RESEARCH ARTICLE
Use of Cemented Spacer with a Handmade Stem to Treat Acute Periprosthetic Tibial Fracture Infection: A Case Report
LluÍs Font-Vizcarra*, 1, Oscar Izquierdo1, Laura GarcÍa-NuÑo1, Araceli GonzÁlez2, VicenÇ Diaz-Brito3, Juan Castellanos1
Article Information
Identifiers and Pagination:
Year: 2014Volume: 8
First Page: 24
Last Page: 26
Publisher ID: TOORTHJ-8-24
DOI: 10.2174/1874325001408010024
Article History:
Received Date: 8/10/2013Revision Received Date: 3/12/2013
Acceptance Date: 7/1/2014
Electronic publication date: 24/1/2014
Collection year: 2014

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.5/) which permits unrestrictive use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
We report an 85-year-old woman with dementia and dependent for normal life activities who was admitted due to a left periprosthetic tibial fracture. The tibial component was replaced by one with a long stem and she was discharged. Four weeks after the intervention the patient was re-admitted due to an acute prosthetic joint infection. All the components were removed and a bone-cement spacer with a handmade stem with a metal core was implanted. Radiological signs of fracture consolidation were observed after 3 months of follow-up. Due to the previous health status of the patient, it was decided to keep the spacer as a definitive treatment. After 24 months, the patient was able to sit without pain and to stand up with help using a knee brace. There were no radiological or clinical signs of infection.
INTRODUCTION
In contrast to fractures of the distal femur or patella associated with a total knee arthroplasty (TKA), periprosthetic fractures of the tibia are very uncommon [1]. The largest series reported by Felix et al., [2] classified these fractures according to the anatomical location of the fracture and prosthesis fixation. Fractures associated with a well-fixed prosthesis could be successfully treated with the usual principles of fracture management, while those associated with loosening of the components require a revision arthroplasty.
Infection after treatment of this type of fracture has no frequently been described. In these cases, the fracture repair and the treatment of the infection is a challenge for the surgeon. We present a case managed with an antibiotic-loaded bone cement spacer with handmade stem and a metal core. To the best of our knowledge, this surgical procedure has not been previously reported in similar cases.
CASE PRESENTATION
An 85-year-old woman with hypertension, dementia and dependent for normal life activities presented after an accidental fall with a left periprosthetic tibial fracture around total knee arthroplasty (Alpina®, Biomet-France) implanted 9 years ago (Fig. 1). The fracture was classified as type IIB according to the Felix classification [2] (adjacent to the stem and with an unstable tibial component). To treat this lesion, areplacement of the tibial component by one with a long stem was performed (Fig. 2). Although the patient was discharged two weeks later without clinical complications, she was readmitted 4 weeks after the intervention due to wound drainage. Acute prosthetic joint infection was suspected and a surgical debridement was performed. The intraoperative cultures were positive for extended-spectrum beta-lactamase (ESBL) producing Escherichia coli and ampicillin- and high
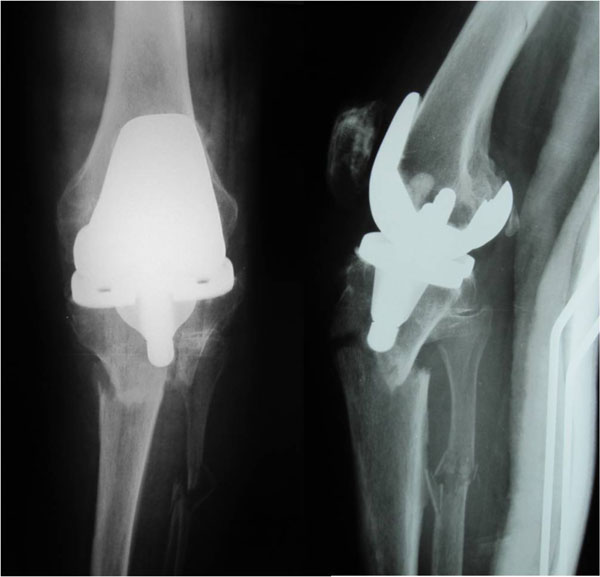 |
Fig. (1). AP and lateral X-rays showing type IIB periprosthetic tibial fracture. |
 |
Fig. (2). AP and lateral post-surgical X-rays after the replacement of tibial component. |
level gentamicin-resistant Enterococcus faecium. Despite this surgical approach and parenteral antibiotherapy with vancomycin and imipenem, the clinical evolution was non-satisfactory, so after three days, all components were removed and a bone-cement spacer coated with clindamycin and gentamicin and a handmade stem with a metal core was implanted (Fig. 3). The stem was made using the following
 |
Fig. (3). AP and lateral X-rays after implantation of bone-cement spacer coated with clindamycin and gentamicin and a handmade stem with a metal core. |
technique: first, the cement was injected using a cement gun into a mold (although we used the tube used for cementing the femoral component of hip prosthesis, other molds, such as chest tubes, could be used) [3]. After this, a Kischner wire was inserted into the tube and buried in the cement leaving about an inch uncovered to allow for connecting it with the tibial plateau cement spacer. The limb was immobilized with knee extension with an orthosis for 4 weeks to control rotational forces at the level of the fracture focus. The wound evolution was correct except for a skin defect at the level of tibial tuberosity that required a neurocutaneous pedicled graft. Based on antibiogram, specific-parenteral antibiotherapy (imipenem 28 days + vancomycin 17 days followed by 11 days of linezolid) was prescribed. The patient was discharged with an articulated knee brace. Radiological signs of fracture consolidation were observed after 3 months of follow-up. Due to the previous health status of the patient and short life expectancy, it was decided to keep the spacer as definitive treatment. In the latest follow-up (24 months after surgery), the patient was able to sit without pain and to stand with help using a knee brace. There were no radiological (Fig. 4), clinical (Fig. 5), or blood analysis signs of infection.
 |
Fig. (4). AP and lateral X-rays at 24 months follow-up. |
 |
Fig. (5). Images showing the clinical aspect of the knee at the end of follow-up. |
DISCUSSION
Surgical debridement and prosthesis retention is the recommended surgical approach to acute prosthetic joint infections [4]; however, when this initial approach fails, the replacement of all components in one or two steps is recommended. Infected non-unions require procedures to control infection, to provide stability, and to achieve union. In order to control the infection, surgical debridement and systemic antibiotherapy are required, and the use of local antibiotics at the infection site is advisable. Classically, fracture stabilization has been managed using external fixation [5]. However, a high prevalence of pin-site infections has been observed in association with external fixation [6]. Moreover, some patients do not tolerate the use of these devices. Therefore, in recent years, internal fixation using various devices with antibiotic-impregnated cement has been reported: cement-coated intramedullary nails [7], Ender or Küntscher nails coated with antibiotic-impregnated cement [8, 9] and antibiotic cement rods [3]. These strategies allow stabilization concurrent with local antibiotic elution.
An acute prosthetic joint infection around a non-consolidated periprosthetic tibial fracture is an exceptional complication which to our knowledge, has not previously been reported. In our case, external fixation was ruled out due to her general condition. Amputation is a technique also associated with a high rate of complications in such patients. Therefore, we decided to use a personal modification of the previously described technique for preparing antibiotic cement rods [3] that consisted of a cement stem with a Kirschner wire as metal core combined with an antibiotic-loaded cement spacer (Biomet). With this device, we controlled the axial and sagittal forces but we needed to use a brace to control rotation of fragments. Due to the high risk of complications, and in agreement with the patient’s family, we decided to keep the spacer as definitive treatment. Fracture healed, and the patient is still alive. However, we think that leaving a cement spacer as definitive treatment is only indicated in selected cases, for instance elderly patients with multiple co-morbidities, short life expectancy and very low level of activity. In the rest of patients, this treatment should be used as the first step of two-stages surgery. The value of our report is that it documents an inexpensive reproducible surgical technique as an alternative to external fixation for treatment of an acute septic non-union of a periprosthetic tibial fracture. However, this is a personal experience with a single case, so more studies are needed to corroborate our results and verify the utility and practicality of this surgical technique.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ETHICAL APPROVAL
Written informed consent was obtained from family members of the patient for publication of this case report and accompanying images.
ACKNOWLEDGEMENTS
We thank the Department of Research and Innovation of Parc Sanitari Sant Joan de Déu and specially Dr. Haro, Dr. Pares and Mrs. Elena Romero for their support during the progress of preparation of the manuscript.







