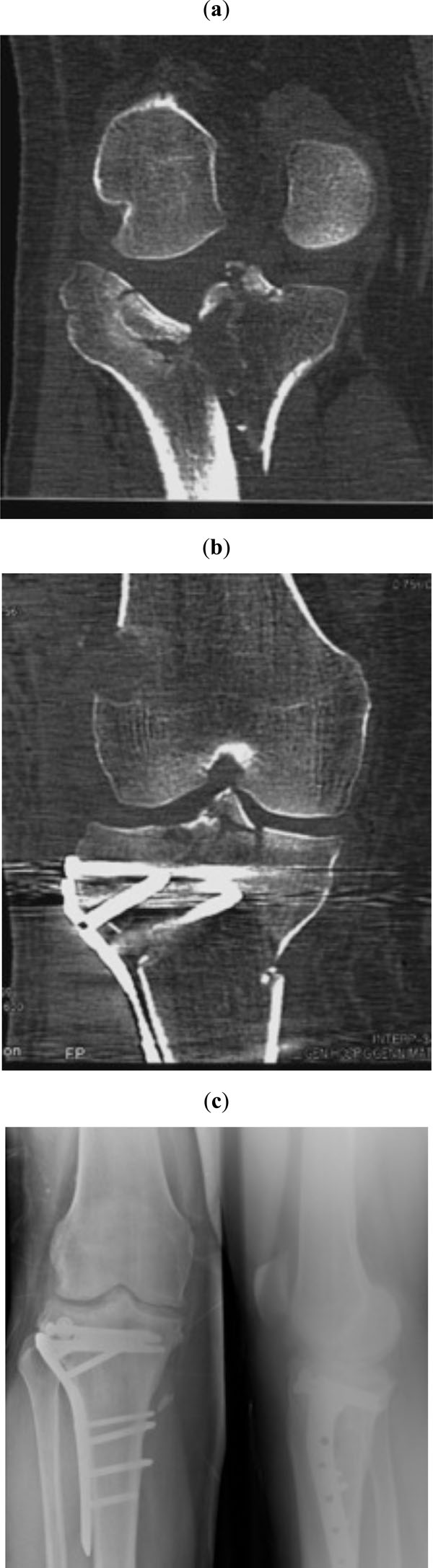
Schatzker type V fracture of the right tibia in a 36-year-old man with a body weight exceeding 160 kilograms that was not changed during follow-up. Preoperative (a) and early postoperative (b) computed tomography views. The femoral cortical window is located at the level of the physeal scar. Final radiographs, 30 months postoperatively (c).
Postoperatively, a compression dressing was applied around the knee for about a week, and gentle active and active-assisted flexion-extension exercises of the knee were started as early as the pain permitted. Full weight bearing was discouraged for at least 2 months.
RESULTS
Eighteen patients with a depressed tibial plateau fracture were included in the autograft group. The average time to fracture union in the autograft group was 14 weeks (range 12-16). Follow-up ranged from 12 to 37 months (average 28 months). The radiological results obtained at the final evaluation were compared to those obtained immediately after surgery. They indicated that the height of the reduced plateau was maintained to a less than 2mm depression level at follow-up in all cases (Fig. 1c). There were no infections or any other postoperative complications including morbidity at the bone graft donor site. The mean total cost for the autograft group was 1276 Euros (range 1123-1401 Euros).
Seventeen patients that exhibited an excellent clinical and radiological outcome following treatment with open reduction, internal fixation and grafting with bone substitutes (allografts) were included in the bone substitute group. The average time to fracture union was 18 weeks (range 16-20), while the mean total cost was 2978 Euros (range 2656-3583 Euros) for the bone substitute group.
The period of hospitalization was similar between the two groups. When the cost of the bone substitute was removed, the cost of plating implants was similar between the two groups. No patient in either group had loss of reduction, internal fixation or needed a reoperation. There was no significant difference in the range of motion in flexion and extension at six and twelve months in both groups.
The average time to fracture union in the 5 osteoporotic patients was 15 weeks (range 13-17). They all exhibited an excellent clinical and radiological result after a mean follow-up of 12 months. The mean total cost was similar with that of the patients in the autograft group.
Radiographic signs of external bone healing at the graft donor site were evident about 14 weeks postoperatively, but were 2-4 weeks earlier evident in the osteoporotic patients.
DISCUSSION
A wide variety of methods have been used to achieve anatomic reduction, stable fixation and early motion of depressed intra-articular fractures of the tibial plateau [13]. Open reduction and internal fixation of a non-complex closed fracture is the treatment of choice in most centers [14]. The single parapatellar and the midline incision are usually used for the unicondylar or bicondylar fractures of the tibial plateau, respectively [15-19]. Dual-incision approaches may be associated with a significantly higher rate of complications [10, 20-24]. Locking plates are indicated for high-energy or comminuted bicondylar fractures and in osteoporotic injuries [25-28]. Arthroscopic-assisted reduction and fixation is mainly indicated for pure depression fractures [9, 29, 30], while external fixation can be valuable in complex cases with gross intra-articular comminution and severe soft tissue compromise [31-33].
The use of bone grafting in conventionally treated plateau fractures is associated with superior results [34]. Bone graft, using either autogenous (autologous) bone or bone substitutes, is packed within the subarticular osseous defect following fracture reduction and preferably before internal fixation [5, 35, 36].
Autogenous bone graft has been considered the optimum standard for management of bone defects in unstable fractures of the tibial plateau. It exhibits all three prerequisite properties including osteogenic potential, osteoinductive factors and osteoconductive scaffold along with an optimal biological reaction. The most likely source of autograft for treating lateral tibial plateau fractures is the iliac crest [34, 37]. Other sources of autograft for treating depressed lateral tibial plateau fractures include the medial tibia, the fibula, the patella and the greater trochanter [30, 38-43]. The use of the distal femur has occasionally been referred as a bone graft donor site. Younger and Chapman [44] reported three out of 239 patients (243 autogenous bone graft donor sites) but the exact graft harvest site is not clear. The use of the lateral femoral condyle as an alternative graft donor site for lateral tibial plateau fractures has previously been reported but without a bibliographical reference or a clinical study report [30, 36, 45]. Procurement of autogenous bone graft from the distal femur has also been reported in the treatment of acute trauma and reconstructive procedures [46], bone tumors [47] and patellar reconstruction [48].
The major problems with autogenous bone graft are that harvesting usually requires a second surgical procedure, it may provide a limited mass of bone, it may cause pain, bleeding and infection at a previously uninjured site and it exhibits poor compressive strength that may lead to loss of correction and malunion. A number of disadvantages have also been documented with the use of several graft harvest sites. Iliac bone graft procurement requires a second surgical procedure thus increasing the needed time or personnel and may, finally, be associated with a keloid or a hypertrophic surgical scar. The use of the fibular head or shaft as autogenous bone graft is associated with a potential injury to the peroneal nerve and the anatomy of the area is permanently altered. Patellar autografting may not be sufficient for a large fracture cavity, while bone grafting from the greater trochanter has mechanical disadvantages, especially in older patients. [12, 49-55].
A wide variety of bone substitutes is available. It includes allografts (homogenous grafts) collected from cadavers or living donors, biomaterials such as xenografts (heterogenous grafts), and ceramics, osteoinductive growth factors, autogenous platelet concentrate, and the new innovational recently developed technologies such as mesenchymal stem cells and regional gene therapy. Bone substitutes avoid morbidity at the extraction site. Clinical studies have evaluated the efficacy of some of them in the treatment of tibial plateau fractures, while some others are not available yet for clinical use. They all have specific advantageous and disadvantageous mechanical and handling characteristics including safety and cost [54, 56-74].
The current study indicated that the use of the ipsilateral femoral condyle as a donor graft site for depressed tibial plateau fractures has specific advantages over other donor sites as well as over bone graft substitutes. The surgical time is not significantly elongated since only a proximal extension of the surgical approach, usually not exceeding 2cm, is needed and the patient is not exposed to an increased infection risk [23]. It also provides sufficient corticocancellous bone graft which has the advantages of structural support and bone inductive biologic capacity to prevent late articular subsidence [37, 60]. Moreover, the close proximity to the fracture site tends to reduce the impact of any eventual morbidity at the donor site. In addition, rehabilitation and recovery period is not affected, since the cavity of the femoral condyle is usually restored within the time that the patient remains non weight-bearing for the healing of the tibial plateau fracture. The potential complication risk of a cortical fracture is significantly diminished, since the cortical metaphyseal bone at the level above the physeal scar is soft and thin. Finally, the results of this study also indicated the lower cost of the procedure using autograft harvest from the ipsilateral femoral condyle versus bone substitute cost.
The available literature on the outcome of tibial plateau fractures in the elderly [75, 76] as well as on the influence of osteoporosis on fracture healing [77] is limited. A deterioration of bone tissue healing ability is expected in osteoporotic patients [78, 79]. However, earlier radiographic signs of external bone healing, than those of the autograft group, were detected at the graft donor site in our osteoporotic patients. It could be due to an increased osteoblastic activity to balance the poor bone quality, especially in the first time period. Although this report showed a favorable outcome in the osteoporotic patients, its usefulness may not be sufficiently proved due to the limited number of treated cases.
CONCLUSION
The results of this study suggest that the use of the ipsilateral femoral condyle as a bone following open reduction and internal fixation of depressed tibial plateau fractures was associated with a reduction of the average time to fracture union as well as of the treatment expenses when compared with the bone substitute group.
CONFLICT OF INTEREST
The author certifies that he has no commercial associations (such as consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. The author received no financial support for this study.
ACKNOWLEDGEMENTS
Declared none.


