All published articles of this journal are available on ScienceDirect.
Kinematic Alignment Technique for TKA on Degenerative Knees with Severe Bone Loss: A Report of 3 Cases
Abstract
A severely degenerative knee joint with substantial bone attrition poses a significant challenge when performing Total Knee Arthroplasty (TKA) using the Kinematic Alignment (KA) technique. In order to restore the pre-arthritic knee anatomy, the surgeon has the task of estimating quantity and location of bone loss. We present three such cases and describe the key steps to safely perform KATKA in these complex situations.
1. INTRODUCTION
Severely degenerative knee joints with substantial bone attrition and remodelling pose a significant challenge when performing Total Knee Arthroplasty (TKA) using the Kinematic Alignment (KA) technique [1, 2]. In order to restore the pre-arthritic knee anatomy, the surgeon has the task of estimating the quantity and location of bone loss.
We are presenting three such cases: one performed with manual instrumentation (calipered KA technique [2]), and two performed with the use of computed navigation [3]. Regardless of the technique selected to perform KA TKA in these cases, the key steps to estimate the quantity and location of bone loss are:
1. Pre-operative planning on radiographs using the healthy or mildly diseased contralateral knee as a guide for determining the constitutional knee anatomy.
2. Intra-operative assessment of the gap of the worn knee compartment by correcting the limb deformity (stress test) before making any cuts. The mean ligament laxity is around 1-2 mm medially and 3-4 mm laterally [4], and the cartilage thicknesses on the femur and tibia are approximately 2 mm [5, 6]. With full cartilage loss, gaps would be expected to be 5 to 6 mm medially (cartilage loss plus physiological ligament laxity). A larger gap suggests the presence of bone loss.
3. Intra-operative joint surface inspection to identify preserved areas of articular surfaces that could serve as references.
4. Assessment of laxity of collateral ligaments with spacer blocks or trial implants to refine bone resections when needed, using the average healthy knee ligament laxity as a target (1-2 mm medially and 3-4 mm laterally).
2. CASE 1
A 72-year-old female rheumatoid patient with a windswept lower limb deformity. Previously, she had undergone a gap-balancing, Mechanically Aligned (MA) left TKA (Fig. 1b). One year later, she requested a right knee replacement. On examination of the right knee, the 20º valgus deformity was fully correctable, the medial collateral ligament had a firm endpoint during the valgus stress-test, and the patella was stable.
2.1. Pre-operative Planning
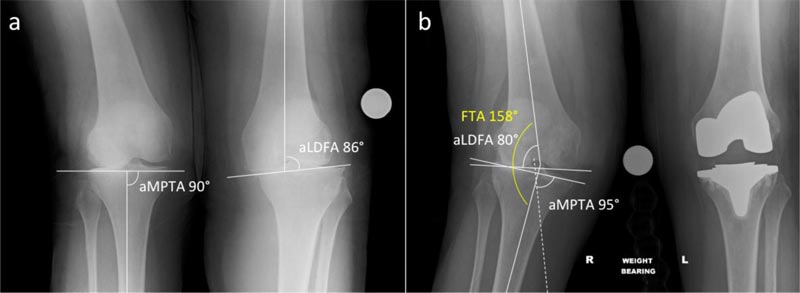
Knee radiographs were used to estimate the pre-arthritic right knee anatomy (Fig. 1). The constitutional (pre-arthritic) Lateral Distal Femoral Angle (aLDFA) was estimated to be 85° (distal femoral joint line 5° valgus) and the Medial Proximal Tibial Angle (aMPTA) was estimated to be 90° (proximal tibial joint line neutral at 0°) (Fig. 1a). Considering we measured 80° and 95° for these respective angles on a subsequent radiograph taken 18 months before performing the right TKA (Fig. 1b), a 5 mm bone loss was suspected from both the lateral femoral condyle and tibial plateau.
2.2. Intra-operative Joint Measurements
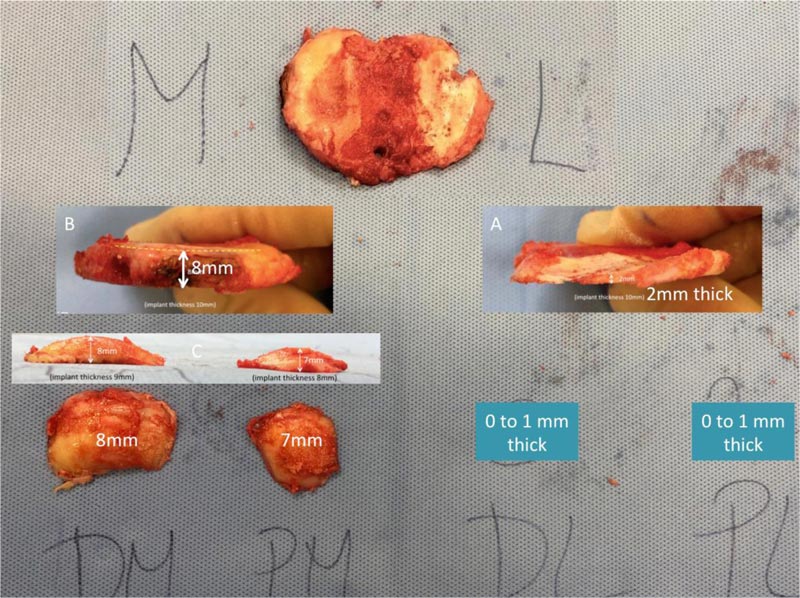
Once the articular surfaces were exposed, the medial compartment integrity was confirmed by assessing the cartilage thickness with a scalpel (Fig. 2). With valgus and varus stresses, the medial and lateral compartment laxities were assessed throughout the knee Range of Motion (ROM). The medial knee compartment had a 3-4 mm laxity, and the lateral knee compartment had approximately 20 mm laxity (use of spacer blocks to measure gaps). Considering the physiological lateral collateral ligament laxity of 3-4 mm, and the 4 mm of cartilage loss (2 mm on femur and tibia), approximately 12 mm of lateral bone loss was estimated (20 mm minus 8 mm). Since there was a similar lateral knee compartment laxity throughout the range of flexion and considering our pre-operative planning, we estimated there was 6 mm of bone loss from the lateral plateau and 6 mm of bone loss from the distal and posterior aspect of the lateral condyle.
2.3. Bone Cuts
The distal and posterior lateral femoral condyle cuts were performed by compensating for 8 mm surface loss (2 mm of cartilage plus 6 mm of bone). The tibial cut was performed with the aim of removing 9 mm medially (tibial component is 10 mm, minus 1 mm to account for a probable 1 mm medial collateral ligament stretching) and 2 mm laterally (tibial component is 10 mm, minus 2 mm of cartilage and 6 mm of bone loss). Caliper measurements confirmed adequate execution of the plan (Fig. 3).

2.4. Collateral Ligaments Laxity Assessment
With the trial components in situ, the knee laxity was re-assessed throughout ROM: the medial and lateral compartments had a 1-2 mm and 2-3 mm laxity throughout knee flexion, respectively, and there was no laxity in full knee extension; there was no residual knee stiffness, and the passive patella tracking was centered without tilt. No ligament release was necessary.
2.5. Radiographic and Clinical Outcomes
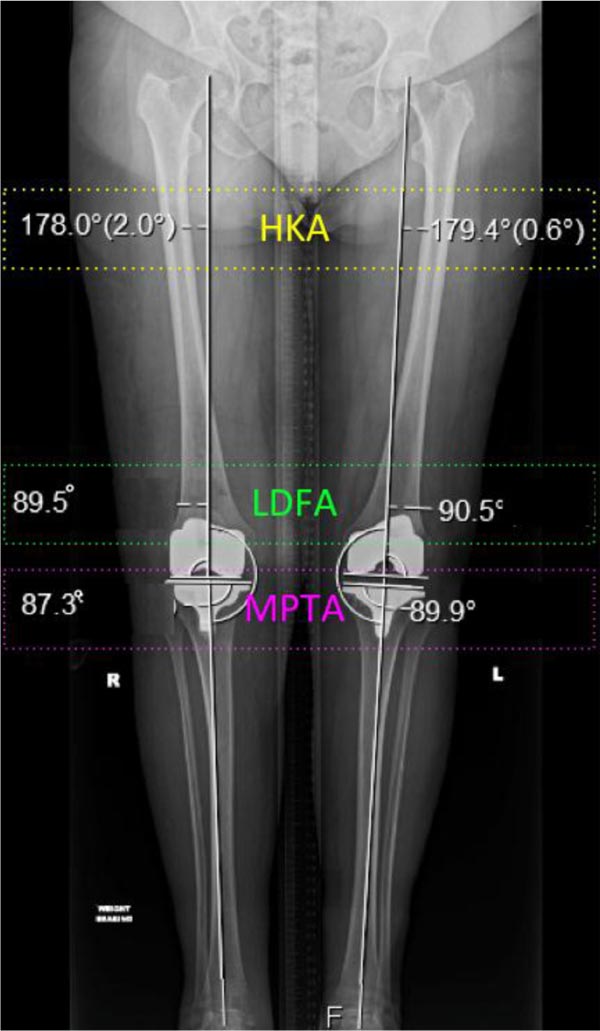
The radiographic outcomes are illustrated in Figs. (4 and 5). No complication occurred during or after surgery, and the patient was discharged home on the third post-operative day. On post-operative day two, her prosthetic knee active ROM ranged from a few degrees of fixed flexion deformity to 100° of flexion (Fig. 6). At the six-week clinic review, the patient reported no pain or instability in the operated knee and had a ROM of 0-125°. At the first operative anniversary, the patient’s subjective satisfaction rate was 100/100, and the Oxford Knee Score increased from a pre-operative value of 17 to 46.


3. CASE 2
An 82-year-old female with bilateral valgus knee osteoarthritis (OA) (Fig. 7a). The right knee OA was bone-on-bone, with substantial bone loss, 17° valgus deformity, and with a firm endpoint under valgus stress-test suggestive of a functional medial collateral ligament. Using the same concepts as described above, a restricted KA (rKA) TKA [3, 7, 8] was performed using computer navigation (Fig. 7b, c). During surgery, using zones of intact cartilage or minimal wear, we estimated the patient’s pre-arthritic knee anatomy (distal femur joint line with 8° valgus, proximal tibia with 2° varus). To fit within the rKA thresholds, correction of the patient’s anatomy was performed only on the femoral side, reducing her pre-arthritic femoral valgus angle from 8° to 5°. On the tibial side, we reproduced her physiological 2º of varus. Posterior femoral resection was sy mmetrical (0º rotation). Using spacer blocks, pie-crusting of the posterolateral corner was performed to obtain a balanced knee. Knee stability and good patellar tracking were confirmed with trial implants. An uncemented cruciate-retaining TKA was implanted. On post-operative radiographs, the femoral component was orientated at 5.5° valgus and the tibial component 2° varus for a resultant HKA of 3.5° valgus (Fig. 7). The patient had an uneventful post-operative period. Five years after surgery, she is still very satisfied.
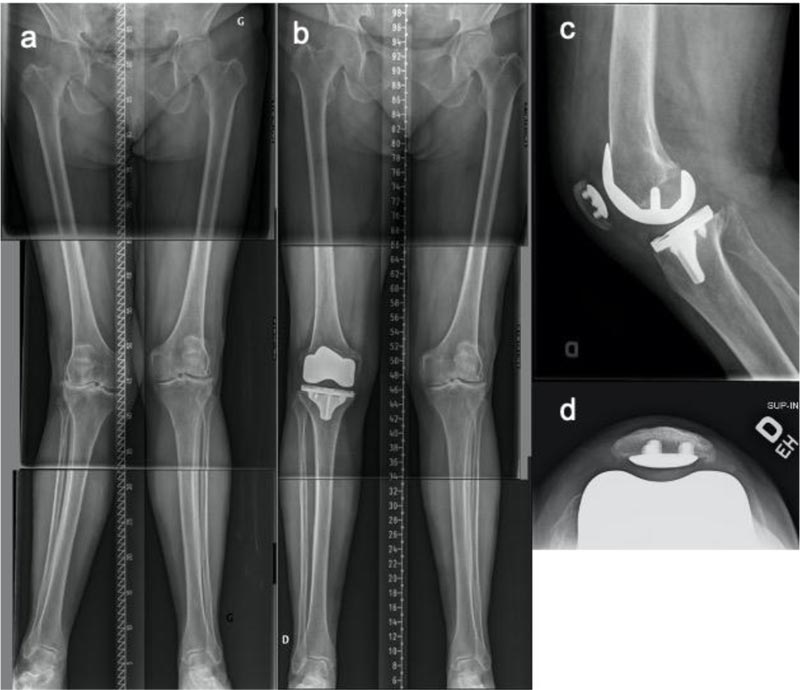
4. CASE 3
A 74-year-old male with severe varus OA of the left knee treated with rKA TKA (Fig. 8). Severe bone loss was present on both the medial femoral condyle and the medial tibial plateau. Using computer navigation and following the aforementioned steps to quantify bone loss, we estimated the knee pre-arthritic alignment: distal femoral joint surface 2º of the valgus and tibial joint surface 10º varus relative to femoral and tibial mechanical axis, respectively. In accordance with the rKA technique, the patient’s anatomy was maintained on the femur (2° of valgus), and the tibial varus angle was reduced from 10° to 5° to obtain a final HKA of 3° varus (intra-operative computer navigation data). Sy mmetrical resection of the posterior femoral condyles was performed (neutral rotation). With trial implants, the knee was well balanced throughout the ROM, and with no collateral ligament release except the deep medial collateral ligament, as part of the approach. The PCL was considered severely degenerative, so a cemented posterior-stabilised TKA was implanted. The radiographic implant orientations were: femur 1° valgus and tibia 6° varus (Fig. 8). At the one-year follow-up and thereafter, the patient had a knee ROM of 0-120º and was able to walk without a walking aid for more than an hour. The patient, unfortunately, died of a cause unrelated to his TKA eight years post-operatively.
5. RESULTS
For all 3 cases, soft tissue laxity was restored with medial and lateral knee compartments with respectively 1 to 2 mm and 2 to 3 mm laxity, Standard TKA implants without bone augment or stem extension were used in all cases: 2 CR and 1 PS implant. After a minimum of one year post surgery, the three patients are satisfied and do not report instability or stiffness.
6. DISCUSSION
It is important to develop skills to ‘read’ the joint and find the appropriate plan which enables the closest restoration of the native knee anatomy. The combination of careful analysis of the pre-operative radiographs, intra-operative observation of articular surfaces, and assessment of gaps and laxity of the collateral ligaments throughout knee ROM are important steps for planning, performing, and quality-checking KA TKA implantation, especially in complex cases with significant bone loss.
Most surgeons would consider these patients to have a severe constitutional deformity, lateral femoral condyle hypoplasia (cases 1 and 2), and stretched collateral ligaments. Therefore, they may have chosen to use a more invasive, ste mmed, augmented, and constrained component. It is surprising how simple the KA TKA surgery was in those cases, avoiding or minimising the need for ligamentous release and allowing the implantation of unconstrained implants.
Regarding the first case where a pure (unrestricted) KA was intended, it is impossible to ascertain close restoration of the patient’s pre-arthritic knee anatomy as the joint was severely worn. Nevertheless, the uniform femorotibial and patellofemoral balance throughout the knee ROM and the excellent clinical outcomes suggest that the native knee anatomy and balance have likely been adequately restored.
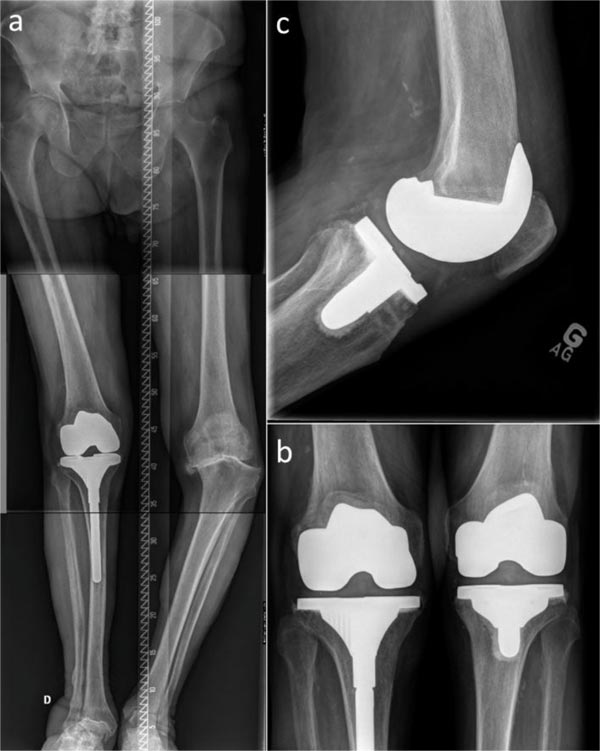
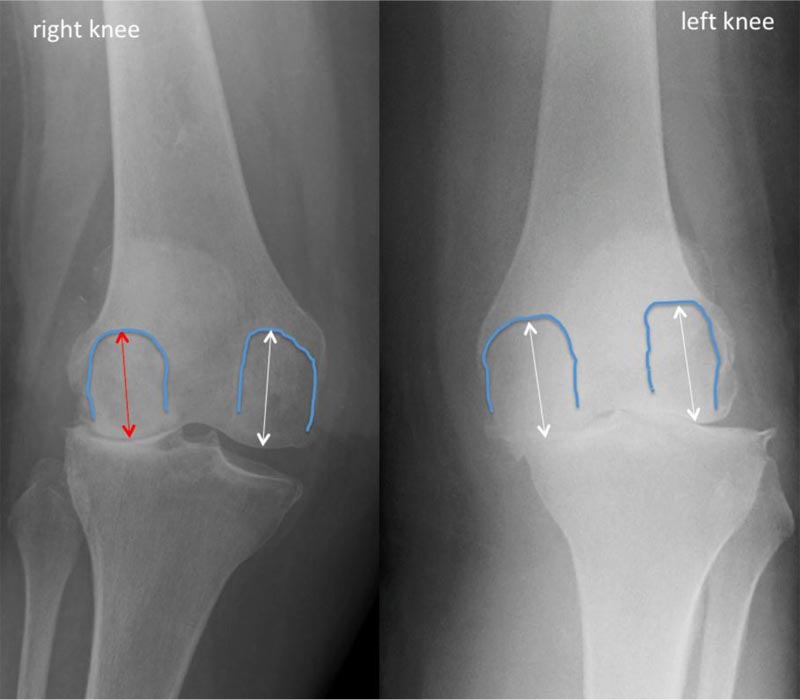
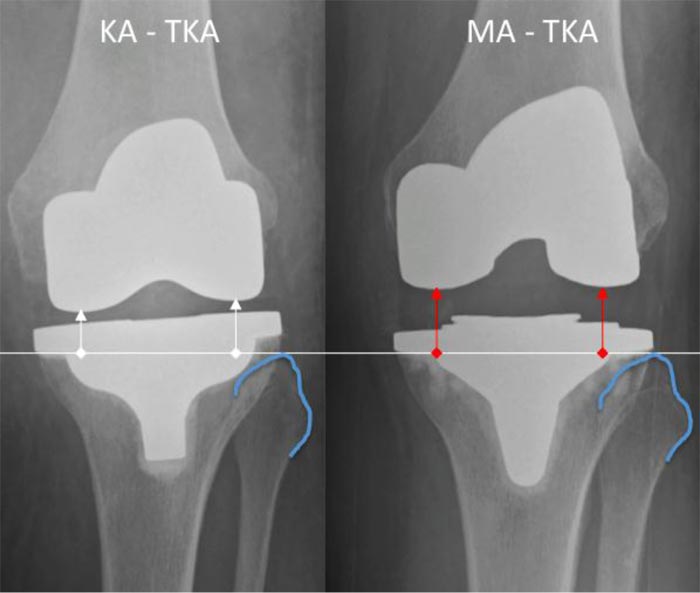
The fact that degenerative valgus knees often have a distal femoral epiphysis that is oriented in high valgus [9] and are prone to femoral bone loss probably explains why the lateral condyle of valgus knees is often thought to be dysplastic. If condylar radii were compared in Case 1, it would have shown a lateral condyle much smaller than the medial (Fig. 9), which in fact was the result of a 5 mm condylar bone loss. Regarding Case 1, the left MA TKA has altered the original joint line orientation and height much more than the right KA TKA (Fig. 10). Theoretically, the more the knee anatomy is altered, the less physiological the prosthetic knee kinematics will be, and the functional performance will be impaired.
CONCLUSION
Severe bone loss does not preclude performing kinematically aligned TKA. The combination of careful analysis of the pre-operative radiographs, intra-operative observation of articular surfaces, and assessment of laxity of collateral ligaments throughout knee ROM are important steps in achieving adequate KA implantation that ensure an optimal outcome.
AUTHORS' CONTRIBUTION
(1) The conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) Drafting the article or revising it critically for important intellectual content, (3) Final approval of the version to be submitted: C.Rivière: 1-2-3; J.Webb: 2-3; P-A.Vendittoli: 1-2-3.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed patients consent was obtained from all subjects prior to the study.
FUNDING
None.
CONFLICT OF INTEREST
Charles Rivière declares being a paid consultant for Medacta; Pascal André Vendittoli declares being a consultant for Microport, Medacta, Stryker, Ethicon, and Johnson & Johnson; Jeremy Webb declares no conflict of interest related to or outside the current study.
ACKNOWLEDGEMENTS
Declared none.


