All published articles of this journal are available on ScienceDirect.
The Outcome of Bone Substitute Wedges in Medial Opening High Tibial Osteotomy
Abstract
Background:
Opening wedge high tibial osteotomy often requires bone grafting to improve the union rate and avoid instability at the osteotomy site. Autograft and allograft have both been associated with complications and the use of bone substitute wedges has been advocated to improve the outcome. This study investigated the clinical, radiological and histological outcomes of using biphasic calcium phosphate ceramic (Triosite) wedges in opening wedge high tibial osteotomy and determined whether the presence of the graft would compromise the satisfactory conversion to a total knee replacement.
Methods:
A consecutive cohort underwent radiological review to determine whether the osteotomy healed and the correction was maintained. Biopsies were performed on those undergoing second procedures. All patients converted to total knee arthroplasty were assessed separately as to any surgical complications attributed to the Triosite wedge.
Results:
There were 36 osteotomies in 33 patients with a minimum of 4 years follow up. All osteotomies healed. There was an average 90 (5-14) of correction, which was maintained. Histological assessment of 17 cases confirmed adequate bone replacement of the Triosite although some areas of tricalcium phosphate remained visible. Conversion to a total knee arthroplasty occurred in 11 cases with no complications.
Conclusion:
Biphasic calcium phosphate ceramic wedges (Triosite) can be reliably used in opening wedge high tibial osteotomy with a low incidence of complications and satisfactory conversion to total knee arthroplasty.
INTRODUCTION
High tibial osteotomy (HTO) is a common treatment option in patients with medial compartment knee osteoarthritis and can be performed through either a medial opening wedge or a lateral closing wedge technique. Our preferred technique is an oblique medial opening wedge osteotomy performed at the level of the tibial tubercle [1] which has the advantages of avoiding the patellar tendon and any potential scarring of the extensor mechanism. This osteotomy also enables the surgeon to avoid any of the co-morbidities associated with a concurrent fibula osteotomy. This technique creates a wedge shaped defect in the bone, which can be managed either by leaving to heal or grafting with bone, bone substitute or other synthetic materials.
Traditionally opening wedge osteotomy sites have been grafted with autograft [2], which is considered the most osteoconductive and osteoinductive option. However, harvesting bone graft is associated with increased morbidity including prolonged operative time, increased pain, hematoma and infections at the donor site [3-8]. Allograft can be used to eliminate these complications but is associated with the possibility of disease transmission and it is less effective at stimulating bone healing [4-6].
In an attempt to avoid these co-morbidities bone substitutes have been developed. These have proven to be a safer alternative as they cannot cause disease transmission and may be associated with accelerated bone healing and remodeling leading to faster recovery times and earlier weight bearing [4-6,8]. Bone substitute wedges often appear as well delineated areas on radiographs several years following the osteotomy and this failure of full incorporation raises the question of the mechanical strength of the tibia and whether it will be suitable to undergo conversion to a total knee replacement when required.
We wished to establish whether using synthetic grafts in medial oblique opening high tibial osteotomies would result in acceptable clinical, radiological and histological outcomes and whether the continued radiological presence of the graft would prohibit the satisfactory conversion to a total knee replacement.
MATERIALS AND METHODS
A single surgeons (GH) database was retrospectively reviewed to identify all oblique medial HTOs in which bone substitute wedges were utilized to fill the gap in an oblique medial opening wedge osteotomy.
Between July 2002 and April 2009 bone substitute wedges were utilized in 36 consecutive oblique medial HTO in 33 patients (26 males, 7 females) with an average age of 45 years (range 21 – 57years). All patients were followed for a minimum of 4 years.
Surgical Technique
A detailed description of the oblique upper tibial opening wedge osteotomy surgical technique and its philosophy has been previously reported [1]. A straight 12-cm incision was created starting at the tibial tubercle medially and continuing distally parallel to the tibial crest exposing the proximal tibia. Using a thin saw blade, the oblique osteotomy started at the distal end of the medial collateral ligament insertion and ran below the tibial tubercle at approximately 60° distal-medial to proximal-lateral, finishing in the lateral flare of the proximal tibial metaphysis just distal to the proximal tibiofibular joint. Care was taken to leave the lateral tibial cortex intact. The osteotomy site was opened medially, normally 10-12mm, with gentle manual pressure until the mechanical axis was corrected. To maintain the correction appropriately sized bone substitute wedges were inserted in the osteotomy gap. A ‘low profile’ T-plate was then contoured to the anteromedial tibial border and secured with 4-6 non-locking cancellous screws. The wound was closed with a subcuticular suture (Fig. 1).

A 42 year-old male with bilateral genu varum (A) underwent staged bilateral oblique opening wedge high tibial osteotomies. (B) shows early healing of the right side at 6 weeks with satisfactory alignment.
Patients were mobilized, without bracing, touch weight bearing for 4-6 weeks, progressing to full weight bearing by 8-12 weeks.
Bone Substitute Wedges
In all cases biphasic calcium phosphate ceramic wedges (Triosite, Zimmer) were used. This osteoconductive scaffold was a combination of hydroxyapatite (HA) (60%) and the more soluble beta-tricalcium phosphate (β-TCP) (40%) designed to gradually dissolve releasing calcium and phosphate. The porosity of 60-70% was composed of macropores (300-600microns) and micropores (<10microns), sized to optimized bony in-growth. The wedges were 30 x 30mm2 and were available in various dimensions (3.0 x 6.0mm – 6.0 x 12.0mm).
The demographics, surgical indication, radiological parameters (femorotibial alignment at pre-operative, post-operative and post-union time points), size of bone substitute wedge, union rates and adverse events including rates of second surgery were recorded for each patient. Union was declared when the osteotomy gap was bridged by callus in at least 3 of 4 interfaces, as viewed on AP and lateral plain radiographs.
During second surgeries for plate removal +/- conversion to total knee arthroplasty, biopsies of the osteotomy site were obtained and analyzed histologically to assess bony in-growth into the bone substitute matrix. The biopsies comprised a longitudinal sliver of bone/graft/bone obtained with an osteotome and were independently reviewed by a pathologist.
Patients who required conversion to a total knee replacement were reviewed separately to establish whether the radiological presence of the bone substitute wedge complicated the procedure or the final outcome. All patients were reviewed radiologically at a minimum of 12 months following the total knee replacement.
RESULTS
The primary indication for oblique medial HTO was medial compartment osteoarthritis with varus alignment in 35 (97%) of 36 patients. In a single case excessive varus alignment was corrected to off load the medial compartment following a medial femoral condyle osteochondral fracture.
Patients received 5 x 10mm (42%) or 6 x 12mm (58%) Triosite wedges. No osteoinductive agents were added. No adverse local inflammatory reactions to the graft were noted. An isolated case (2.8%) of superficial infection settled with intravenous antibiotics. A single case of non-union (2.8%) and deep wound infection (2.8%) occurred in the same 52-year-old patient. At his initial surgery the lateral tibia cortex was violated during opening of the osteotomy. Additional fixation, comprising of a single lag screw, was used at the lateral cortical breach in an attempt to support the medial construct. Over time he had repeated falls and serial images confirmed loss of correction and eventual non-union. Twelve months following his index procedure he underwent revision fixation and iliac crest bone grafting following which union occurred. Seventeen months following revision he developed a deep wound infection without joint involvement that required plate removal and intravenous antibiotics to eradicate the infection, he subsequently underwent satisfactory revision to a total knee replacement.
The remainder of the cohort united and no other patients had recurrence of their varus deformities.
Femorotibial alignment, measured on AP weight-bearing long leg radiographs averaged 182° pre-operatively and 173° post-operatively for an average correction of 9° (range 5-14°). Following union the femorotibial alignment averaged 174°. The Trisoite (Zimmer) wedges remained radiologically visible in all cases even those out to 9 years post implantation (Fig. 2).

Appearances of the tibia 4 years following HTO and subsequent plate removal. The Triosite wedge was still visible radiologically.
At intervals of 11 – 74 months post the index procedure 11 patients underwent conversion to a total knee arthroplasty. Despite radiographically visible residual bone substitute all arthroplasties were performed without any problems at the osteotomy site. The surgical procedure was performed through a standard medial para-patellar incision without the need of either a quadriceps snip or tibial tubercle osteotomy to enhance the exposure. Primary components were used in all cases without the use of stems. At 12 months all arthroplasties were functioning well with a range of motion from 100° to 125° and a satisfactory clinical outcome (Fig. 3).

Anteroposterior and lateral radiographs taken one year following conversion to total knee replacement. The visible Triosite graft did not compromise the surgical procedure and rehabilitation programme.
In a further 6 cases the plate was removed in isolation. During both second surgery scenarios biopsies were taken of the osteotomy site. White granular material was macroscopically visible at the osteotomy site in amounts relative to the duration since the index procedure. The histological analysis of all of these confirmed abundant bony infiltration of the synthetic scaffold with areas of residual graft surrounded by new bone formation (Fig. 4).
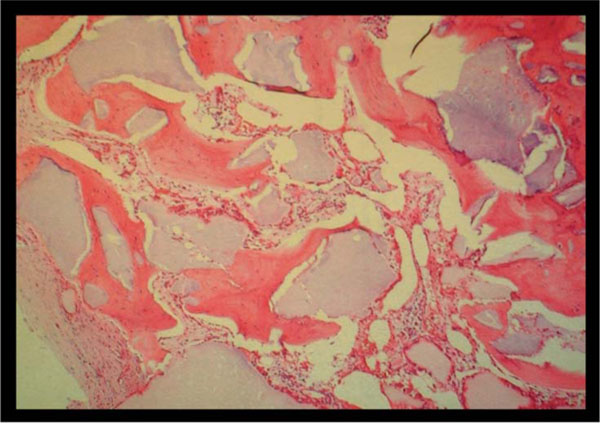
The histological appearances at three years post oblique medial HTO using Triosite (Zimmer) wedge. Although remnants of the synthetic graft remain visible (purple amorphous areas) histological analysis confirms the presence of viable bone within the remaining matrix.
DISCUSSION
HTO is a valuable operation in a young, active population with medial compartment osteoarthritis and a varus knee deformity. The key to success is maintaining correction as well as stability of the osteotomy. Medial opening wedge osteotomy creates a defect which is inherently unstable and although the original technique suggested that no graft was required to fill the defect more recent literature (Zorzi et al. [8]) has shown that the complication rates, including delayed union and loss of correction, were higher in patients where graft was not used. Bone substitute grafts such as triosite are not only easy to use intra-operatively with fewer co-morbidities, but they provide stability to the construct and do not affect further operative procedures. Although all of the participants in this study had radiologically visible triosite grafts at maximum follow up, all constructs remained mechanically stable with no episodes of re-fracture at the osteotomy site and no recurrence of the varus deformity.
Radiological union has been difficult to define with recent studies utilizing an evaluation system outlined by van Hermet et al. [6]. This rating system was modified from McKibbin’s description of fracture healing [10] and compares radiological findings with known bone healing phases. Using this system all of the patients in this study were at the consolidation phase (phase 4) where the bone has healed, however the bone substitute was still recognizable, as full reformation had not yet occurred. No patients in this study progressed to phase 5 of remodeling where there was full reformation and the osteotomy site was no longer visible. The results of the biopsies at secondary surgery confirmed that all had abundant bony infiltration, although areas of the graft still remained visible. This incomplete resorption of the graft was not associated with increased complications, in particular, loss of correction or secondary fracture, suggesting that phase 5 of remodeling is not necessary for a successful long term outcome.
Most studies in the current literature look at the use of either β-TCP or HA bone substitutes. The bone substitute used in this study was a composition of both HA and the more soluble β-TCP, to our knowledge there are no other studies involving similar bone substitute compositions. Koshino et al. [9] have shown that HA bone blocks remain visible on X-ray at 3 years post HTO. They also report that on removing the bone blocks there was macroscopic bone formation on the substitute suggesting again that despite incomplete resorption the bone substitute does promote bony ingrowth and maintains stability. Studies utilizing β-TCP bone substitutes have reported full resorption [6,11,12] in some of the study population, however others including Gaasbeek et al. [5] found the β-TCP was still visible on X-ray at maximum follow up. This discrepancy may be due to the site of use as both Muschik et al. [11] and Erbe et al. [12] reported studies using β-TCP graft in spinal fusion, where the graft is not under axial load.
Few previous studies have looked at conversion to total knee arthroplasty following medial opening wedge HTO with bone substitute in situ. Kraal et al. [4] published a series of 17 patients with 21 knees undergoing medial opening wedge HTO using rigid β-TCP in which 6 knees were converted to arthroplasty (5 total knee replacements and 1 unicompartmental arthroplasty). There were no complications noted during the revision procedure and no interference of the β-TCP wedges during or after the surgery. We have shown that conversion to total knee arthroplasty using Triosite wedges also results in a satisfactory outcome despite the continuing radiological presence of the graft. We developed this oblique osteotomy [1] at the tibial tubercle, to avoid damage to juxta-articular structures such as the patellar tendon, which can cause patellar infra and resultant difficulty in the exposure when converting to total knee arthroplasty. All conversion procedures in this study were achieved without extension of the routine medial para-patellar approach, confirming that this osteotomy does allow simple conversion to arthroplasty.
CONCLUSION
Medial opening wedge HTO is a safe and efficacious treatment option in patients with a varus deformity. The use of bone substitute wedges eliminates donor site morbidity without compromising the outcome. Despite radiologically visible grafts there is notable bony ingrowth histologically and the osteotomies remain mechanically sound, including those who have gone on to have a subsequent knee replacement.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


