All published articles of this journal are available on ScienceDirect.
Comparison of Perioperative Pain Management between Arthroscopic Rotator Cuff Repair and Total Knee and Hip Arthroplasty, A Retrospective Study
Abstract
Background
Although postoperative shoulder pain surgery is severe, the quality of its management has not been studied in comparison with pain after other orthopedic surgeries. Furthermore, reports have investigated daytime pain, but none have discussed nighttime pain.
Objective
This study aimed to compare perioperative pain management in patients who underwent Arthroscopic Rotator Cuff Repair (ARCR) and those who underwent lower extremity arthroplasty.
Methods
The study population included 33 patients who underwent ARCR and 21 patients who underwent lower-extremity arthroplasty between August 2015 and March 2016. For postoperative analgesia, an interscalene brachial plexus block was used for ARCR, and an epidural block was used for lower extremity arthroplasty. The Visual Analog Scale (VAS) for rest and night pain was measured from the day before the operation to the fourth postoperative day.
Results
In ARCR, night pain was significantly weaker on the day of surgery (VAS, ARCR 23.9 vs. lower extremity arthroplasty 47.9; P = 0.008); however, it was significantly stronger on the second and third postoperative days (2nd, 45.6 vs. 23.2; P = 0.002 / 3rd, 38.1 vs. 23.5; P = 0.021). There were no significant differences in rest pain.
Conclusion
It was confirmed that postoperative pain can be well managed in patients undergoing ARCR. However, because the pain worsened after the removal of the block, further improvement is required.
1. INTRODUCTION
Pain is a common complication of surgery, and it has been reported that perioperative pain in orthopedic surgery is stronger than that in other departments [1]. Perioperative pain is known to lead to chronic pain, and orthopedic surgery has been reported to be a risk factor for chronic pain [2]. Severe prolonged pain interferes with rehabilitation [3, 4], which may be disadvantageous for functional improvement and may significantly impair patients’ quality of life [5]. Although a painless postoperative state is ideal, the side effects of using high doses of oral and intravenous painkillers have been problematic [6]. To reduce side effects, there has been a shift from systemic to local analgesics. Depending on the site of surgery, an epidural block is often used in combination with knee and hip pain management, and its usefulness has been reported in many cases [7-10]. Although perioperative pain management is also crucial for patients with shoulder disorders, postoperative pain in shoulder surgery is reported to be severe, and as in other operations, its management is a serious problem [11, 12].
In recent years, arthroscopy has been used more frequently in shoulder surgery to reduce surgical invasion. Although arthroscopy is less invasive than open surgery [13], some reports suggest that the postoperative pain is equivalent to that after open surgery [14-16]. It has been reported that rotator cuff repair is more painful than other arthroscopic shoulder procedures [11, 17]. The interscalene brachial plexus block has been used to alleviate perioperative pain in shoulder surgeries, and it has been reported to be effective for local anesthesia in shoulder surgery [18, 19].
Perioperative pain management in shoulder surgery has not yet been established. Therefore, it is necessary to investigate whether perioperative pain management by inter scalene brachial plexus block is effective in shoulder surgery. In contrast, perioperative pain management for Total Knee Arthroplasty (TKA) and Total Hip Arthroplasty (THA) by epidural block has been relatively well established [20].
To the best of our knowledge, no report has compared perioperative pain management with orthopedic surgeries. In addition, although there have been many reports comparing pain during the day, none have investigated and compared night pain. We believe that it is useful to investigate night pain in patients with shoulder disease because of the high incidence of sleep disorders. This study aimed to compare perioperative pain management between arthroscopic rotator cuff repair (ARCR) and lower extremity arthroplasty.
2. MATERIALS AND METHODS
This retrospective observational study was conducted using the opt-out method on the hospital website. All procedures were performed in compliance with the relevant regulations and guidelines. This research has been approved by the Institutional Review Board of the authors’ affiliated institutions.
This 6-day observational study included 37 patients who underwent ARCR and 23 patients who underwent lower extremity arthroplasty (TKA, n=5; THA, n=18) between August 2015 and March 2016 at our hospital. Patients who underwent ARCR and lower extremity arthroplasty were classified into Groups ARCR and TKA/THA, respectively. The inclusion criteria were as follows: patients who (1) received either ARCR for rotator cuff tear or TKA/THA for knee or hip OA; (2) received an interscalene brachial plexus block for ARCR or epidural block for TKA/THA as perioperative anesthesia; and (3) underwent surgery that was started in the morning (the investigation period for night pain included the day of the surgery and the time at which the operation ended was thought to affect the outcome). The exclusion criteria were as follows: (1) revision surgery for the shoulder, hip, or knee; (2) bilateral surgery on the same day or week; and (3) treatment for or history of psychiatric or neurological disorders.
2.1. Anesthesia and Analgesia
Nerve block and general anesthesia were performed by anesthesiologists. All surgeries were performed under general anesthesia using propofol, sevoflurane, remifen- tanil, air, and oxygen. Nerve blocks were used for intraoperative and postoperative analgesia. The use of non-narcotic drugs for analgesic rescue was approved.
2.1.1. Interscalene Brachial Plexus Block
The patients received no premedication or sedation prior to the nerve block procedure. Ultrasound-guided interscalene brachial plexus block was performed by placing a 6–15 MHz linear phased-array transducer (HFL50x/15-6, FUJIFILM SonoSite, Inc., Tokyo, Japan) equipped with a Sonosite S-Nerve (FUJIFILM SonoSite, Inc.). A 50-mm, 18-gauge needle (Stimuplex D, B. Braun, Melsungen, Germany) was then placed into the interscalene groove using the lateral-to-medial in-plane technique. The patient initially received a single injection of 20 ml of 0.25% ropivacaine at C5/6 between the anterior and middle scalene muscles. Subsequently, a catheter was inserted through the needle into the same area, 10 ml of the same solution was injected once again, and a cold test was conducted to confirm the effect of the block. General anesthesia was then administered, and adequate positioning of the catheter was confirmed after surgery. After confirming the catheter position, the patient received a single injection of 0.25% levobupivacaine (10 ml) through the catheter. The catheter was then connected to a disposable infuser (COOPDECH Balloon- jector, Daiken Medical, Osaka, Japan) containing a mixture of 200 ml of 0.25% levobupivacaine and 100 ml of saline, which was administered continuously at 6 ml/h.
2.1.2. Epidural Block
The patients received no premedication or sedation prior to the epidural block procedure. An 80 mm, 18-gauge needle and standard catheter (Portex epidural system, Smith Medical, Saint Paul, MN, USA) were used. The catheter was inserted at L2/3 for THA and at L3/4 for TKA. The epidural block was performed with the patient in the left lateral and knee-chest position. The epidural space was confirmed using the loss-of-resistance technique with saline. Subsequently, 1% mepivacaine (4 mL) was administered through the catheter as the test dose. After confirming that the movement of the lower limbs was unaffected, general anesthesia was administered. During the surgery, 0.25% levobupivacaine (6-10 ml) was administered through the catheter. Postoperatively, the catheter was connected to a disposable infuser (COOPDECH Balloonjector, Daiken Medical, Osaka, Japan) containing a mixture of 200 ml of 0.25% levobupivacaine and 100 ml of saline, which was administered continuously at 4 ml/h.
2.2. Surgical Procedure
2.2.1. ARCR
The surgery was performed by a sufficiently experienced shoulder surgeon. All operations were performed with the patient in the beach chair position using an arm positioner.
A posterior portal was first established for the initial assessment of the glenohumeral joint. The arthroscope was removed from the glenohumeral joint and redirected into the subacromial space. The size, location, and delamination of the tears were carefully assessed during the initial assessment. As much bursal tissue as possible was removed, and arthroscopic subacromial decom- pression was performed. The footprint was exposed by removing the remnant of the rotator cuff and bone abrasion using an arthroscopic shaver. The suture bridge method was applied using suture anchors after footprint preparation of the rotator cuff for reattachment. Eventually, a total of 5-7 portals were created.
All patients underwent supraspinatus and infra- spinatus tendon repair, with additional treatment for subscapularis tendon tears and long head of biceps tendon tears, depending on the case. All patients used a sling with an abduction pillow after surgery.
2.2.2. TKA
Surgery was performed by one of two sufficiently experienced knee surgeons. All operations were performed with the patient in the supine position using a tourniquet placed just before the skin incision and after the closure of the skin. Standard medial parapatellar arthrotomy was performed after an anterior midline skin incision. Osteotomy was performed using an intra- medullary guide and cutting block guide for the femur and an extramedullary guide for the tibia. All prostheses were fixed with cement. A suction drain was placed intra-articularly before closing the articular capsule and removed on the second postoperative day.
2.2.3. THA
Surgery was performed by one of two sufficiently experienced hip surgeons. All surgeries were performed with the patient in the lateral decubitus position using a posterior approach. A skin incision of approximately 10 cm was made, the fascia was incised over the gluteus maximus muscle, and the muscle was bluntly divided down to short external rotators. The short external rotators were tenotomized from the greater trochanter, and the exposed articular capsule was incised to reach the joint. Osteotomy of the femoral head and acetabular preparation were performed, and implants were placed without cement. Following reconstruction, the capsule and short external rotators were repaired to the greater trochanter or directly repaired to the gluteus medius tendon. A suction drain was placed in the submuscular space before closing the fascia and removed on the second postoperative day. Postoperatively, a hip abduction pillow was used in bed.
2.3. Postoperative Therapy and Block Removal
Postoperative rehabilitation was performed using the same protocol in all cases for each surgery. A shoulder sling was used after ARCR, and mild passive range-of-motion (ROM) exercise, trunk and shoulder girdle function training, and isometric cuff exercises were started on the first postoperative day.
For postoperative therapy for TKA, the patient was kept in bed on the first postoperative day. To initiate oral administration of edoxaban for the prevention of deep venous thrombosis, a suction drain was removed on the morning of the second postoperative day. Subsequently, the patient began to walk and perform ROM exercises as long as they were able to tolerate the pain.
A hip abduction pillow was used in bed after THA. On the first postoperative day, the patient rested in bed. Suction drains were removed in all cases on the morning of the second postoperative day. The patients then began to walk within their pain tolerance. All blocks were removed on the morning of the second postoperative day.
2.4. Outcome Measures
The survey items included age, sex, duration of surgery, rest pain, and night pain. Pain at rest was defined as pain experienced without movement during the day. Night pain was defined as pain that occurred without movement from night to the following morning. The visual analog scale (VAS) was used to measure pain, with 0 mm defined as no pain and 100 mm as the maximum possible pain. The VAS was investigated for six days, from the day before surgery to the fourth postoperative day. In addition, the size of the rotator cuff tear was confirmed intraoperatively.
The primary outcome was the group difference in the VAS of night pain on the day of surgery because the pain was generally most intense on the day of surgery, especially at night when patients tended to complain of an increased degree of pain. As a secondary outcome, we compared the VAS scores for rest and night pain between the two groups after the removal of blocks to evaluate the appropriateness of the timing of block removal for early postoperative analgesia.
2.5. Statistical Analysis
The pre and intraoperative parameters were compared between the two groups using Fisher's exact probability test for categorical variables and an unpaired t-test for continuous variables. The VAS values for rest and night pain were compared between the two groups using an unpaired t-test. Statistical analyses were performed using IBM SPSS Statistics version 25 (IBM Corp., Armonk, NY, USA). Statistical significance was set at P < 0.05.
3. RESULTS
3.1. Demographics
The present study included 33 patients who underwent ARCR and 21 who underwent TKA (n=5) or THA (n=16). Four patients who underwent ARCR were excluded due to a history of psychiatric disorders. Two patients who underwent THA were excluded because they had undergone revision surgery.
Demographic data are demonstrated in Table 1. The general anesthesia and operation times of the two groups did not differ significantly; however, there was a significant difference in sex. The cuff tear size, defined according to the report of Cofield et al. [21], was classified as small, medium, large, or massive in 2, 13, 16, or 2 cases, respectively.
Additional procedures for ARCR included subscapularis tendon repair (n=9), long head of biceps (LHB) tenotomy (n=6), and LHB tenodesis (n=6).
NSAIDS, acetaminophen, and tramadol hydrochloride/ acetaminophen combination tablets were administered for rescue analgesia. Intravenous analgesics were not administered.
3.2. Perioperative Pain Comparison
The rest pain in the two groups did not differ significantly on any of the days (Fig. 1). The night pain on the day of surgery was significantly more severe in Group TKA/THA (P=0.03). However, on the second and third postoperative days, it was significantly stronger in Group ARCR (Fig. 2).
4. DISCUSSION
The most important result obtained in this study was that ARCR significantly reduced nighttime pain on the day of surgery. In this study, we compared perioperative pain associated with ARCR and TKA/THA using a block as local anesthesia to evaluate perioperative pain management in shoulder surgery. To the best of our knowledge, this is the first study to compare the perioperative pain management of ARCR with that of other orthopedic surgeries.
Conversely, night pain in group ARCR was significantly more severe on the second and third postoperative days. In this case, all blocks were removed on the morning of the second postoperative day, which was one of the affecting factors.
| - | ARCR (n=33) | TKA (n=5) / THA (n=16) | P-value |
|---|---|---|---|
| Sex (M/F) | 21/12 | 2/19 | < 0.001 |
| Age (years) | 64.5 | 65.7 | 0.726 |
| Anesthetic time (min) | 244.6 | 252.9 | 0.553 |
| Surgical time (min) | 173.3 | 178.6 | 0.690 |
Abbreviations: ARCR, arthroscopic rotator cuff repair; TKA, total knee arthroplasty; THA, total hip arthroplasty.
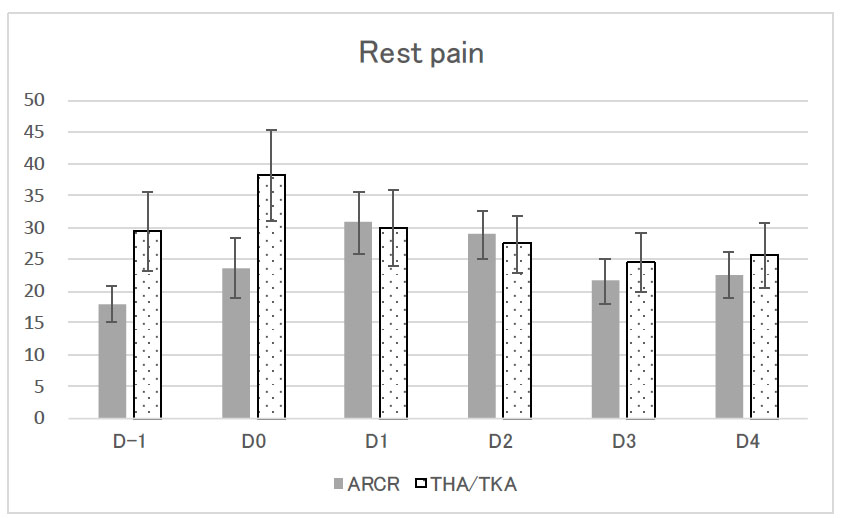
Perioperative rest pain measured by the VAS.
Abbreviations: VAS; visual analog scale; ARCR; arthroscopic rotator cuff repair; TKA, total knee arthroplasty; THA, total hip arthroplasty.
D-1: One day before surgery; D0, The day of surgery; D1, postoperative day 1; D2, postoperative day 2; D3, postoperative day 3; and D4, postoperative day 4.
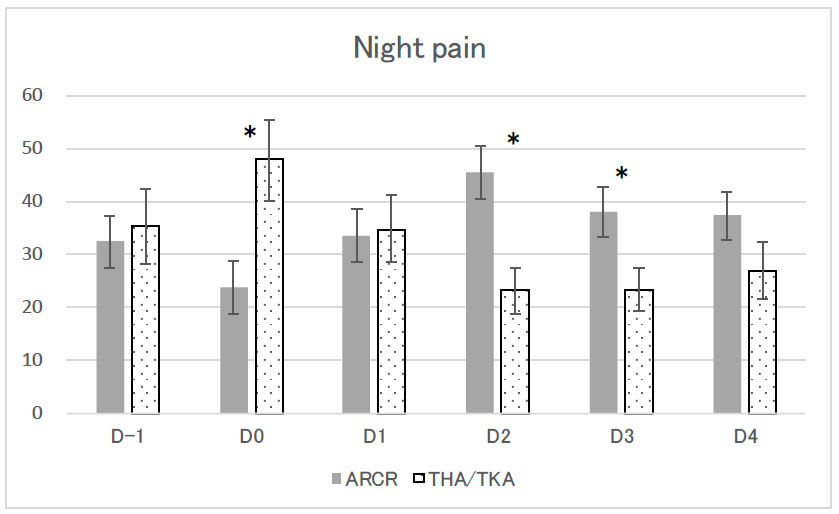
Perioperative night pain measured by the VAS.
Abbreviations: VAS; visual analog scale; ARCR; arthroscopic rotator cuff repair; TKA, total knee arthroplasty; THA, total hip arthroplasty.
D-1: One day before surgery; D0, The day of surgery; D1, postoperative day 1; D2, postoperative day 2; D3, postoperative day 3; and D4, postoperative day 4.
*Indicates a statistically significant difference between two groups (p < 0.05).
4.1. Perioperative Pain at Night
Shoulder surgery is associated with severe post-operative pain. Ghandour et al. reported that on the day of ARCR, without special treatment, the postoperative pain was reported to be 70/100 (VAS) [12]. Cho et al. reported that the postoperative pain one day after arthroscopic acromioplasty and mini-open rotator cuff repair under management with IV-PCA (fentanyl [15 μg/kg], ketorolac [2 mg/kg], and ondansetron [8 mg]) [22] was 5.9/10 on the Numeric Rating Scale (NRS), suggesting that some form of pain management is essential.
The concomitant use of an interscalene brachial plexus block has been reported to improve postoperative pain management in shoulder surgery. Fredrickson et al. reviewed the postoperative pain in shoulder surgery. Subacromial (bursal)/intra-articular infiltration analgesia, suprascapular and/or axillary (circumflex) nerve block, single-injection ('single-shot') interscalene brachial plexus block, and continuous interscalene brachial plexus block were described. Although there were technical problems, they stated that a continuous interscalene brachial plexus block was the most effective treatment [15].
Shin et al. reported a 48 hour postoperative NRS score of approximately 2/10 when ARCR was combined with continuous interscalene brachial plexus block [23], suggesting that the block may have a positive effect on analgesia.
Conversely, regarding postoperative pain in patients undergoing lower extremity arthroplasty with an epidural block, Campbell et al. reported a mean VAS of 30/100 at 24 hours after TKA [24], and Vanterpool et al. reported an NRS of 4.3/10 on day 1 and 3.5/10 on day 2 after TKA/THA [25]. In the present study, the rest pain on the first postoperative day was 38/100 (VAS), suggesting that pain management for TKA/THA was acceptable.
In this study, in addition to resting pain, we evaluated perioperative pain at night. There was no significant difference in daytime rest pain between the two groups; however, nighttime pain on the day of surgery was significantly reduced in the ARCR group. While there have been reports of an association between shoulder joint disease and sleep disorders [26, 27], most previous studies have only investigated daytime pain. When investigating shoulder pain, it is necessary to evaluate not only daytime pain but also nighttime pain. The quality of sleep was not investigated in this study; therefore, it is not possible to discuss the effect of the suppression of night pain immediately after surgery. This should be a subject for future studies.
4.2. Block Removal Timing
Continuous interscalene brachial plexus block is useful for shoulder surgery; however, there is no consensus on the timing of its removal. Salviz et al. reported post- operative pain after ARCR combined with a continuous interscalene brachial plexus block when the block was removed 48 hours after surgery; on postoperative day 2, the severity of pain rated according to an NRS, was as follows: 0-3, 55% of patients; 4-7, 35%; and 8-10, 10%. In contrast, the values on postoperative day 3 were as follows: 0-3, 35%; 4-7, 45%; and 8-10, 20% [28].
There was no uniformity in the timing of epidural block removal. Vanterpool et al. reported that the NRS increased from approximately 3.5/10 on postoperative day 2 to 4.5 on postoperative day 3 when the block was removed at 48 hours [25]. Tsukada et al. used an epidural block for the management of postoperative pain in TKA, and when the epidural block was removed 24 hours after surgery, the VAS was approximately 20/100, but it gradually increased to approximately 35 at 72 hours [29].
When the blocked catheter was removed on the morning of the second day after surgery in this study, there was no significant difference in rest pain; however, night pain was significantly stronger in the ARCR group on the second and third days after surgery. Increased pain after block removal wasreported previously; however, in the present study, by examining night pain and comparing it to that after other orthopedic surgeries, we found that there was a large increase in pain after ARCR.
There is no recommended timing for block removal. However, because of the significant increase in pain after removal on the second postoperative day, prolongation of block usage should be considered depending on the case.
The present study has some limitations. First, pain is subjective and difficult to compare among patients. However, there was no significant difference in the preoperative VAS scores, suggesting that there was no difference in pain sensitivity. Psychological tests may also be necessary due to the influence of psychological factors on pain.
More than one person performed the surgeries. However, there was no significant difference in operative time between the surgeons, and we believe the impact on the surgery was small.
The use of rescue analgesics was not managed with regard to the use of rescue analgesics, which may have affected postoperative pain. However, we did not approve of the use of narcotic drugs. The establishment of a rescue analgesic protocol should be considered; however, there are ethical difficulties associated with the use of medications owing to patient demands.
CONCLUSION
The present study compared postoperative pain management in patients who underwent ARCR with that in patients who underwent total knee and hip arthroplasty. A significant difference was observed for night pain, with a reversal before and after the removal of the block. Further research is needed to improve pain management, such as prolonged use of blocks.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ARCR | = Arthroscopic Rotator Cuff Repair |
| TKA | = Total Knee Arthroplasty |
| THA | = Total Hip Arthroplasty |
| ROM | = Range-of-motion |
| VAS | = Visual Analog Scale |
| LHB | = Long Head Of Biceps |
| NRS | = Numeric Rating Scale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Gunma University Ethical Review Board for Medical Research Involving Human Subjects (20201036) approved this study.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent for participation and publication was obtained from the participants.
(The patients and/or their families were informed that data from the research would be submitted for publication, and their consent was given.)


