All published articles of this journal are available on ScienceDirect.
Functional Outcomes After Anatomic and Reverse Shoulder Arthroplasty Assessed using a Novel Objective Method
Abstract
Introduction
Anatomic shoulder arthroplasty replicates joint anatomy, while Reverse Total Shoulder Arthroplasty (RSA) is preferred for rotator cuff deficiency or bone loss. This study compares pre- and post-operative function after TSA and RSA using outcome measures and the Kinesiological Instrument for Normal and Altered Reaching Movement (KINARM).
Methods
A cohort of 81 shoulders in 74 patients (mean age 71 ± 8) underwent Total Shoulder Arthroplasty (TSA) or Reverse Total Shoulder Arthroplasty (RSA). Outcomes included lateral and forward elevation; WOOS, Constant, Oxford, and SF-36 scores; and Kinarm sensorimotor tasks (visually guided reaching, object hit, arm position matching). Patients were evaluated pre-operatively and at 6 weeks, 3, 6, and 12 months. Analyses used paired and independent t-tests, ANOVA, and Pearson correlation.
Results
ROM improved at 3, 6, and 12 months in TSA and at 6 and 12 months in RSA (p < 0.01), with TSA showing better ROM at 3 months (p < 0.01). Both groups showed improvement in WOOS, Oxford, and Constant scores (p < 0.01). The TSA group had higher SF-36 mental scores, while the RSA had higher physical scores beyond 3 months. TSA showed better early WOOS, Oxford, and Constant scores. Kinarm tasks improved at 1 year in both groups (p < 0.01), and RSA showed greater improvement in arm matching. Kinarm scores correlated strongly with WOOS, Constant, and Oxford.
Discussion
Early recovery favored TSA; by 12 months, outcomes converged. Kinarm offers an objective complement to PROMs.
Conclusion
TSA and RSA showed similar 1-year outcomes, with earlier recovery after TSA. Kinarm is a reliable objective tool for pre- and post-operative upper extremity assessment.
Level of Evidence: Level II.
1. INTRODUCTION
The goal of shoulder replacement surgery is to improve pain and shoulder function in patients with shoulder arthritis, whether or not they have a rotator cuff deficiency. Shoulder arthritis, both with and without rotator cuff deficiency, is a complex condition that seriously compromises the comfort and function of the shoulder. The primary indication for shoulder arthroplasty is a painful shoulder caused by glenohumeral arthritis that has failed nonsurgical management [1]. On the other hand, the presence of rotator cuff arthropathy often results in significant pain and loss of shoulder motion [2].
While pain relief and increased range of motion can be obtained in shoulders with arthritis and an intact rotator cuff with an anatomical shoulder arthroplasty, a Reverse Total Shoulder Arthroplasty (RSA) is more suited to shoulders with a deficient rotator cuff or severe bone loss [3-6]. In addition to providing pain relief and improving shoulder motion, each type of arthroplasty has been shown to enhance functional outcomes using traditional subjective functional outcome scores [5, 7]. Flurin et al. found that Total Shoulder Arthroplasty (TSA) performs better than RSA in functional outcome scores, especially Constant and American Shoulder and Elbow Surgeons (ASES) scores, and better in Range of Motion (ROM) pre- and post-operative over 30 months follow-up [8]. Simovitch et al. evaluated 1641 shoulders retrospectively and found that the functional outcome is 30% larger in RSA compared with TSA in the first 12 months post-operative [9]. Kiet et al. reported no significant difference between TSA and RSA at a two-year follow-up in functional outcome and complication rate [10].
Although several validated questionnaires can be used to assess shoulder function, such as the WOOS, Oxford shoulder score, Constant score, and 36-Item Short-Form Health Survey (SF-36) questionnaire, there is no widely adopted objective tool to compare the outcome of shoulder arthroplasty. Interactive robotic technologies offer an objective method for assessing arm function. In particular, the Kinarm Exoskeleton Lab uses interactive robots and an integrated virtual reality system, along with standardized behavioral tasks to quantify upper limb sensory and motor function (Fig. 1A); Kinarm, Kingston, Ontario, Canada). Kinarm has been used previously to assess the upper extremity sensory and motor function in stroke [11-14]. Therefore, this study was designed with two objectives. First, to compare the functional outcomes after anatomic and reverse shoulder arthroplasty. Second, to determine the usefulness of the Kinarm as a reliable tool to objectively measure shoulder functional improvement in subjects receiving a shoulder arthroplasty.
2. MATERIALS AND METHODS
This was a prospective study of patients with glenohumeral arthritis who had failed nonoperative treatment and underwent shoulder replacement surgery. After obtaining informed consent, patients were assigned to receive either anatomic or reverse shoulder arthroplasty based on several factors, including patient age, diagnosis, associated rotator cuff disease and pre-operative function. This study was approved by the Queen’s University and Affiliated Teaching Hospitals Health Sciences Human Research Ethics Board under study number: SURG-206-09. All surgeries were performed by the senior author, a fellowship-trained shoulder surgeon.
Patient evaluation included shoulder range of motion, incorporating forward elevation and lateral elevation. Patients also completed several Patient-Reported Outcome Measures (PROMs), including the WOOS, the Oxford Shoulder Score, the Constant Score, and the SF-36 questionnaire [15-19]. All PROMs were evaluated pre-operatively and at 6 weeks, 3 months, 6 months and 1 year post-operatively.
Kinarm assessments were performed pre-operatively and at 1-year post-operatively at Kingston Health Sciences Centre (Kingston, ON, Canada). Individuals sat in an adjustable-height chair, and their arms were supported by troughs connected to robotic linkages. The linkages were adjusted such that the participant’s shoulder and elbow joints were aligned with the joints of the robotic linkage. Shoulder and elbow angles and hand position were calculated from encoders within the torque motors attached to the mechanical linkage. The system permitted arm movement in the horizontal plane with the shoulder positioned at approximately 85 degrees of abduction. A virtual reality system using a television and a reflective mirror displayed spatial goals and feedback of limb position (when required) aligned in the horizontal workspace of the arms (Fig. 1A). Direct vision of the arms was occluded by a physical barrier, and peripheral vision of the arms was removed using a bib connected between the virtual reality stand and around the participant’s neck. (For a video of the basic setup for the Kinarm Exoskeleton Lab, see https://kinarm.com/solutions/exoskeleton-lab/).
Each patient performed three Kinarm Standard Tests (KST) in 15 minutes, including training and instruction [13].
2.1. Visually-guided Reaching (VGR) (Figure 1B) [11]
Individuals were instructed to maintain the fingertip (represented by a small white circle) to a central target (red 1cm diameter circle). After ~1 second, a peripheral target appeared, and the participant was (previously instructed) to move toward quickly and accurately to the peripheral target. When the individuals reached the peripheral target, the central target was re-illuminated, and they then returned to the central target. The task included four peripheral targets in different spatial directions (10 cm reach) and six repeated trials for each target.
2.2. Object Hitting Task (OH) (Figure 1C) [14]
Virtual paddles appear at the subject’s fingertips, and virtual balls move toward them in the workspace. Individuals are instructed to use the virtual paddles to hit the balls away from their bodies. As the task progresses, the balls move at greater speeds and appear more frequently, making the task more difficult as time progresses. Haptic feedback (a small force pulse) is provided when contact is made between the paddle and ball to provide haptic feedback. The task initially included 300 balls located in 10 virtual bins across the top of the screen.
2.3. Arm Position Matching (APM) Task (Fig. 1D) [12]
This task assesses arm proprioceptive function. During this task, the Kinarm robot attached the operative arm to one of four spatial locations, and the participant was instructed to move their other arm to the mirror-image position. The test was repeated six times for each target.
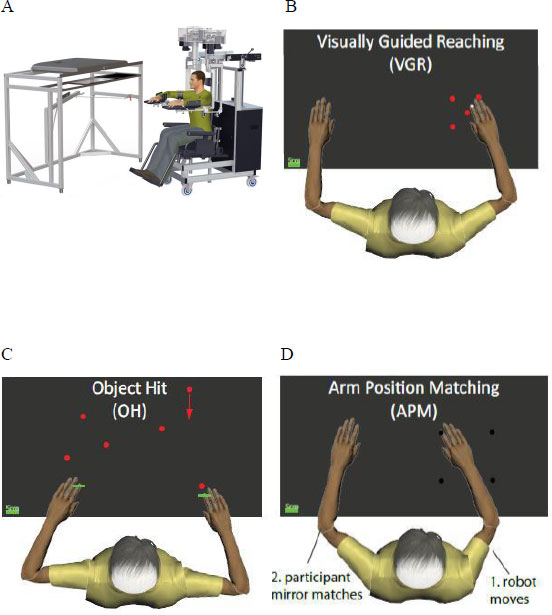
Kinarm robotic system and task paradigms used for objective assessment of upper limb function. (A) Overhead view of participant seated in the Kinarm Exoskeleton Lab. (B) Visually Guided Reaching (VGR): Participants reach from a central target to peripheral targets using real-time visual feedback. (C) Object Hit (OH): Participants use virtual paddles to strike moving balls appearing at increasing frequency and speed across the screen. (D) Arm Position Matching (APM): The robot moves one arm to a position, and the participant mirrors the movement with the opposite arm.
Several spatial and temporal features were used to characterize performance on each of the Kinarm tasks [11-14]. KST also calculates a Task Score that quantifies an individual’s performance relative to a large cohort of healthy controls, such that scores near 0 reflect the best performance and 1.96 represents the 95th percentile for healthy individuals [13].
Sample size was calculated using a previous Kinarm visually guided reaching task study [11]. With a mean difference of 7 degrees between affected and unaffected arms and standard deviations of 6 and 13 degrees, 30 patients are required in each of the two arthroplasty groups. To allow for a 20% loss to follow-up, we targeted 36 patients in each group. Comparisons were made within and across implant groups. Statistical analyses employed paired and independent samples t-tests, as well as one-way Analysis of Variance (ANOVAs). As there is no gold standard tool to compare the Kinarm measure with, Pearson’s correlation coefficient was used to correlate the pre- and post-operative Kinarm scores with each of the WOOS, Oxford, Constant, and SF-36 measures to assess reliability.
3. RESULTS
This study included 81 shoulders in 74 patients, with 13 patients lost to follow-up, 31 of whom received a TSA and 37 received an RSA (Fig. 2). The RSA group matched the age of the TSA group but contained significantly more females Table 1. Evaluation of shoulder range of motion included forward elevation and lateral elevation. Comparing each group with baseline findings (pre-op), the TSA group showed a significantly better range of motion at 3, 6 and 12 months post-operatively, whereas the RSA group showed significant improvement at 6 and 12 months post-operatively Tables 2 and 3. The TSA group had a better forward elevation at 6 weeks and 3 months and better lateral elevation at 3 months post-operatively compared with RSA. However, no significant difference was observed between the two groups after these points Tables 2 and 3.
Evaluation of functional outcome scores revealed that the WOOS and Oxford scores showed significant improvements from baseline to 6 weeks, 3, 6 and 12 months in both groups (p < 0.05). The Constant score showed better outcome in both groups at 3, 6 and 12 months post-operatively Tables 3 and 4. The SF-36 showed improvements in physical scores in RSA, but not in mental scores in TSA Table 4 and 5. When comparing the functional outcome measures of both groups, the TSA group showed better WOOS scores at 6 weeks and 3 months compared to the RSA group, but no differences were observed at 6 months and 1 year Table 6. The Constant score was better at 3 months in the TSA group, but there were no differences at other time points. The TSA group had higher Constant and Oxford scores at baseline and 6 weeks post-operatively Table 6, but there were no differences at other time points.
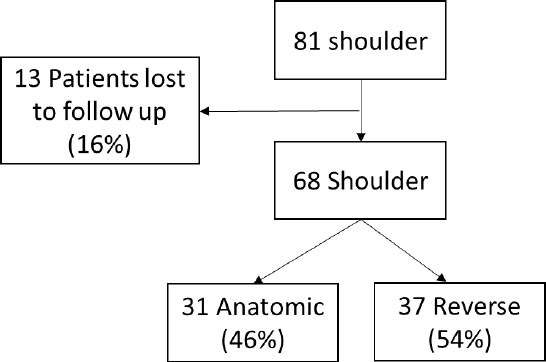
Flowchart of patient enrollment and group allocation. A total of 81 shoulders were enrolled in the study. 13 shoulders (16%) were lost to follow-up, leaving 68 shoulders for analysis. Of these, 31 received an anatomic Total Shoulder Arthroplasty (TSA; 46%) and 37 received a Reverse Total Shoulder Arthroplasty (RSA; 54%).
| Characteristic | Anatomic (n = 31) | Reverse (n = 37) | P-value |
|---|---|---|---|
| Age (SD) | 69.90 (9.19) | 73.57 (6.66) | 0.06 |
| Sex F:M | 10:21 | 26:11 | 0.002 |
| Timepoint |
Forward elevation Mean (SD) |
P-value |
Lateral elevation Mean (SD) |
P-value |
P-value (Comparison between groups) |
|---|---|---|---|---|---|
| Pre-op | 89.9 (27.6) | - | 75.8 (29.7) | - | 0.18 |
| 6 weeks | 88.5 (23.8) | 0.82 | 82.0 (21.9) | 0.34 | 0.002 |
| 3 months | 102.8 (20.4) | 0.04 | 96.5 (20.7) | 0.007 | 0.001 |
| 6months | 115.0 (13.1) | 0.001 | 108.7 (16.2) | < 0.001 | 0.084 |
| 1 year | 113.7 (15.1) | 0.001 | 113.5 (18.4) | < 0.001 | 0.66 |
| Timepoint |
Lateral elevation Mean (SD) |
P-value |
Forward elevation Mean (SD) |
P-value |
P-value (Comparison between groups) |
|---|---|---|---|---|---|
| Pre-op | 78.4 (33.3) | - | 69.9 (25.9) | - | 0.80 |
| 6 weeks | 66.7 (28.7) | 0.09 | 69.7 (31.1) | 0.97 | 0.08 |
| 3 months | 82.8 (23.0) | 0.71 | 81.6 (22.8) | 0.35 | 0.009 |
| 6months | 106.0 (23.7) | 0.001 | 100.9 (24.2) | < 0.001 | 0.15 |
| 1 year | 115.8 (21.0) | <0.001 | 108.2 (21.4) | < 0.001 | 0.28 |
| Timepoint |
WOOS Mean (SD) |
P-value |
Oxford Mean (SD) |
P-value |
Constant Mean (SD) |
P-value |
SF36 Physical Mean (SD) |
P-value |
SF36 Mental Mean (SD) |
P-value |
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | 1193.6 (344.9) | - | 24.0 (7.7) | - | 43.7 (16.8) | - | 39.2 (9.5) | - | 45.9 (15.3) | - |
| 6 weeks | 617.3 (243.3) | < 0.001 | 31.8 (8.3) | < 0.001 | 44.4 (15.5) | 0.84 | 42.7 (8.6) | 0.28 | 47.8 (13.8) | 0.003 |
| 3 months | 380.1 (329.7) | < 0.001 | 36.3 (7.6) | < 0.001 | 56.1 (12.3) | 0.002 | 45.8 (10.1) | 0.19 | 47.8 (12.9) | < 0.001 |
| 6 months | 353.7 (410.3) | < 0.001 | 39.5 (10.1) | < 0.001 | 65.7 (12.0) | < 0.001 | 49.1 (11.5) | 0.49 | 43.6 (13.5) | < 0.001 |
| 1 year | 324.7 (391.6) | < 0.001 | 41.4 (7.3) | < 0.001 | 68.3 (12.2) | < 0.001 | 49.7 (11.5) | 0.18 | 40.7 (14.1) | < 0.001 |
| Timepoint |
WOOS Mean (SD) |
P-value |
Oxford Mean (SD) |
P-value |
Constant Mean (SD) |
P-value |
SF36 Physical Mean (SD) |
P-value |
SF36 Mental Mean (SD) |
P-value |
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | 1316.4 (224.7) | - | 19.2 (7.6) | - | 32.4 (14.7) | - | 37.2 (9.4) | - | 39.2 (16.3) | - |
| 6 weeks | 849.4 (348.7) | < 0.001 | 23.9 (9.3) | 0.005 | 31.8 (14.6) | 0.84 | 40.1 (8.1) | 0.05 | 41.2 (14.2) | 0.41 |
| 3 months | 616.4 (360.8) | < 0.001 | 33.0 (9.2) | < 0.001 | 45.1 (16.6) | < 0.001 | 44.3 (9.7) | < 0.001 | 41.7 (15.7) | 0.37 |
| 6 months | 370.9 (331.0) | < 0.001 | 37.5 (8.4) | < 0.001 | 59.0 (14.2) | < 0.001 | 46.1 (9.9) | < 0.001 | 41.1 (15.3) | 0.30 |
| 1 year | 364.8 (355.7) | < 0.001 | 40.6 (5.5) | < 0.001 | 61.8 (17.1) | < 0.001 | 46.8 (10.7) | < 0.001 | 33.5 (12.1) | 0.08 |
| Timepoint |
WOOS Anatomic/reverse |
P-value |
Oxford Anatomic/reverse |
P-value |
Constant Anatomic/reverse |
P-value | SF36 physical Anatomic/reverse | P-value |
SF36 mental Anatomic/reverse |
P-value |
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | 1251.5/1315.9 | 0.41 | 23.59/19.2 | 0.02 | 43.9/32.9 | 0.006 | 38.6/37.2 | 0.53 | 43.9/38.8 | 0.20 |
| 6 weeks | 616.8/849.4 | 0.003 | 31.8/23.1 | <0.001 | 44.4/31.8 | 0.002 | 42.5/39.9 | 0.22 | 47.8/41.2 | 0.06 |
| 3 months | 383.8/616.4 | 0.01 | 36.3/32.0 | 0.06 | 56.1/45.1 | 0.004 | 45.5/44.3 | 0.64 | 47.7/41.7 | 0.12 |
| 6 months | 373.1/370.9 | 0.98 | 39.1/37.1 | 0.41 | 65.7/59.0 | 0.05 | 48.7/46.1 | 0.34 | 43.2/41.1 | 0.57 |
| 1 year | 334.3/376.2 | 0.65 | 40.5/39.7 | 0.69 | 68.3/61.8 | 0.09 | 49.4/46.9 | 0.38 | 40.6/33.6 | 0.04 |
| Timepoint |
Object Hit Anatomic/Reverse |
P-value Anatomic/Reverse |
*P-value |
Arm matching Anatomic/reverse |
P-value Anatomic/Reverse |
*P-value |
Visually guided reaching Anatomic/reverse |
P-value Anatomic/Reverse |
*P-value |
|---|---|---|---|---|---|---|---|---|---|
| Pre op | 2.29/2.62 | - | 0.41 | 1.33/1.36 | - | 0.86 | 3.36/4.06 | - | 0.30 |
| 1 year post op | 1.54/1.50 | 0.012/0.001 | 0.88 | 1.29/0.97 | 0.80/0.013 | 0.05 | 1.78/2.19 | 0.003/< 0.001 | 0.17 |
| A. Anatomic shoulder replacement | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WOOS | Oxford | Constant | SF-36 physical | SF-36 mental | ||||||||||
| Kinarm Pre-op | 0.30* | P = 0.01 | 0.63* | P < 0.01 | 0.80* | P < 0.01 | 0.32 | P = 0.17 | 0.25 | P = 0.13 | ||||
| Kinarm Post-op | 0.52* | P < 0.01 | 0.35 | P = 0.03 | 0.61* | P < 0.01 | 0.54* | P < 0.01 | 0.17 | P = 0.14 | ||||
| B. Reverse shoulder replacement | ||||||||||||||
| Kinarm Pre-op | 0.40* | P < 0.01 | 0.60* | P < 0.01 | 0.55* | P < 0.01 | 0.42* | P < 0.01 | 0.07 | P = 0.14 | ||||
| Kinarm Post-op | 0.66* | P < 0.01 | 0.55* | P < 0.01 | 0.58* | P < 0.01 | 0.20 | P = 0.22 | 0.18 | P = 0.21 | ||||
The evaluation of objective functional outcomes using the Kinarm revealed that pre-operative performance in the visually guided reaching and object-hitting tasks was quite high (poor score) (Fig. 3A). A majority of individuals were identified as impaired in reaching and object-hitting tasks Table 7. A few individuals were identified as impaired pre-operatively in the arm matching task, which assessed proprioceptive function, and even fewer were identified at the one-year follow-up Table 7. In general, both surgical groups showed a significant improvement in object hit and visually guided reaching tasks with no significant difference between groups. In contrast, in arm matching tasks, the RSA group performed better than the TSA group (p-value = 0.05) (Fig. 3B, Table 7.
Pearson’s correlation coefficient showed that the pre- and post-operative Kinarm Task Scores were moderately to highly correlated with Constant, Oxford scores, and WOOS scores Table 8. The pre- and post-operative SF-36 scores showed a weak to moderate correlation with Kinarm scores Table 8.
4. DISCUSSION
This study found that the TSA group scored significantly better on several pre-operative measures compared to the RSA group. This is expected as the selection criteria for patients undergoing RSA included associated rotator cuff disease and poor pre-operative function. Another important finding was the significant improvement in all functional scores in both groups post-operatively compared with the pre-operative functional scores. The TSA group had better function in the early post-operative period, but there was no significant difference in functional scores between the two groups at 6 months and 1 year post-op. These results align with those observed in previous studies, which suggested a significant improvement in functional outcomes both before and after surgery, with no difference between the two groups over time [20, 21]. This is expected as the TSA group had better pre-operative function and would therefore be expected to have better function early post-operatively, whereas the RSA group took longer to regain function post-operatively.
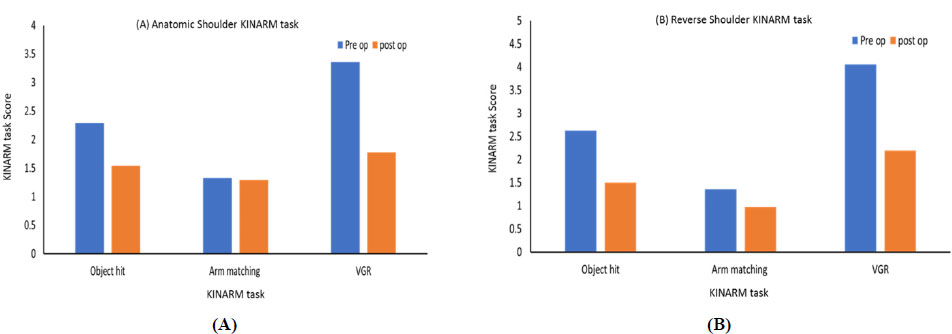
Pre- and post-operative Kinarm task performance in patients undergoing shoulder arthroplasty. (A) Anatomic Total Shoulder Arthroplasty (TSA) group and (B) Reverse Shoulder Arthroplasty (RSA) group performance on three KINARM tasks: Object Hit (OH), Arm Position Matching (APM), and Visually Guided Reaching (VGR). Task Scores decreased post-operatively in both groups, indicating improved motor and sensory function. RSA patients demonstrated greater improvement in Arm Position Matching compared to TSA. Bars represent mean Task Scores. X-axis: KINARM task (Object Hit, Arm Position Matching, VGR). Y-axis: KINARM Task Score (z-score; lower = better, 0 = control mean, 1.96 = 95th percentile).
This study found a statistically significant moderate to strong correlation between the Kinarm score and the Constant score pre- and post-operatively. A moderate correlation was found between Oxford scores pre- and post-operatively, as well as with WOOS pre- and post-operatively. However, Kinarm scores showed a low to moderate correlation with the SF-36, which is similar to a previous study that found a poor correlation between the SF-36 and shoulder-specific measures [20]. Therefore, Kinarm can be considered a good, reliable, and objective tool to assess pre- and post-operative improvement in shoulder function after shoulder arthroplasty. Thus, Kinarm may provide an objective measurement tool to assess shoulder function and may be an important addition to current functional outcome measures.
In addition, we found a significant post-operative improvement in the Kinarm limb matching task, which measures proprioception function in the RSA group. However, no significant change was found in the TSA group. This finding suggests that shoulder arthroplasty does not impair proprioceptive function and may provide some improvement, particularly as observed with the RSA group. Therefore, RSA may provide an improvement in proprioceptive function that is not observed after TSA. As mentioned earlier, the Kinarm findings were reinforced by the PROMs, which showed significant post-operative improvements compared with pre-operative scores. However, these measurements are subjective and depend mainly on the patient’s cooperation and memory, which can be prone to response fatigue. Thus, the Kinarm measurements are objective tools and can overcome this issue. Therefore, Kinarm may provide an objective measurement tool for shoulder function after shoulder arthroplasty.
One strength of this study was the standardization of procedures, as all shoulder replacements were performed by the same fellowship-trained shoulder surgeon. The Kinarm strengths include its ability to eliminate human subjectivity in quantifying the nature and severity of dysfunction. It also allows precision by quantifying subtle but measurable limb dysfunction. Although the status of the patient’s pre-operative shoulder condition prevented us from randomizing them to the implant intervention, the study was prospective, which limited the biases inherent in retrospective studies. One limitation of using the Kinarm is its inability to assess the full shoulder range of motion, as the patient requires both arms and forearms to be attached to the Kinarm exoskeleton linkages. However, this limitation was minimized in this research by the ability of the participant to move their shoulder through flexion/extension in the horizontal plane, as well as abduction/adduction around 85 degrees. The ROM findings were also in accord with the Kinarm and PROM results, showing improvements over time and no differences between the implant groups at one year.
5. STUDY LIMITATIONS
This study involved a moderate sample size and non-randomized patient allocation, which may limit the generalizability of the findings. Kinarm assessments, although objective, do not capture the full three-dimensional motion of the shoulder. Additionally, outcomes were limited to one year post-operatively.
CONCLUSION
There was an overall improvement in functional outcome scores after both anatomic and reverse shoulder arthroplasty. Patients undergoing TSA have a better range of motion and function pre-operatively and in the early post-operative period compared to patients undergoing RSA. However, both TSA and RSA have a similar range of motion and function at 6 months and 1 year post-operatively. Kinarm is a novel research tool that may be useful to objectively assess functional outcomes after shoulder arthroplasty. Therefore, this tool may have applications to pre- and post-operative objective evaluation of shoulder function. We anticipate that this will primarily be used in objective measurement in research studies, rather than routine post-operative evaluation.
LIST OF ABBREVIATIONS
| TSA | = Total Shoulder Arthroplasty |
| RSA | = Reverse Shoulder Arthroplasty |
| KINARM | = Kinesiological Instrument for Normal and Altered Reaching Movement |
| WOOS | = Western Ontario Osteoarthritis of the Shoulder Index |
| PROMs | = Patient-Reported Outcome Measures |
| SF-36 | = 36-Item Short-Form Health Survey |
| ROM | = Range of Motion |
| ANOVA | = Analysis of Variance |
| ASES | = American Shoulder and Elbow Surgeons (score) |
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: R.B., R.S., D.P., S.H.S: Study Conception and Design; E.A., S.A.Q.: Analysis and interpretation of results. All authors reviewed the results and approved the final version of the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Queen’s University and Affiliated Teaching Hospitals Health Sciences Human Research Ethics Board under study number: SURG-206-09.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants prior to inclusion in the study.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
ACKNOWLEDGEMENTS
The authors wish to acknowledge Heather Grant for their assistance with data analyses and Kim Moore for assistance in data collection.


