RESEARCH ARTICLE
Cost-Effectiveness of Image-Guided Spine Surgery
Robert Green Watkins, IV*, 1 , Akash Gupta2, Robert Green Watkins, III1
Article Information
Identifiers and Pagination:
Year: 2010Volume: 4
First Page: 228
Last Page: 233
Publisher ID: TOORTHJ-4-228
DOI: 10.2174/1874325001004010228
Article History:
Received Date: 28/5/2010Revision Received Date: 23/6/2010
Acceptance Date: 25/6/2010
Electronic publication date: 6/8/2010
Collection year: 2010

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Objective:
To determine if image-guided spine surgery is cost effective.
Methods:
A prospective case series of the first 100 patients undergoing thoracolumbar pedicle screw instrumentation under image-guidance was compared to a retrospective control group of the last 100 patients who underwent screw placement prior to the use of image-guidance. The image-guidance system was NaviVision (Vector Vision-BrainLAB) and Arcadis Orbic (Siemens).
Results:
The rate of revision surgery was reduced from 3% to 0% with the use of image guidance (p=0.08). The cost savings of image guidance for the placement of pedicle screws was $71,286 per 100 cases. Time required for pedicle screw placement with image guidance was 20 minutes for 2 screws, 29 minutes for 4 screws, 38 minutes for 6 screws, and 50 min for 8 screws. Cost savings for the time required for placement of pedicle screws with image guidance can be estimated by subtracting the time required with currently used techniques without image guidance from the above averages, then multiplying by $93 per minute. The approximate costs of the navigation system is $475,000 ( $225,000 for Vector Vision-BrainLAB and $250,000 for Arcadis Orbic-Siemens).
Conclusion:
Image guidance for the placement of pedicle screws may be cost effective in spine practices with heavy volume, that perform surgery in difficult cases, and that require long surgical times for the placement of pedicle screws.
INTRODUCTION
Pedicle screws are commonly used to assist in fusion of the thoracic and lumbar spine. Most surgeons have confidence in their ability to accurately place pedicle screws via various techniques. However, misplaced screws can cause nerve damage, failure of fixation, and revision surgery. Neurologic deficits after pedicle screw surgery have been reported to occur up to 5% of the time [1, 2].
Misplaced pedicle screw rates with traditional techniques have been reported to be 10-42% [3-14]. Previous image guided studies have shown misplaced rates of 0-9% [15-20]. Despite reports of improved accuracy, use of image guidance for spine surgery has not become the standard of care. Limitations on the use of image guidance include the cost of purchase of the systems, time required for usage in the operating room, and questionable accuracy of the systems.
Our hypothesis is that image guidance for the placement of pedicle screws will decrease the cost of healthcare. Our study entailed a prospective case series of the first 100 patients undergoing thoracolumbar pedicle screw instrumentation under image-guidance was compared to a retrospective control group of the last 100 patients who underwent screw placement prior to the use of image-guidance. The Arcadis Orbic 3D (Siemens Medical, Munich, Germany) acquires a three-dimensional image in the operating room and the NaviVision (BrainLAB AG, Feldkirchen, Germany) navigation system allows real-time image guidance for the placement of instrumentation.
This study documents time required for usage of image guidance in the operating room, accuracy of pedicle screw placement, complications of the image guidance systems, and radiation doses to the surgeon. Additionally, this study entails a retrospective review of a case control group of patients with pedicle screw fixation prior to the use of image guidance. Analysis of the potential cost savings of image guidance based on the cost of reoperations and time spent in the operating room is performed.
MATERIALS AND METHODOLOGY
We began using the Arcadis Orbic 3D and NaviVision navigation systems in May, 2007. These systems were used for the placement of every pedicle screw inserted for 100 consecutive patients undergoing open thoracolumbar fusion. Prospective data was collected in terms of time, accuracy, radiation exposure, complications, and reoperations.
Our method for pedicle screw insertion with image guidance is as follows. We expose the pars interarticularis, base of the superior facet joint, and transverse process at every level to receive a pedicle screw. While the surgeons are exposing the spine, the surgical technician registers the instruments with the NaviVision system. The NaviVision frame is placed via a clamp on to the spinous process of the middle vertebral body. For example, the clamp is placed on L5 for fusion of L4-S1. The Arcadis Orbic 3D images at least three vertebral bodies, therefore pedicle screws can be inserted into three vertebral bodies with one imaging cycle.
All metal is removed from the field of view of the image, including sponges, retractors, and electrocautery cords. The posterior spinal wound is filled with normal saline. A sterile drape is placed over the patient. A slit in the drape allows the navigation frame to protrude out. A clear plastic bag is placed over the navigation frame, so that the navigation camera can detect the Marker Spheres on the reference frame yet remain sterile.
The Arcadis Orbic 3D is brought into the surgical field without a sterile cover. The patient is covered, not the imager. After an anteroposterior and lateral image confirm that the desired levels are centered on the radiograph, the three-dimensional image is acquired. The original Siemens imager was called the ISO-C because it has an isocentric center that the imager revolves around. If the spine is centered on the anteroposterior and lateral images then it will be centered on all of the images as the machine rotates around the patient. Ventilation of the patient is stopped, as the imager performs a 180º semi-revolution taking 100 images in 2 minutes. (The oxygen saturation remains at 100% during this time.) Computer generated three-dimensional images are constructed from these two-dimensional images. The Arcadis Orbic 3D, the latest version of the ISO-C, provides improved quality of the image compared to the ISO-C. During image acquisition, the surgeon stands behind a lead shield or exits the room.
The Arcadis Orbic 3D sends the three-dimensional image to the NaviVision navigation system. The drape is removed from on top of the surgical field and two sterile drapes are secured on both sides of the patient. A Wiltse retractor is inserted from the cephalad direction of the wound, so it does not interfere with the navigation frame attached to the spinous process which is directed caudally towards the navigation camera at the foot of the bed.
A divot is made in the cephalad lamina with the awl. The image-guided probe is inserted into the divot to register the divot as a checkpoint. The divot can be checked throughout the case (with the image-guided probe) to know if the frame attached to the spinous process at the caudal level has moved in relation to this point.
The awl and the pedicle finder are registered with the “pre-calibrated” stars. The tap is registered with the “calibrate with ICM-4” star. A freehand star is attached to the pedicle screw inserter handle and registered with the ICM-4.
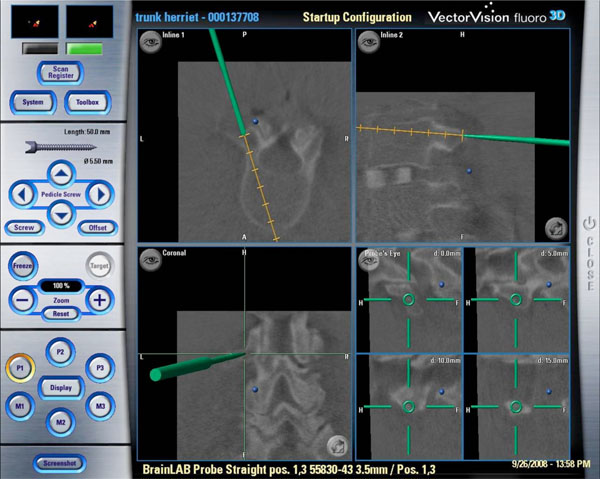
The pedicle hole is started with the awl, opened with the pedicle finder, probed, tapped, probed again, then the screw is inserted. The navigation system shows the position and trajectory of the tip of these instruments on the navigation screen (Fig. 1).
After all screws are inserted, electromyographic testing of the screw is performed.
Patients were routinely followed after the surgery at two weeks, six weeks, and every three months.
The time spent for placement of pedicle screws was measured after exposure of the spine. It includes placement of the reference frame, preparation of the field, image acquisition, instrument registration, and placement of pedicle screws.
Accuracy of pedicle screw placement was based on intraoperative electromyography stimulation of the pedicle screws and reoperation rates due to misplaced screws. Radiation exposure of the surgeon was based on a radiation badge that the surgeon wore under his operative gown.
Additionally, we retrospectively reviewed the most recent 100 patients that underwent pedicle screw fixation prior to our use of image guidance. These patient charts and operative notes were reviewed for reoperation rates due to misplaced pedicle screws.
Cost analysis of misplaced pedicle screws was based on the hospital costs of reoperations and surgeon reimbursement. Operating room charges were itemized by the hospital’s billing department and included lab work, drapes and supplies (gowns, gloves, disposable items, prep kits), spinal monitoring, employees, pharmacy, anesthesia, radiographs, recovery room, and hospital stay. Furthermore, the cost of time spent in the operating room for the placement of pedicle screws was analyzed.
RESULTS
There was total of 446 pedicle screws inserted into 100 patients. The demographics of the patients were 15 cases of scoliosis, 36 cases of spondylolisthesis, and 21 cases of revision surgery. The location of pedicle screw placement was 12 thoracic, 352 lumbar, and 82 sacral screws.
Of 446 pedicle screws, intraoperative electromyographic stimulation of the screws revealed no significant nerve stimulation. Additionally, we reviewed patient charts with an average follow-up of 18 months (12 to 24 month range) and found that no patient required revision surgery for a misplaced pedicle screw.
Time for image acquisition, registration of instrumentation, and placement of screws is as follows: 2 screws = average 20 min (range 17-23 min), 4 screws = average 29 min (range 24-47 min), 6 screws = average 38 min (range 31-62 min), 8 screws = average 51 min (range 40-59 min).
Types of cases were analyzed for differences in time required for screw insertion. For four screws, normal cases averaged 29 minutes, revision cases averaged 30 minutes, scoliosis cases averaged 31 minutes, and spondylolisthesis cases averaged 28 minutes, (p = 0.667). For six screws, normal cases averaged 38 minutes, revision cases averaged 41 minutes, scoliosis cases averaged 39 minutes, and spondylolisthesis cases averaged 41 minutes, (p = 0.947).
The complications are divided into system failure and user failure. The system failure rate was 1% (1/100). The Arcadis Orbic 3D would not allow image acquisition. The machine was shut down and re-booted without success. After wasting 25 minutes with the Arcadis Orbic 3D system, the six pedicle screws were inserted under fluoroscopic technique in 42 minutes. Two days later, the Arcadis Orbic 3D worked without complication. The source of error remains unknown.
The user error rate requiring repeat image acquisition was 3% (3/100). Time spent revising image was 9 minutes average (range 7-11 min). One error was due to the radiology technician entering the wrong side of the patient. Another error was due to the radiology technician moving the Arcadis Orbic machine before the collision check resulting in image off center of spine. The final user error was the surgeon bumping the reference frame requiring repeat image acquisition.
The failed screw insertion rate was 1 screw out of 442 (0.2%). The patient had a screw pathway that was misdirected lateral to the vertebral body from a previous surgery done by a different surgeon. Attempt to revise the pathway medially was unsuccessful.
Radiation dosage of the badge worn by the operating surgeon was 18MREM for the entire study group of 100 cases, average 0.18MREM per case. The radiation dose to the patient is 100 images per spin, approximately 40 seconds of fluoroscopy. Every patient received one spin of the Arcadis Orbic 3D, except as described below. Three out of the four cases with eight pedicle screws required two spins in order to capture the vertebral bodies, while one case all four vertebral bodies were captured on one image. Three patients required an additional spin because of user errors as previously described.
Retrospective review of the most recent 100 pedicle screw cases prior to the use of image guidance revealed three cases with misplaced pedicle screws (3%). All screws were placed with the use of fluoroscopy and manual feel. The three symptomatic misplaced screws that breached the medial wall of the pedicle were removed during revision surgery. One screw was redirected into the pedicle. Postoperatively, duration of hospital stay was one day for one patient, two days for one patient, and three days for one patient. Chi-square analysis of the incidence of revision surgery with image guidance (0%) and without image guidance (3%) revealed a p-value of 0.081.
Cost of the revision surgeries was based on costs to the surgery department of the hospital, inpatient fees, and surgeon reimbursement. The average cost of a two hour spinal surgery was $15,915, which includes time in the operating room, lab, drapes, supplies, neuro monitoring, pharmacy, and employees. One hour in the recovery room cost $1,100. Two days hospital stay cost $3,600. The total cost to the hospital was $20,615. Including the average surgeon reimbursement of $3,147, makes the total cost of revision surgery $23,762.
Cost of time for placement of pedicle screws was based on the cost of usage of the operating room. The estimated cost of operating room usage is $5,580 per hour, which equals $93 per minute.
The approximate costs of the navigation systems are $225,000 for the NaviVision (Vector Vision-BrainLAB) and $250,000 for the Arcadis Orbic-Siemens.
DISCUSSION
The accuracy and safety of pedicle screw insertion has been documented with and without the assistance of image guidance. Without image guidance, misplaced screw rates have been reported to be 10-42% [3-14]. While most misplaced screws are not clinically detrimental, they can cause nerve damage, instrumentation failure, and pseudoarthrosis.
Guven et al. reported a 10% misplaced screw rate on thoracolumbar screws inserted under fluoroscopic control. Three percent of the screws were misplaced medially and one patient (2%) experienced neurologic deficit [6]. Odgers et al. reported a misplaced thoracolumbar pedicle screw rate of 11% inserted with lateral plain radiograph. Neurologic complications occurred with two screws [10].
Castro et al. reported on the accuracy of pedicle screw placement in the lumbar spine under fluoroscopic control in both patient and cadaveric groups [3]. The cadaveric study showed 24% of the screws were misplaced medially. In the patient group, 40% of the screws were misplaced. Five out of thirty patients (17%) experienced neurologic deficit, all of these screws were placed 6mm or more medial to the pedicle. All five of these patients required revision surgery.
Percutaneous pedicle screw placement may have an accuracy advantage over open manual palpation techniques because of the increased use of bi-planar fluoroscopy. However, Weisner et al. still showed a 6.6% misplaced screw rate even with percutaneous screw placement [21].
In relation to image guidance systems, Foley et al. has demonstrated that at the thoracolumbar junction the maximum permissible translational error is less than 1mm [22]. However, he also has stated that “in general, mean fiducial errors of less than 1.5mm are considered adequate for most spinal procedures” [23]. In summary, pedicle screws inserted within 2mm of the medial wall of the pedicle have never been reported to cause neurologic injury [5, 7, 24], however, image guidance systems would ideally have accuracy requirements of 1mm or less.
Foley et al. reported on six thoracolumbar cadaveric spines tested with pedicle screw insertion under image guidance. Out of 96 screws, they found no evidence of unintended pedicle wall perforation [15].
Comparison of the accuracy of image guidance versus image intensifier was performed by Laine et al. [17]. They showed a misplaced thoracolumbar pedicle screw rate of 13% for image intensifier versus 5% for image guidance. Of note, the image guidance system tested was an earlier model that relied on preoperative CT scan. Our study tested an intraoperative three-dimensional imager which may be more accurate because the image is acquired with the patient in position on the operating room table, not in a preoperative CT scanner.
Another recent study by Bostelmann et al. showed no complications and no revisions with image guidance placement of pedicle screws in 109 patients [25]. However, there was a 5-12% unsuccessful application of the navigation system. This compares to our findings of only 1% system failure rate. The reason this study had a higher failure rate is most likely due to the reliance on a preoperative CT and requirement for surface matching. The NaviVison system does not require surface matching.
Recently, Kosmopoulos et al. performed a meta-analysis on the accuracy of navigation in the placement of pedicle screws [26]. The median placement accuracy for the in vivo assisted navigation subgroup (95%) was higher than that of the subgroup without the use of navigation (90%).
Image guidance insertion of pedicle screws can be especially helpful in revision surgery. Lim et al. showed 96% accuracy with lumbar pedicle screws inserted into previously fused spines under image guidance [18]. Austin, et al. showed that image guidance had no pedicle wall violations in a simulated fusion cadaver model versus 8% misplaced screws with fluoroscopic assistance [27]. Furthermore, Merloz et al. demonstrated greater accuracy in the placement of pedicle screws with image guidance than manual insertion in cases of fractures, spondylolisthesis, and pseudoarthtrosis [9].
Our study did not show a statistically significant difference in the amount of time required for insertion of pedicle screws in spondylolisthesis, scoliosis, or revision cases. We did not have a large enough sample size to prove this, but the average times are relatively the same.
One the main concerns over the use of navigation is the time required. Kim et al. found similar times in the placement of pedicle screws with and without navigation [28]. In their clinical series, the use of FluoroNav (which is multiple two-dimensional images) required an average setup time of 18 minutes. The average time for screw insertion was 10 minutes per screw.
Our study, which utilizes three-dimensional images, shows an average time for image acquisition, tool registration, and screw placement of 20 minutes for 2 screws, 29 minutes for 4 screws, 38 minutes for 6 screws, and 51 min for 8 screws. Cost savings for the time required for placement of pedicle screws with image guidance can be estimated by subtracting the time required with currently used techniques without image guidance from the above averages, then multiplying by $93 per minute.
Using hospital charges and physician reimbursement rates to estimate the cost of revision surgery has been performed by previous studies [29-31]. Our study showed that the average cost of revision surgery for a misplaced pedicle screw was $23,762. In our practice, we saved $71,286 in the first hundred cases of using the navigation system. In order to estimate annual cost savings for an institution, multiply the amount of cases requiring revision placement of pedicle screws in the past year by $23,762.
Another potential benefit of NaviVision is that the surgeons stand behind a radiographic barrier away from the patient while the images are obtained. The radiation exposure is presumably less than most traditional fluoroscopy techniques in which the surgeon stands near the fluoroscopy machine as it acquires images [32]. Kim et al. found a decrease in radiation exposure to the patient and the surgical team with navigation-assisted fluoroscopy versus standard fluoroscopy [28]. Gebhard et al. also showed a decrease in radiation exposure to the surgical team with the use of navigation [33]. Our study reveals a negligible amount of radiation exposure to the surgeon of 0.18 MREM per case.
LIMITATIONS OF STUDY
- Ideally, postoperative CT scans would be obtained on all study group patients to assess pedicle screw accuracy. However, we did not find it necessary to subject an asymptomatic patient to additional radiation.
- The accuracy of the image guidance system is based on electromyographic stimulation of the screws and reoperation rates for screw revision. The accuracy of electromyographic stimulation of pedicle screws has not been proven scientifically.
- Despite the rate of revision surgery being 0% with and 3% without the use of image guidance, the p-value was 0.081, which is not statistically significant. An increase in the number of cases would add power to our study.
CONCLUSION
- The rate of revision surgery was reduced from 3% to 0% with the use of image guidance.
- The cost savings of image guidance for the placement of pedicle screws was $71,286 per 100 cases.
- Time required for pedicle screw placement with image guidance was 20 minutes for 2 screws, 29 minutes for 4 screws, 38 minutes for 6 screws, and 50 min for 8 screws.
- Cost savings for the time required for placement of pedicle screws with image guidance can be estimated by subtracting the time required with currently used techniques without image guidance from the above averages, then multiplying by $93 per minute.
- Image guidance for the placement of pedicle screws may be cost effective in spine practices with heavy volume, that perform surgery in difficult cases, and that require long surgical times for the placement of pedicle screws.
CONFLICT OF INTEREST
Dr. Robert Watkins, IV, is a paid educational consultant for BrainLAB and Siemens. Research funding was contributed by Siemens for the collection and synthesis of the data for this study.