All published articles of this journal are available on ScienceDirect.
Intra-articular Corticosteroid Injection for Adhesive Capsulitis: A Randomized Controlled Trial
Abstract
Background
Adhesive capsulitis is a common cause of glenohumeral joint pain and stiffness that significantly interferes with patients' lives and ability to work. Since no specific treatment options have been well established, this research examines arthrographic injection of the glenohumeral joint with steroid and local anesthetic versus local anesthetic alone for the treatment of adhesive capsulitis.
Methods
A double-blinded randomized controlled trial was conducted with patients diagnosed with idiopathic adhesive capsulitis. They were randomized to one of two groups: (1)local anesthetic plus steroid or (2)local anesthetic. A musculoskeletal radiologist performed all of the image-guided injections using a standardized patient-blinded technique. Outcome measures included shoulder range of motion, grip strength, and scores on the Shoulder Pain and Disability Index (SPADI), Constant Score, and Visual Analog Scale (VAS) for pain. Evaluations occurred at baseline and 3-, 6- and 12-weeks post-injection.
Results
Thirty-seven patients were enrolled in the study. There was no significant improvement in shoulder range of motion and grip strength with local anesthetic plus corticosteroid injection compared to local anesthetic alone. Shoulder range of motion was better at all time points for the group with local anesthetic alone. Both groups showed significant improvements in their VAS and SPADI pain scores at all post-injection follow-up appointments (p=.011). The SPADI results showed significantly better disability scores for the local anesthetic plus steroid group (p=.012) and improved pain scores from baseline at all follow-up times (p=.011), whereas the local anesthetic group had significant pain relief for only the first 3 weeks (p=.050).
Conclusion
Intra-articular injection with local anesthetic plus steroid was beneficial in improving pain but not range of motion when compared to injection with local anesthetic alone.
1. INTRODUCTION
Adhesive capsulitis, or frozen shoulder, is a common cause of glenohumeral joint pain and stiffness that is estimated to affect 2–5% of the general population and up to 20% of patients with diabetes mellitus [1-5]. The American Shoulder and Elbow Surgeons (ASES) define frozen shoulder as “a condition characterized by functional restriction of both active and passive shoulder motion for which radiographs of the glenohumeral joint are essentially unremarkable except for the possible presence of osteopenia or calcific tendonitis [6]. The primary frozen shoulder describes the condition with no known identifiable etiology, and the secondary frozen shoulder applies when an intrinsic or extrinsic cause is determined. The condition has three described stages: freezing, frozen, or thawing, based on clinical findings. [7-10] It progresses from a painful, inflammatory state to one of stiffness due to capsular fibrosis, with the whole process taking up to two years and, in some cases, even longer. [3, 11] Frozen shoulder is most commonly seen in the non-dominant arm of middle-aged women and tends to be associated with endocrinopathies such as diabetes mellitus and thyroid dysfunction. [2, 7] Additionally, smokers and patients with cardiovascular disease or those who have had a cerebrovascular accident are at increased risk of developing this disease. [6, 12-14]
The frozen shoulder was initially thought to be a self-limiting condition with a favourable natural history, with some stating that the resolution would be within 2 years without any specific treatment. [1, 15-17], More current studies, however, have demonstrated that many patients continue to experience unacceptable dysfunction that interferes with their work and lifestyle for over 3 years from symptom onset. [4, 11, 16],
The treatment options for frozen shoulder are vast, and despite this, no specific protocols have been well established or accepted. [7, 18-20] Conservative treatment with physiotherapy, Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), and intra-articular corticosteroid injections are often recommended initially, with surgical intervention in the form of arthroscopic or open lysis of adhesions reserved for refractory cases. [3, 5] Although commonly prescribed and thought to be beneficial for short-term symptomatic relief, the efficacy of intra-articular local anesthetic plus corticosteroid injection over local anesthetic alone has not been well established in this patient population. [21].
Several randomized controlled trials comparing interventions for adhesive capsulitis have looked at intra-articular corticosteroid injection compared to placebo [15, 22, 23], intra-articular versus subacromial corticosteroid injection [24], and corticosteroid injection versus placebo with or without supervised physiotherapy. [19] Intra-articular corticosteroid was shown to significantly improve pain and disability at 6- and 12-week regardless of physiotherapy intervention, and the difference between treatment groups became smaller with time out to one year. [19] To our knowledge, no studies have examined the difference between intra-articular local anesthetics with and without corticosteroid for the treatment of adhesive capsulitis.
We hypothesize that arthrographic injection of the glenohumeral joint with local anesthetic with corticosteroid is an effective treatment for adhesive capsulitis and is superior to injection with local anesthetic alone.
2. MATERIALS AND METHODS
This was a double-blinded, Randomized Controlled Trial (RCT) NCT02001740 of patients with a diagnosis of idiopathic adhesive capsulitis who were recruited from one orthopedic surgeon’s practice over a one-year period. All study participants were blinded to their treatment group. The surgeon who conducted the follow-up visit data collection was also blinded to group allocation as randomization and participant tracking were performed by the participating research nurse, and the musculoskeletal radiologist administered injections. Ethics approval was granted by the institution’s research ethics board. The inclusion criteria were patients between 18-70 years of age with a diagnosis of primary idiopathic adhesive capsulitis who had symptoms for a minimum of 3 months. The exclusion criteria included patients who developed adhesive capsulitis secondary to trauma, had previous surgery on the affected shoulder, and had radiographic evidence of glenohumeral joint osteoarthritis or rotator cuff arthropathy.
Once informed consent for the study was obtained, data was collected, including patient demographics and risk factors, and group allocation was assigned using computer randomization to receive one image-guided arthrography glenohumeral joint injection with either a mix of 40mg of triamcinolone (corticosteroid), 5cc of 1% lidocaine (local anesthetic) and 0.5-1cc of contrast or a mix of 5cc of 1% lidocaine and 0.5-1cc of contrast alone. A fellowship-trained musculoskeletal radiologist performed all of the image-guided arthrographic glenohumeral injections using the same patient-blinded technique. The accuracy of injections was confirmed by a flow of contrast within the glenohumeral joint on fluoroscopy.
Outcome measures included active and passive shoulder Range Of Motion (ROM) comparing the affected shoulder to the contralateral shoulder. The movements tested abduction, forward flexion, and internal and external rotation at 900 of shoulder abduction, and measurements were made with a goniometer. Grip strength as a measure of pain was recorded using the average calculated from three measurements for each hand with a digital hand dynamometer to establish a more accurate result. A previous study on adhesive capsulitis showed that patients clinically demonstrated pain with static effort at the shoulder and grip strength was shown to be a reliable measure of pain as strength should increase with decreasing pain. [25] Functional outcomes were assessed using the Shoulder Pain and Disability Index (SPADI), the Constant Score, and a Visual Analog Scale (VAS) for pain. [26, 27] Evaluations occurred at baseline and 3-, 6- and 12- weeks post-injection. Additionally, all patients in both treatment arms were prescribed outpatient physiotherapy for shoulder range of motion after the injection. All patients started with the same baseline assessment by the clinic physiotherapist, who demonstrated shoulder range of motion exercises and provided exercise sheets with instructions for use at home. Outpatient physiotherapy was not standardized; patients may have attended different physiotherapy clinics, and the number of sessions depended on the individual’s health coverage.
Statistical analysis included descriptive statistics in the form of counts, percentages, means, and standard deviations to summarize demographic and other study variables. Parametric and non-parametric tests were used to compare variables between and within groups over time. Specific tests include chi-square, paired and independent samples t-test, and a one-way ANOVA with post-hoc Bonferroni correction. An alpha value of < .05 was considered statistically significant.
The sample size was calculated similarly to an RCT conducted by Buchbinder et al. [22], which used the SPADI score at 3 weeks as the primary outcome measure. We determined that 49 patients in each treatment group would be needed to detect a difference in mean SPADI scores of 13 [28] with 80% power.
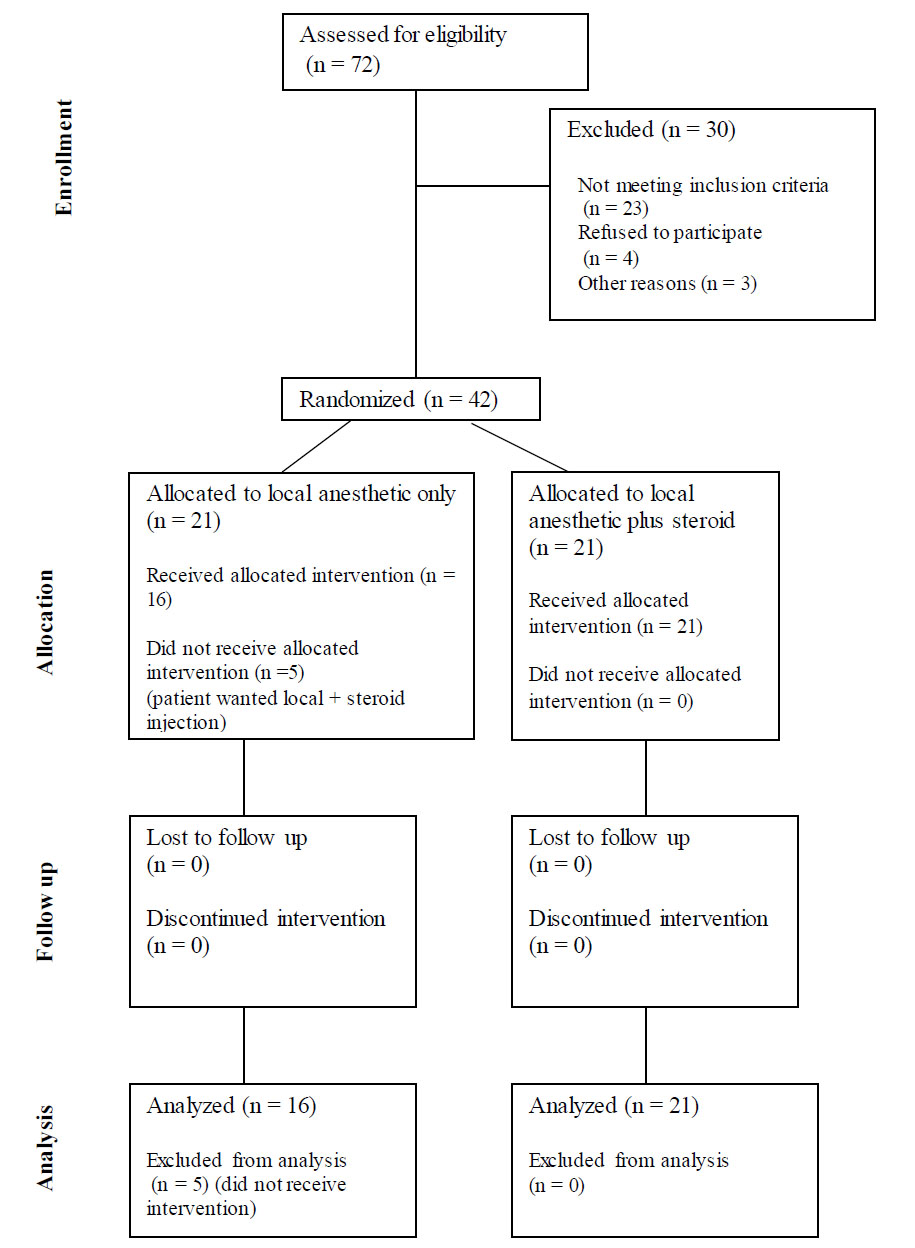
CONSORT flow diagram.
3. RESULTS
There were 37 patients aged 42 to 67 years old included in this study (Table 1 and Fig. 1). Twenty-three patients were female, and 14 were male. Sixteen patients were randomized to the local anesthetic-only group – 10 females and 6 males with an average age of 51 (range of 42-57). Twenty-one patients were randomized to the local anesthetic plus corticosteroid group – 13 females and 8 males with an average age of 55 (range of 42-67). There were 22 right shoulders and 15 left shoulders, with 30 right-hand dominant participants and 7 left-hand dominant. Twenty-seven percent (n=10) of the cohort had a diagnosis of diabetes, 30% (n=11) smoked cigarettes, 8% (n=3) had a history of cardiovascular disease, 5% (n=2) had rheumatoid arthritis, and one patient had hypothyroidism. There were no significant differences between the number of comorbidities between groups. Furthermore, we did not identify differences in any outcomes with respect to comorbidities.
Compared to their baseline VAS pain score, both the local anesthetic only and local anesthetic plus corticosteroid groups showed significant improvements at their 3-, 6- and 12-week post-injection follow-up appointments (p=0.011). The VAS pain scores showed no significant differences between the two groups at any of the time points (Table 2).
Grip strength scores showed no significant differences over time in either the local anesthetic (p=.47) or local anesthetic plus corticosteroid group (p=.60). There were statistically significant differences between the groups’ baseline scores (p=.023) but not at any of the subsequent follow-up appointments (Table 3).
Constant scores showed no statistically significant differences between the local anesthetic group compared to the local anesthetic plus corticosteroid group at baseline (p=.92), 3 weeks (p=.39), 6 weeks (p=.86), and 12 weeks (p=.36). The SPADI results showed significantly better disability scores for the local anesthetic plus corticosteroid group (p=.012), and significantly better pain scores from baseline for both groups (p=.011). Pain scores improved from baseline in all follow-up time points for the local anesthetic plus corticosteroid group (p=.014). The local anesthetic group experienced pain relief for only the first 3 weeks (p=.050).
| Characteristic | No. of Shoulders (n=37) |
|---|---|
| Age | 51 (42-67) |
| Sex: male/female | 14/23 |
| Side: right/left | 22/15 |
| Dominance: right/left | 30/7 |
| Co-morbidities (%) | - |
| Diabetes | 27 |
| Smoked cigarettes | 30 |
| Cardiovascular disease | 8 |
| Rheumatoid arthritis | 5 |
| Hypothyroidism | 3 |
| - | Baseline | 3 Weeks | 6 Weeks | 12 Weeks |
|---|---|---|---|---|
|
Local Anesthetic Mean (SD) |
6.9 (1.7) | 2.9 (2.1) | 3.4 (2.5) | 2.5 (2.0) |
|
Local Anesthetic plus Corticosteroid Mean (SD) |
7.9 (1.6) | 2.2 (2.7) | 4.0 (3.0) | 3.1 (2.7) |
| p-value | .11 | .45 | .59 | .50 |
| - | Baseline | 3 Weeks | 6 Weeks | 12 Weeks |
|---|---|---|---|---|
|
Local Anesthetic Mean (SD) |
10.8 (6.8) | 13.9 (5.1) | 12.6 (5.1) | 13.4 (5.3) |
|
Local Anesthetic plus Corticosteroid Mean (SD) |
15.8 (5.9) | 18.6 (22.5) | 13.8 (5.2) | 14.5 (6.7) |
| p-value | .023 | .31 | .70 | .72 |
| Range of Motion | Study Group | Baseline Mean (SD) Degrees [p-value] |
3 Weeks Mean (SD) Degrees [p-value] |
6 Weeks Mean (SD) Degrees [p-value] |
12 Weeks Mean (SD) Degrees [p-value] |
|---|---|---|---|---|---|
| FF Active | local | 108(24) | 126(17) | 139(28) | 135(18) |
| - | local + steroid | 96(23) | 110(20) | 114(30) | 117(23) |
| - | - | [.39] | [.34] | [.16] | [.18] |
| FF Passive | local | 113(23) | 131(20) | 143(26) | 138(21) |
| - | local + steroid | 103(23) | 113(21) | 120(27) | 124(23) |
| - | - | [.49] | [.33] | [.52] | [.27] |
| LE Active | local | 91(31) | 105(34) | 117(36) | 109(26) |
| - | local + steroid | 83(21) | 108(24) | 110(32) | 100(22) |
| - | - | [.33] | [.82] | [.56] | [.36] |
| LE Passive | local | 95(31) | 111(36) | 122(37) | 111(26) |
| - | local + steroid | 87(21) | 111(25) | 117(28) | 104(23) |
| - | - | [.41] | [.96] | [.69] | [.46] |
| IR Abduction Active | local | 33(28) | 21(14) | 50(30) | 24(29) |
| - | local + steroid | 33(27) | 14(18) | 31(20) | 26(18) |
| - | - | [.95] | [.37] | [.07] | [.86] |
| IR Abduction Passive | local | 37(31) | 22(14) | 55(33) | 29(31) |
| - | local + steroid | 38(30) | 17(20) | 35(21) | 29(21) |
| - | - | [.95] | [.48] | [.08] | [.98] |
| ER Abduction Active ActiveAcActive | local | 41(33) | 58(31) | 68(25) | 63(27) |
| - | local + steroid | 43(29) | 60(25) | 63(23) | 62(22) |
| - | - | [.87] | [.82] | [.58] | [.88] |
| ER Abduction Passive | local | 44(35) | 62(35) | 74(27) | 65(28) |
| - | local + steroid | 49(31) | 64(28) | 71(21) | 64(23) |
| - | - | [.71] | [.83] | [.74] | [.93] |
Passive and active shoulder ROM is demonstrated in Table 4. The local anesthetic group had significantly better active and passive shoulder forward flexion at all follow-up times compared to the local anesthetic plus corticosteroid group. The local anesthetic group showed statistically better forward flexion, both actively and passively, at 6 weeks compared to baseline (p=.031, p=.010). For the local anesthetic plus corticosteroid group, the forward flexion measurements were highest and statistically significant compared to baseline at the 12-week mark for both active and passive measurements (p=.050, p=.032).
4. DISCUSSION
Arthrographic injections with local anesthetic or local anesthetic plus a corticosteroid are safe treatment options for patients with adhesive capsulitis. Shoulder injections with local anesthetic plus corticosteroid showed no advantage over injection with local anesthetic alone in terms of improving range of motion. However, there was more sustained pain control in the local anesthetic plus corticosteroid group compared to local anesthetic alone.
The optimal treatment regimen for adhesive capsulitis remains unclear. According to one review paper by Griesser et al. in 2011, all treatment options for this condition resulted in improved clinical outcomes as measured by the Constant, SPADI, and VAS pain scores [8]. Interestingly, an intra-articular injection with corticosteroid was found to be superior in the short-term when compared to the other treatment modalities, including physiotherapy, manipulation under anesthetic, hydraulic joint distention, and oral steroids [11, 21, 24]. Carette et al. found similar results that patients treated with intra-articular corticosteroid injection had improved pain and function scores compared to those treated with a saline injection alone or in combination with supervised physiotherapy [19]. Patients in their study who received a combination of an intra-articular corticosteroid injection and a supervised physiotherapy program had the most improvement in their range of motion. They also found that corticosteroid injections produced more short-term improvement in pain and range of motion when compared to physiotherapeutic intervention alone. Our study showed significantly better SPADI disability scores for the local anesthetic plus steroid injection group (p=.012), and improved pain scores from baseline at all follow-up times (p=.011) when compared to the injection of local anesthetic alone.
An RCT by Rizk et al. [23] investigating the effect of corticosteroid injections in adhesive capsulitis showed that the injection of lidocaine with steroids had no advantage over lidocaine alone in terms of shoulder range of motion, but there was some transient pain relief noted in two-thirds of the patients treated with lidocaine with steroid. Their study randomized 48 patients to one of 4 treatment groups (i.e., intra-articular lidocaine plus steroid, intrabursal lidocaine plus steroid, intra-articular lidocaine, and intrabursal lidocaine) with the same physical therapy program for all patients and found no significant difference in outcome between intrabursal and intra-articular injection. Our study complements this RCT by confirming their findings with a larger sample size from one surgeon’s practice over a year period.
Our cohort experienced a few minor, temporary complications, and all participants reported that they tolerated the procedure well. Our findings are consistent with the literature as arthrographic injection using corticosteroid is considered a relatively benign and inexpensive procedure with few inherent risks to the patient [11].
The study design is one strength of this research. We used a double-blinded prospective randomized controlled design and saw a 92% follow-up at the 12-week injection appointment. All patients were recruited from the same surgeon’s practice and thus had the same evaluations, recommendations, and offered treatment options. All of the image-guided intra-articular injections were performed by the same musculoskeletal radiologist using their standard technique.
There were several limitations to this study. The small sample size is a weakness of this study, as we were unable to stratify the results due to the limited number of patients diagnosed with adhesive capsulitis over our study period. As with other RCTs comparing interventions for adhesive capsulitis, slower patient recruitment than expected was an issue, and the study was stopped early and, as a result, may be underpowered. The follow-up time of 12 weeks is relatively short and was chosen to be able to examine the effect of the injection, while other similar RCTs showed an effect of 12 weeks with decreasing difference to the comparative intervention after that. [22] Also, outpatient physiotherapy was not standardized for this study due to limitations in available resources and patient factors, and this was a major limitation. Finally, our patient population had several comorbidities. However, given the small sample size, we were not able to identify any differences in outcomes between comorbidities.
CONCLUSION
Arthrographic injection with local anesthetic plus steroid was beneficial in improving pain but not range of motion when compared to injection with local anesthetic alone. Patients in both groups demonstrated improve- ments in their VAS and SPADI pain scores from baseline, but only patients in the local anesthetic plus corticosteroid group improved their SPADI disability scores and had improvements in their SPADI pain scores past the 3-week follow-up visit. As a result, we recommend intra-articular injection with local anesthetic plus corticosteroid as a safe treatment option that is superior to local anesthetic alone for longer-term pain control in the treatment of adhesive capsulitis.
DISCLAIMER
This study was supported by a Grant from the Physicians’ Services Incorporated Foundation.
The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
AUTHORS’ CONTRIBUTION
R.B.: Contributed to the study’s concept and design; P.F. and A.T.: Collected data; C.H. Analyzed the data and interpreted the results; J.C.: Drafted the manuscript.
LIST OF ABBREVIATIONS
| NSAIDs | = Nonsteroidal Anti-Inflammatory Drugs |
| RCT | = Randomized Controlled Trial |
| ROM | = Range of Motion |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Queen’s University Health Sciences, Canada and Affiliated Teaching Hospitals Research Ethics Board (SURG-246-12) reviewed and approved the ethics for this study.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.


