All published articles of this journal are available on ScienceDirect.
Translation of Oswestry Disability Index into Tamil with Cross Cultural Adaptation and Evaluation of Reliability and Validity§
Abstract
Study Design:
Prospective longitudinal validation study
Objective:
To translate and cross-culturally adapt the Oswestry Disability Index (ODI) to the Tamil language (ODI-T), and to evaluate its reliability and construct validity.
Summary of Background Data:
ODI is widely used as a disease specific questionnaire in back pain patients to evaluate pain and disability. A thorough literature search revealed that the Tamil version of the ODI has not been previously published.
Methods:
The ODI was translated and cross-culturally adapted to the Tamil language according to established guidelines. 30 subjects (16 women and 14 men) with a mean age of 42.7 years (S.D. 13.6; Range 22 - 69) with low back pain were recruited to assess the psychometric properties of the ODI-T Questionnaire. Patients completed the ODI-T, Roland-Morris disability questionnaire (RMDQ), VAS-pain and VAS-disability at baseline and 24-72 hours from the baseline visit.
Results:
The ODI-T displayed a high degree of internal consistency, with a Cronbach's alpha of 0.92. The test-retest reliability was high (n=30) with an ICC of 0.92 (95% CI, 0.84 to 0.96) and a mean re-test difference of 2.6 points lower on re-test. The ODI-T scores exhibited a strong correlation with the RMDQ scores (r = 0.82) p<0.01, VAS-P (r = 0.78) p<0.01 and VAS-D (r = 0.81) p<0.01. Moderate to low correlations were observed between the ODI-T and lumbar ROM (r = -0.27 to -0.53). All the hypotheses that were constructed apriori were supported.
Conclusion:
The Tamil version of the ODI Questionnaire is a valid and reliable tool that can be used to measure subjective outcomes of pain and disability in Tamil speaking patients with low back pain.
INTRODUCTION
Low back pain (LBP) is a common source of pain and disability and a major health problem across the globe. Estimates of lifetime incidence of low back pain range from 60 to 80% [1]. More than 80-90% of the people who experience low back pain are expected to recover within 6 weeks [2]. Measuring pain and disability are important to set goals, plan treatment and assess outcomes in LBP patients. To quantify patients’ self-assessment pain of their disability we need valid, reliable and responsive self-report measures. The Food and Drug Administration (FDA) recommends the use of patient reported outcome measures (PRO) to capture patients’ own assessment of their pain and disability [3]. The Oswestry Disability index (ODI) is a valid and reliable self-reported measure widely used as a disease specific questionnaire to evaluate pain and disability resulting from LBP [4]. The ODI has more than 200 citations in the science citation index. It has been translated in more than 10 different languages and all of them were found to be comparable with the original English version in terms of validity and reliability [5, 6]. Tamil is a language that is spoken across the globe by over 76 million people [7] and is an official language in India, Sri Lanka and Singapore. Furthermore, Tamil speaking immigrants populate countries around the world. Since the original English version of ODI is designed to cater to the needs of patients in corresponding countries and culture, it is not effective in assessment of pain and disability in LBP patients whose primary language is Tamil. No current validated Tamil version of the ODI has been published. The objectives of this study are to: 1) Carry out the translation and cross cultural adaptation of the ODI version 2.1 according to established guidelines into Tamil, and 2) Estimate the reliability and construct validity of the ODI-Tamil (ODI-T).
MATERIALS AND METHODOLOGY
This study had two phases:
Phase I- Cross-Cultural Adaptation Process
Permission was obtained from MAPI, the copyright owners of the ODI to translate and cross-culturally adapt the ODI into Tamil. Five step guidelines proposed by Beaton and Guillemin were followed [8-10] (see Fig. 1).
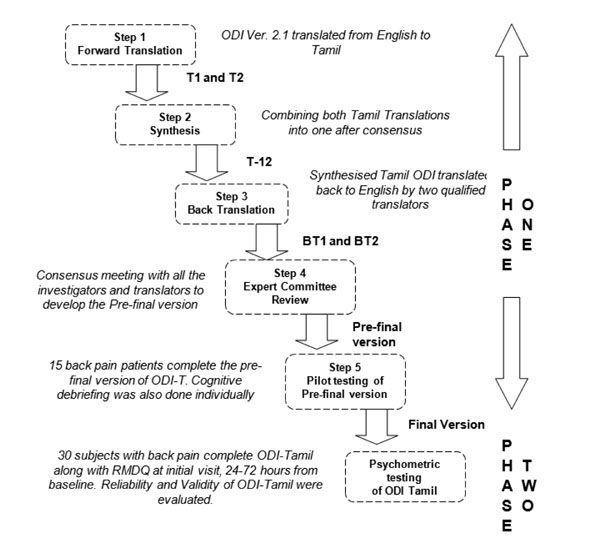
Flow chart describing the development of Tamil version of ODI.
1) Forward translation: Two professionally qualified translators who are bilingual in Tamil and English translated ODI from English to Tamil. This stage evolved two forward translations T1 and T2.
2) Synthesis: A synthesized version (T-12) was produced by combining both T1 and T2 after a reconciliation meeting between two translators and one of the authors (JV).
3) Back Translation: The synthesized version (T-12) was translated back into English by two independent qualified translators to identify inconsistencies in the words and concepts of the synthesized version. This was referred to as BT1 and BT2.
4) Expert committee review: An expert committee comprised of the investigators and all four translators met to discuss issues of cultural adaptations and linguistic equivalence with the original English version of the ODI. The outcome of this stage was the pre-final version of the ODI-T.
5) Pilot testing: The pre-final version of the ODI-T was administered to 15 Tamil speaking patients with back pain for a minimum of 6 months. The mean age of these patients was 41.27 years (SD 9.8). Upon completion of the questionnaire, cognitive debriefing was done individually. Respondent’s interpretation of items was investigated to evaluate whether the adapted version retained equivalence to the items of the English version.
Reports were prepared at each stage covering the issues faced and how they were resolved.
Phase II- Psychometric Evaluation Process
Subjects
The psychometric properties of the ODI-T were tested in a sample of 30 Tamil speaking LBP patients receiving outpatient physiotherapy treatment at a clinic in Chennai, India. They were recruited by the treating physiotherapist after obtaining written consent. Subjects of both sexes aged 20 years and above with LBP for any duration of time were included. They were excluded if they had cognitive impairment and communication problems. Patients were also excluded if their LBP was due to trauma or other secondary causes e.g. Cancer. There were 14 men and 16 women. The mean age was 42.7 years (S.D. 13.6; Range 22 - 69). The characteristics of the subjects are described in Table 1.
Baseline Patient Characteristics
| Characteristics | Values |
|---|---|
| Subjects (n) | 30 |
| Male/Female (n) | 14/16 |
| Age in years – mean (SD) | 42.7 (13.6) |
| Radiating pain –Yes: No (n) | 15:15 |
| Side of radiating pain - R : L : Bilateral (n) | 7:6:2 |
| Diagnosis | n (%) |
| Intervertebral disc prolapse | 13 (43.3) |
| Lumbar spondylosis | 7 (23.3) |
| Lumbosacral strain | 9 (30) |
| other causes | 1(3) |
* The values are expressed as mean and standard deviation (SD).
Outcome Measures
The Oswestry Disability Index Version 2.1a (ODI)
ODI was developed in the year 1980 by Fairbank et al. [4]. Since then different versions of the ODI have been published [5]. The ODI version 2.1 is recommended by the developers for clinical use and research purposes [5]. It consists of ten items to assess LBP and the difficulty it has caused in 9 different areas of everyday life [11]. Each section has 6 responses, scored from 0-5. Scores obtained in individual sections are summed up and converted to get a percentage. This percentage gives the patient-perceived level of disability, with “0” indicating no disability and a higher score indicating greater disability.
Roland-Morris Disability Questionnaire (RMDQ)
The RMDQ is a self-reported questionnaire developed in the year 1982 [12] used to evaluate the outcomes related to LBP. It has 24 items focusing on the disability caused due to LBP. The total score is the total number of items checked by the patient. The RMDQ scores range from 0 (no disability) to 24 (maximum disability) [13]. The RMDQ has been previously shown to correlate with the ODI [14]. The minimally important difference for RMDQ was identified as 4 points [15].
Visual Analog Scale for Pain (VAS-P)
The intensity of pain was assessed using the visual analog scale (VAS). It is a valid and reliable measure to report pain [16]. It has a 100 mm horizontal line with the left end of the line labelled as “no pain” and the right end as “severe pain”.
Visual Analog Scale for Disability (VAS-D)
Patient perceived disability was assessed using a 100 mm visual analog scale (VAS) [17] with the left end labeled as “no disability” and the right end of the scale as “severe disability”.
Procedure
This study was approved by the Health Sciences Research Ethics Board (HSREB) of the University of Western Ontario in London, Ontario, Canada. Informed consent was obtained from all the patients prior to their participation in the study. Data was collected at baseline and after 24-72 hours. At the initial visit, baseline assessment was performed after patients agreed to participate in the study. During both the visits they completed ODI-Tamil, RMDQ, VAS-P and VAS-D. Lumbar active ROM was also measured. All patients continued to receive their routine physiotherapy treatment as outpatients. This study in no way affected the routine treatment they received from their physiotherapists.
Statistical Analysis
With the data obtained the reliability and construct validity of the ODI-Tamil was evaluated using the SPSS software version 20. The level of statistical significance was set at p < 0.05.
Reliability
Reliability is a generic term used to indicate both the homogeneity (internal consistency) of a scale and the reproducibility (test–retest reliability) of scores [18]. Cronbach’s alpha was used to assess internal consistency of the ODI-T. For this purpose, the baseline ODI-T data was used. Internal consistency is considered acceptable when Cronbach’s alpha exceeds 0.70 [19]. Intra-class correlation coefficient (ICC) [18] was used for assessment of test–retest reliability between the ODI-T scores obtained at baseline and at second visit on a sample which was considered to be stable. We identified a subject to be stable if change in the subject’s RMDQ score was equal to or less than the MDC of RMDQ, which is 4 points. The ICC values ranges from 0 to 1; 1 = perfect reliability, 0.90 to 0.99 = very high correlation; 0.70 to 0.89 = high correlation; 0.50 to 0.69 = moderate correlation; 0.26 to 0.49 = low correlation and 0.00 to 0.25 = little, if any, reliability [20]. The Bland-Altman plot [21] is a measure of with-in subject variation and the limits of agreement were used to assess the agreement between the ODI-T scores at the two occasions [22, 23]. This was created by plotting mean difference in the ODI-T scores for the 2 occasions against the baseline ODI-T scores. 95% confidence interval around the mean difference was calculated and limits of agreement were also plotted [22].
Construct Validity
Construct validity was assessed by calculating Pearson’s correlation coefficients (r) [23] comparing the extent to which expected relationships between the various constructs were fulfilled using the ODI-T. Expected relationships were based on the literature. The r values yield the degree of correlation between two measures where, 0= no correlation between two scores and 1 or –1 = the absolute correlation between two scores. Pearson’s correlation coefficients are interpreted as follows: 0.00 to 0.19 = very weak correlation; 0.20 to 0.39 = weak correlation; 0.40 to 0.69 = moderate correlation; 0.70 to 0.89 = strong correlation; and 0.90 to 1 = very strong correlation [19, 24].
Based on previous studies with similar objectives and our clinical experience we hypothesized the following relationships between the various constructs apriori:
- ODI-T and RMDQ would have high correlation.
- VAS-P and VAS-D would have moderate to high correlations with ODI-T.
- Lumbar ROM would correlate the least with ODI-T.
RESULTS
Phase I- Cross Cultural Adaptation Process
The cross-cultural adaptation process was successful and we had minimal difficulty in achieving an acceptable translation. The word “conveniently positioned” in the second and the third response of section 3 in the original version was translated as “appropriate height” as this was the intended meaning. In section 4 that deals with walking, distances that were described in miles and yards in the original English version were converted into kilometers and meters as, SI units of length are more commonly in use among native Tamil speakers. In option 2 of section 5 the word “favourite chair” in original version was converted to “comfortable chair”, as the term favourite chair is not common in the Tamil culture. The pilot testing showed that the average time taken to complete the ODI-T was 4 minutes. Cognitive debriefing indicated that the perceived meaning of the questions was uniformly consistent with the intended meaning of the questionnaire. Since the pre-final version performed well in the pilot test it was accepted as the final version of the questionnaire. This final version was submitted to the developer. (See Appendix)
Phase II- Psychometric properties
Reliability
ODI-T exhibited excellent internal consistency shown by a Cronbach’s alpha value of 0.92. Test-Retest reliability of the ODI-T analyzed on stable subjects (n=30) yielded excellent results with very narrow confidence intervals [ICC=0.92 (95% C.I. = 0.84 - 0.96)] (see Table 2). The Bland and Altman plot indicated that the measure of with-in subject variation i.e. the bias was very minimal as the mean difference was close to zero [mean difference (d) = 2.63] and the limits of agreement were excellent (-7.15 to 12.41) with just one outlier (see Fig. 2 and Table 2).
Test Retest Reliability Results of ODI-T
| Outcome Measure | Baseline Score | Retest Score | ICC (95% C.I.) | Bland & Altman Analysis | |
|---|---|---|---|---|---|
| d (SD) | LOA | ||||
| ODI-T | 27.73(8.9)* | 25.1(9.8)* | 0.92 (0.84-0.96) | 2.63 (4.9) | 12.41 to -7.15 |
* The values are expressed as mean and standard deviation (SD); d – mean difference of the test and retest scores; LOA- Limits of agreement = d± 1.96 SD.
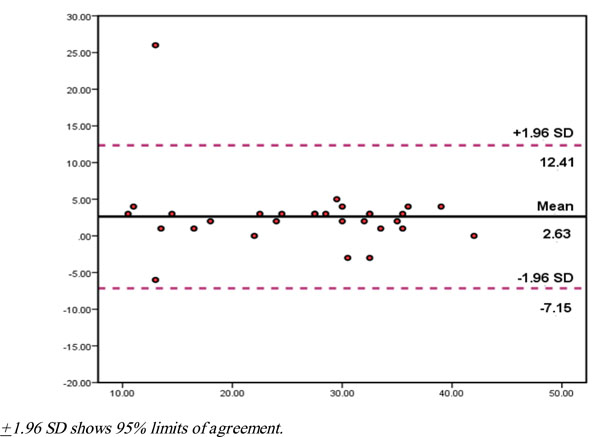
Bland and Altman plot for measuring with-in subject variation and the limits of agreement.
Construct Validity
All the correlations followed expected constructed relationships hypothesized apriori. The ODI-T scores correlated strongly with the RMDQ scores (r = 0.82), VAS-P (r = 0.78) and VAS-D (r=0.81p<0.01 (See Table 3). ODI-T scores were moderately correlated to flexion and extension ROM (r = -.51 and r = -0.53 respectively; p<0.01). Weak inverse correlations were observed between ODI-T scores and side flexion ROM scores (r = -0.27 to -0.30; NS).
Correlation Between the Various Constructs
| R (n=30) | ODI Score | RMDQ Score | VAS P | VAS D | Lumbar ROM |
|---|---|---|---|---|---|
| ODI score | 1 | ||||
| RMDQ score | 0.82** | 1 | |||
| VAS Pain | 0.78 ** | 0.82** | 1 | ||
| VAS Disability | 0.81** | 0.86** | 0.84** | 1 | |
| Lumbar ROM | -0.51** to -0.27* | -0.52** to -0.16* | -0.56** to -0.25* | -0.73** to -0.40*** | 1 |
The values are expressed as Pearson’s correlation coefficient (r); * Not significant; ** p<0.01; *** p<0.05 ODI-T- Oswestry Disability Index-Tamil; RMDQ- Roland-Morris Disability Questionnaire; VAS-P- Visual Analog Scale-Pain; VAS-D- Visual Analog Scale-Disability; Lumbar ROM- Lumbar range of motion (flexion, extension and Side flexion).
DISCUSSION
The results of this current study provide us with the preliminary evidence that the ODI-T is a reliable and valid measure to assess disability in Tamil-speaking LBP patients.
The high internal consistency value of the ODI-T (0.92) was consistent with the original English version (0.87) [25] and other translated versions in Chinese (0.90) [26] Brazilian Portuguese (0.87) [27], German (0.90) [28] and Italian (0.85) [29]. The fact that the Cronbach’s alpha was less than 0.95 supports the current format of ODI-T, as a very high Cronbach’s alpha would indicate redundancy of items [23]. However we recommend further tests of dimensionality like Rasch analysis [30] and confirmatory factor analysis [31] to confirm the unidimensionality of the ODI-T.
The observed test re-test reliability value was high (ICC=0.92) which was comparable to the ICC reported for the original English version (0.91) [4]. This clearly supports the reproducibility of the results of the ODI-T which is one of the essential measurement properties required for any instrument. The narrow confidence intervals that were obtained for the ICCs clearly indicates that this questionnaire can yield reliable results when administered at multiple occasions. The fact that all but one measurement fell within the 95% CI around the mean difference during the Bland and Altman analysis points out to a very strong agreement between the scores obtained at the 2 occasions with very minimal within-in subject variation, strongly backing up the ICCs obtained. However this should be read with caution as the sample size was very small. We recommend studies with larger sample size to confirm the reliability indices obtained in this study.
Construct validity of the ODI-T was supported by the high correlation observed between ODI-T and RMDQ (r=0.82); although this is slightly higher than others reported for the Chinese (r=0.76) [26] and Brazilian Portuguese (r= 0.81) [27] versions, the rank order of correlations is consistent with other studies. These results again strengthen the argument that the ODI and the RMDQ measure the same construct of disability that arises due to back pain.
The VAS-P correlation to the ODI-T (r=0.78) was slightly higher than or equal to what was reported for other translations (Brazilian Portuguese version r=0.66 [27], Chinese r=0.68 [26] and German r=0.78 [28]). These results strengthen the consistency of the results of the ODI across translations since other translations have included a higher proportion of chronic cases, sample differences may have contributed to the slight difference that was observed between versions.
This study adds some more input into the validity of the VAS-D which is interesting as there are not many studies that are available on its validity and reliability. The results of the current study (large correlations with ODI-T, RMDQ and VAS-P; moderate to large correlations with lumbar ROM) (see Table 3) are quite different and support the validity of the VAS-D unlike the study by Boonstra et al., where they concluded that the validity of VAS-D is questionable [17]. A new finding was the high correlation observed between the ODI-T and VAS-D (r=0.81), which suggests that the ODI-T correlates similarly with both pain and disability.
Lumbar range of motion values have been reported to correlate poorly with disability measures [32]. The ODI-T demonstrated a low to moderate inverse correlation with the lumbar range of motion values (r=-0.27 to-0.53). This is similar to the range of correlations reported by Gronblad [13]. Overall, the similarity between correlations in this study and our constructed hypotheses based on previous translations provide support for the construct validity of the ODI-T.
There are a few limitations in this study, most notably the relatively small sample size. Despite this, our confidence intervals around our reliability coefficients were sufficiently precise to be confident that we had excellent reliability. Future longitudinal studies with larger samples should focus on responsiveness, factor analysis and/or Rasch analysis. These would provide additional information on the performance of the ODI-T including structure validity, the potential for differential functioning of items and other measurement properties.
Overall, the observed psychometric properties were consistent with those reported both for the English and other translated versions. Combining the quantitative data with the evidence from the cognitive interviews, supports our conclusion that the ODI-T is a valid and reliable means of measuring change in pain and disability in low back pain patients who are Tamil speaking.
CONCLUSION
Our study results suggest that the Oswestry Disability Index version 2.1 has been successfully translated and cross-culturally adapted from English to Tamil. The preliminary evidence generated by the psychometric testing showed that the Tamil version of the Oswestry disability index demonstrates psychometric properties similar to the English version. Future studies with large sample sizes are needed to confirm these preliminary findings.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.
APPENDIX



