All published articles of this journal are available on ScienceDirect.
Extended Routine Follow-up of Primary Uncomplicated Hip and Knee Arthroplasty is not Necessary
Abstract
Aims:
To create a more effective system to identify patients in need of revision surgery.
Background:
There are over 160,000 total hip and knee replacements performed per year in England and Wales. Currently, most trusts review patients for up to 10 years or more. When we consider the cost of prolonged reviews, we cannot justify the expenditure within a limited budget.
Study Design & Methods:
We reviewed all patients' notes that underwent primary hip and knee revision surgery at our institution, noting age, gender, symptoms at presentation, referral source, details of the surgery, reason for revision and follow up history from primary surgery.
Results:
There were 145 revision arthroplasties (60 THR and 85 TKR) that met our inclusion criteria. Within the hip arthroplasty group, indications for revision included aseptic loosening (37), dislocation (10), and infection (3), periprosthetic fracture, acetabular liner wear and implant failure. All thirty-seven patients with aseptic loosening presented with pain. Twenty-five were referred from general practice with new symptoms. The remaining were clinic follow-ups. The most common reason for knee revision was aseptic loosening (37), followed by infection (21) and then progressive osteoarthritis (8). Most were referred from GP as a new referral or were clinic follow-ups. All patients were symptomatic.
Conclusion:
All the patients that underwent revision arthroplasty were symptomatic. Rather than yearly follow up, we recommend a cost-effective system. We are implementing a 'non face-to-face' system. Patients would be directly sent a questionnaire and x-ray form. The radiographs and forms will be reviewed by an experienced arthroplasty surgeon. The concerning cases will be seen urgently in a face-to-face clinic.
1. INTRODUCTION
There are over 160,000 total hip and knee replacements performed per year in England and Wales alone [1]. Currently, most trusts maintain reviewing patients for a minimum of 1 year and possibly extending to 10 years or more. This is to ensure that potential complications are picked up early and to assess for the restoration of function and alleviation of pain.
Revision arthroplasty is often technically easier when bone stock and soft tissue destruction is minimal. It also allows for the surgeon to have a larger range of choice of implants for the second sitting.
Apart from metal on metal arthroplasties, hip revision cases are still not very common. The National Joint registry (2003-2014) [1] has shown a cumulative percentage of revision for men to range from 0.71 to 0.79 at 1 year. At 5 years, this is 1.91- 4.35 and at ten years it ranges from 3.34 to 8.87. Higher rates of revision were seen in men under the age of 55. The National Joint Registry demonstrated low rates in those over the age of 75 years. A similar trend was found in women undergoing arthroplasty.
The National Joint Registry (NJR) [1] shows that the average hospital performs 686 primary Total Hip Replace-ments (THRs), 692 primary Total Knee Replacements (TKRs) and 83 Uni-compartmental Knee Replacements (UKR) over a three-year period spanning from April 2015 until March 2018. Our institution performs 1372 primary THRs, 1573 TKRs and 179 UKRs. 166 revision total hip replacements and 187 revision total knee replacements were performed in the same period. Though this is higher than the NJR average of 70 revision THRs and 50 revision TKRs, when considering the high volume of cases, the ratio is comparable.
When we consider the cost of prolonged yearly reviews of this large volume of patients with uncomplicated hip and knee arthroplasty, we cannot justify the expenditure. Each clinic that is manned by a nurse or doctor; each radiograph and each time slot taken can be better utilised within the limited budget of the National Health Service.
A vast majority of patients requiring revision surgery will present with symptoms; such as worsening pain, swelling and deformity. It is rare for a patient to be completely asympto-matic prior to surgery.
Keeping this in consideration, we reviewed if routine extended follow up of primary lower limb arthroplasty effectively and efficiently detected patients that would require revision surgery.
2. METHODS
We reviewed all patients’ notes that underwent primary hip and knee revision surgery at our institution. Patients were identified using our theatre databases that were coded as revision.
We noted the following:
Age, gender, symptoms at presentation, referral source, details of the surgery (including implants), reason for revision and follow up history from primary surgery.
We excluded incomplete records, those who had undergone previous revision surgery of the same site, metal-on-metal revisions, due to the separate protocol, those who underwent revision for failed hemiarthroplasties and lastly primaries that were less than 1 year old.
3. RESULTS
There were 145 revision arthroplasties (60 total hip replacements and 85 total knee replacements) that met our inclusion criteria.
3.1. Hip
Within the hip arthroplasty group, there were 28 females and 32 males with ages ranging from 41 to 89 years (average 72 years). All the patients met the inclusion criteria.
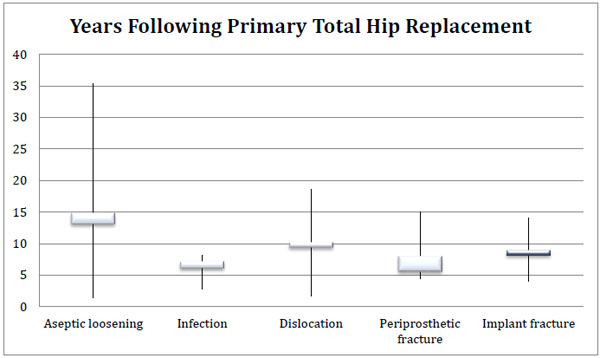
Indications for revision included aseptic loosening (37), dislocation (10), and infection (3), periprosthetic fracture, acetabular liner wear and implant failure. The majority were either fully cemented or fully uncemented. One-third of the patients were followed up in the clinic and the rest were referred. Two of the patients had their primary total hip replacement performed in a different unit. All were symptomatic, presenting with pain, instability/ dislocation and acute fractures. (Fig. 1) demonstrates the breakdown of the reasons for revision.
The time period between primary arthroplasty and revision ranged from 1.63 to 35.3 years (average 7.7 years) as seen in (Fig. 2).

All thirty-seven patients with aseptic loosening presented with pain alone or both pain and new gait abnormalities. Two of the aseptic loosening cases had their primary prosthesis performed in a different unit. Twenty-five of the patients were referred from their General Practitioner (GP) with new symptoms of pain. The remainder had been followed up through clinic.
Those presenting with late infected prostheses (beyond 5 years) were part of ongoing follow up prior to revision. All of the infected cases had symptoms and signs without significant radiological evidence of bone loss.
There were 2 cases of ceramic head fracture and one of femoral stem fracture (ranging 4- 14 years). Two cases of acetabular liner wear occurred at 12 and 21 years. There was one episode of acute acetabular liner dislocation beyond 1 year.
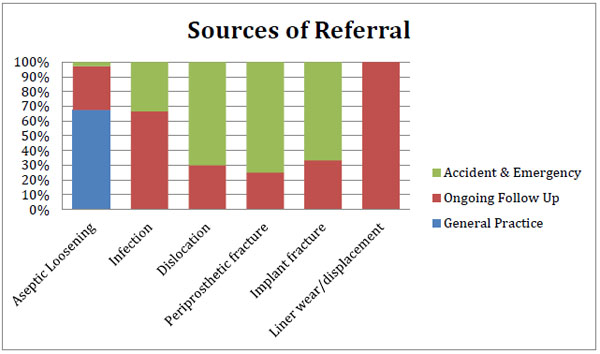
The Accident and Emergency unit (A&E) was the main source of patients presenting with dislocation (8 cases), periprosthetic fracture (4 cases) and stem or ceramic head fracture (2 cases).
(Fig. 3) demonstrates the reasons for revision and the sources of referral. Accident and Emergency (A&E) and ongoing clinic follow up were the main ways patients were identified for infection, dislocation and fractures.
3.2. Knee
Ninety-nine cases for knee arthroplasty were identified of which eighty-five met the inclusion criteria. The ratio of men to women was similar to the hip cohort with 43 males to 42 females, aged between 42 and 95 years. Seventy of the primary knees were performed in our institution.
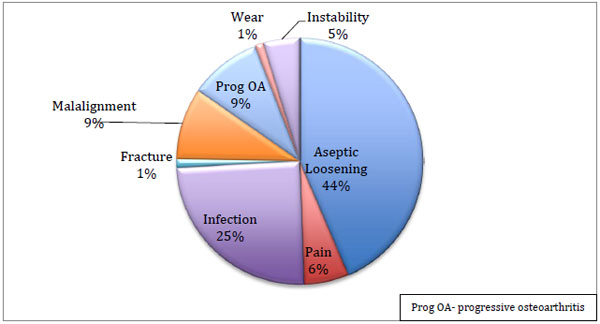
The most common reason for the revision was aseptic loosening (37), followed by infection (21) and then progressive osteoarthritis (8) and malalignment (8). Other causes included fracture, progressive osteoarthritis (OA) and instability (Fig. 4).
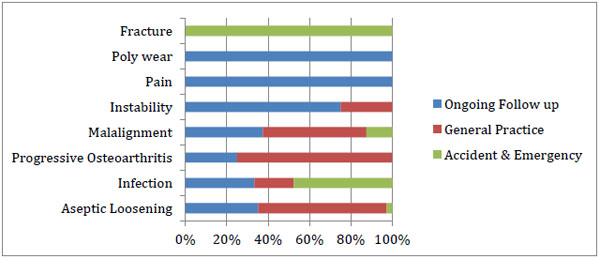
Most were referred from general practice as a new referral or already had ongoing follow up. A few presented from accident and emergency(A&E) as acute trauma, as demonstrated in Table 1 and (Fig. 5).
Amongst those that had their primary knee replacement performed in another unit, eight had aseptic loosening (53%), six had an infection (40%) and one was malaligned (7%). For those that had their primary in our institution, aseptic loosening was the most common reason (41%) followed by infection (21%) and other causes listed previously.
All patients were symptomatic, with pain being a predominant feature. Signs and symptoms of infection and instability were present in a few cases. Revisions were also performed in the trauma setting.
An average of 4 years (1.09-20.5 years) between primary knee arthroplasty and revision was found. For aseptic loosening, this was 6.5 years, ranging from just over 1 year to 20 years post-primary. Patients that had uni-compartmental knee replacements required revision at approximately 5 years, for progressive osteoarthritis.
| - | Ongoing Follow Up | General Practice | Accident & Emergeny |
| Aseptic Loosening | 13 | 23 | 1 |
| Infection | 7 | 4 | 10 |
| Progressive Osteoarthritis | 2 | 6 | 0 |
| Malalignment | 3 | 4 | 1 |
| Instability | 3 | 1 | 0 |
| Pain | 5 | 0 | 0 |
| Poly wear | 1 | 0 | 0 |
| Fracture | 0 | 0 | 1 |
All patients who had reported ongoing pain post-primary arthroplasty within our institution and subsequently underwent revision were regularly seen in clinic and were not discharged.
4. DISCUSSION
It is difficult to justify long term follow up in patients who have had uncomplicated hip and knee arthroplasties. When considering the statistics of revision on the National Joint registry, a significant number are performed for aseptic loosening and infection.
Diduch et al found that even in younger patients below the age of 55 years undergoing total knee arthroplasty the failure rate was still low with 18-year survivorship of 87% [2]. Considering this age group are often more active and as such take the prosthesis through a higher number of cycles, the evidence still does not support routinely reviewing them. Many of these patients were involved in skiing, cycling and had strenuous physical jobs such as construction, yet two were revised due to late infection and few for polyethylene wear on the patella or tibial component.
With uni-compartmental knee replacement, Argenson et al found a low rate of revision of 94% at ten years with progression of arthritis in other compartments being the common reason for revising [3]. Though they recommended routine long term follow up, the patients often presented with complaints of pain from the non-resurfaced compartments.
This is supported by the ten year follow up of the Oxford medial uni-compartmental knee which also found a 94% survivorship at 10 years [4]. Evidence of radiolucency on x-ray at 6 years did not correlate with progression. Again, the progression of arthritis in other components was the main indication for revision.
The literature for hip arthroplasty revisions also shows a high rate of patients presenting with symptoms. The most common indications were instability and loosening [5, 6].
We do appreciate that with loosening in total hip replace-ments, patients may be asymptomatic during the early stages. However, there may not be obvious radiological changes. It is also not uncommon for patients to present with pain and discomfort prior to radiographical evidence of loosening.
Amongst the hip cohort, a majority of the patients had aseptic loosening beyond ten years. Yearly x-rays prior may have identified evidence of loosening but may not have altered the timing of surgical intervention.
In our institution, we have found that patients often present with symptoms and not found incidentally on routine follow up. One has to weigh the pros and cons of this. Patients often have to pay for their own transportation and parking to be seen on a yearly basis when they are satisfied with their outcome. The clinics have to be manned by nurses and/ or doctors as well as radiologists and administration staff.
We understand that one of the limitations of this study is that the numbers are relatively small compared to that of the national joint registry; therefore, it is difficult for us to state that no form of follow up is required.
We are planning on moving to a ‘non face-to-face’ system. This would drastically reduce the costs and work-load of following up these patients but allow reassurance that long-term surveillance is still occurring. Patients will still be seen routinely within the first year.
After the one-year anniversary, patients would be directly sent a questionnaire and x-ray form on a yearly basis. The questionnaire will include questions required for the Patient Reported Outcome Measures (such as the Oxford Hip and Knee Score) and specific questions on new or worsening pain, instability, and symptoms and signs of infection. The radiographs and the questionnaires will be reviewed by an experienced arthroplasty surgeon. This will be conducted in a way similar to a virtual fracture clinic. Those that submitted outcome forms that were concerning, or had radiological evidence of abnormalities would be seen urgently in a face-to-face clinic.
Virtual fracture clinics have been found to be an effective way to identify patients that require urgent in-person review and also increase the capacity for patient review [7, 8]. It has been adopted in many units in the United Kingdom with good outcomes [9].
By utilising a similar system for arthroplasty follow-ups, we envisage that we will reduce our waiting times for clinic appointments and thus increase the number of patients being treated within the 18-week target.
CONCLUSION
All the patients that underwent revision arthroplasty for both knees and hips were symptomatic in some form. Patients who did not progress well and had ongoing symptoms of pain were never discharged from follow up.
Routine follow-up of uncomplicated primary lower limb arthroplasty beyond the first post-operative year does not reliably capture the majority of patients who require subsequent revision surgery. It is very likely that the routine follow-up in its current form may no longer be necessary.
Our proposed system of a “virtual fracture” clinic style yearly radiograph and patient questionnaire would capture problematic cases and streamline service provision.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available at the Trauma and Orthopaedic Department at the Mid Yorkshire National Health Care Trust, Yorkshire, United Kingdom at https://www.midyorks.nhs.uk/.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


