All published articles of this journal are available on ScienceDirect.
Quadriceps Tendon Rupture Following Total Knee Arthroplasty
Abstract
Introduction:
Rupture of a Quadriceps Tendon (QT) following a Total Knee Arthroplasty (TKA) is a rare complication. The purpose of this study was to report outcomes and complications of QT repair following TKA.
Methods:
From a cohort of 437 QT repairs, 19 individuals were identified who had previously undergone a TKA on the ipsilateral leg. Data was collected on individuals with a minimum follow up of 3 months post QT repair (n=16), including Knee Society Scores, pre and post-operative lag, and pre and post-operative range of motion.
Results:
13 patients were treated with End-to-End (EE) repairs and 6 were treated with transosseous or suture anchor repair (ATO). In the ATO group, there was no difference in pre (68.0 ± 22.5) and post KSS (82 ± 9.16) (p=0.231), but in the EE group, there was a significant improvement in KSS (pre=67.8 ± 13.1, post=86 ± 16.75, p=0.0027). There was significant difference in post-operative extension lag between ATO (26.0 ± 12.6) vs. EE (4.0 ± 2.74) (p=0.0083). Four out of six ATO patients had extension lag ≥10 degree extensor lag (66.7%) compared to 2 out of 13 (15.4%) patients in the EE group. Compared to EE, ATO repair had an 8.00 times odds of re-tear (95% CI: 0.53,120.6; p=0.133) and 2.75 times greater risk of infection (95% CI: 0.284, 26.61; p=0.382).
Conclusion:
Patients who underwent EE repair had better functional improvements compared to the ATO group and smaller extension lag.
1. INTRODUCTION
Rupture of the quadriceps tendon following a total knee arthroplasty (TKA) is relatively uncommon. The incidence of this complication is estimated to be between 0.1% and 1.1% [1, 2]. Attempts to repair the tendon often have poor prognoses leading to lifelong consequences for patients requiring repeat interventions [3, 4]. Presently, there are three main techniques for treating these tears, including end-to-end primary repair, suture through bone tunnels, and repairs using suture anchors [5, 6]. Due to the uncommon nature of this event, it is still unclear which of these techniques is superior. The purpose of this study is to compare outcomes of two repair types in the largest cohort in the literature.
2. MATERIALS AND METHODS
After obtaining approval from our Institutional Review Board, we searched the surgical database at our institution for quadriceps repair surgeries performed between January 1, 2008, and December 31, 2016. Our integrated health care system includes 14 medical centers with over 100 orthopaedic surgeons. Our system does not catalogue surgical cases by CPT codes, rather by interfacility codes. We, therefore, searched for “quadriceps tendon repair” and “open repair of tendon, knee” in our database to identify patients who had undergone a quadriceps tendon repair. A retrospective chart review was then performed to identify those patients who had a prior total knee arthroplasty (TKA) who underwent surgical repair of a quadriceps tear. The operative reports, progress reports, and History and Physical examination, physical therapy notes, and emergency room notes were reviewed and relevant data collected.
Data gathered included age, gender, side of surgery, BMI, use of statins, the length of time between TKA and quadriceps rupture (months), and the length of time from quadriceps rupture to surgical repair. In addition, pre- and post-operative Knee Society Scores (KSS) [7, 8], range of motion including extensor lag were recorded. Pre-operative knee society scores were not available in 2 patients and post-operative KSS was only assessed for patients with a minimum of 3 months post QT repair, leaving scores for 16 patients.
Details from the operative report including tourniquet time, repair type, patellar thickness after resection (mm), patellar polyethylene thickness (mm), implant manufacturer, use of auto- or allograft, were recorded. Complications including re-rupture, infection, and thromboembolic events were recorded. Patients underwent a 6 week period of immobilization and hinged bracing, as well as non-weight bearing for 6 weeks. Knee flexion was slowly increased each week by a physical therapist.
Chi-square and Fisher’s exact tests were used to compare categorical variables. Means and medians of continuous variables were compared using t-tests and Kruskal-Wallis tests as appropriate. Unadjusted odds ratios were calculated using logistic regression. All P values were 2-sided with an alpha = 0.05. Statistical analyses were performed with SAS 9.3 (SAS Institute, Cary, NC).
3. RESULTS
3.1. Patient Demographics
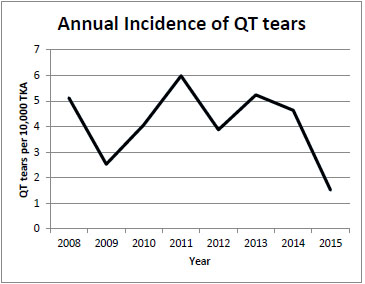
Our database search identified 437 QT repairs. After chart review, we identified 19 patients who sustained a QT disruption following a total knee arthroplasty. The average incidence was 5.5 per 10,000 TKA. Fig. (1) shows the average annual incidence.
There were 10 (52.6%) females. The average age was 67 years (range, 43 to 88 years) at the time of the QT rupture. Fifteen patients were Caucasian, three African-American, and one Asian. Eighteen individuals underwent a TKA for a diagnosis of osteoarthritis and one for rheumatoid arthritis. With respect to predisposing risk factors, there were three active smokers, four patients with diabetes mellitus, eight taking statin medications, and one with stage three chronic kidney disease (Table 1). The average time between TKA to quadriceps tear was 17.2 months (range 1 to 80).
Fifteen disruptions occurred after a primary total knee arthroplasty and four followed a revision total knee arthroplasty. The quadriceps tendon tore as a result of a fall in twelve patients, gradual failure without major event in three patients, and following a peri-prosthetic fracture revision, knee dislocation rising from sitting to standing, and trauma during physical therapy in one patient each (Table 1). The average time from the tear to surgery was 1.86 months (range .13 to 70).
| AGE | GENDER | MECHANISM OF INJURY | TIME FROM TKA TO INJURY (DAYS) | PROSTHESIS` | NOTES |
|---|---|---|---|---|---|
| 43 | M | Fall | 28 | Smith & Nephew Genesis II | - |
| 72 | F | Sitting to standing | 56 | Smith & Nephew Genesis II | DM2, taking statins, had infection/DVT |
| 62 | M | Physical Therapy | 22 | Zimmer Natural Knee | Smoker |
| 59 | M | Fall | 1603 | Zimmer Nexgen | - |
| 82 | F | Fall | 231 | J&J Depuy Sigma revision | Taking statins |
| 45 | F | Fall | 2004 | J&J Depuy Sigma revision | TKA due to Rheumatoid Arthritis, had infection |
| 64 | M | Fall | 22 | J&J Depuy Sigma | - |
| 61 | F | Periprosthetic fracture | 0 | J&J Depuy Sigma (revision) | - |
| 72 | F | No major event | No clear DOI | J&J Depuy Sigma (revision) | DM2, taking statins |
| 55 | F | Fall | 21 | Zimmer Nexgen | Sustained re-tear |
| 51 | M | No major event | 48 | J&J Depuy sigma | Smoker |
| 88 | F | Knee dislocations | 30 | Zimmer Persona | Taking statins |
| 73 | M | No major event | 39 | J&J Depuy Sigma | DM2, taking statins |
| 84 | M | Fall | TKA Out of Network | Sulzer Apollo knee | - |
| 71 | F | Fall | 166 | Zimmer Persona | DM2, taking statins, had infection/DVT |
| 68 | M | Fall | 61 | Zimmer Natural Knee | Sustained re-tear |
| 68 | F | Patella Fracture | 12 | Zimmer Nexgen | - |
| 73 | M | Fall | 566 | J&J Depuy Sigma | Stage 3 CKD, taking statins |
| 74 | F | Fall | 1020 | Smith & Nephew Genesis II | Taking statins, sustained re-tear |
| AGE | GENDER |
PARTIAL/ COMPLETE TEAR |
LOCATION OF TEAR | TYPE OF REPAIR | RETEAR | NOTES/OTHER |
|---|---|---|---|---|---|---|
| 43 | M | Partial | Midsubstance | EE | N | - |
| 72 | F | Complete | Superior pole of patella | EE | N | Concomitant lower extremity hardware removal and placement of antibiotic spacers |
| 62 | M | Partial | Superior pole of patella | EE | N | - |
| 59 | M | Partial | Superior pole of patella | EE | N | - |
| 82 | F | Complete | Vastus Medialis | EE | N | - |
| 45 | F | Complete | Superior pole of patella | EE | N | - |
| 64 | M | Complete | Midsubstance | EE | N | - |
| 61 | F | Partial | Vastus Medialis | EE | N | - |
| 72 | F | Partial | Superior pole of patella | EE | N | - |
| 55 | F | Complete | Vastus Medialis | EE | Y | - |
| 51 | M | Partial | Rectus Femoris | EE | N | - |
| 88 | F | Partial | Superior pole of patella | EE | N | Concomitant L TKA revision with polyethylene liner |
| 73 | M | Partial | Superior pole of patella | EE | N | - |
| 84 | M | Complete | Superior pole of patella | Transosseous | N | Went in for a TKA revision a few years after his QT repair, Came back some time later with a slight lag, but no reoperation performed |
| 71 | F | Complete | Superior pole of patella | Transosseous | N | Ipsilateral Knee irrigation/debridement |
| 68 | M | Complete | Superior pole of patella | Transosseous | Y | Re-operated with 3 Orthocord Quickanchor suture anchors, and augmented with two semitendinosus allografts |
| 68 | F | Complete | Superior pole of patella | Transosseous | N | - |
| 73 | M | Partial | Superior pole of patella | Transosseous | N | - |
| 74 | F | Partial | Superior pole of patella | Anchor Suture | Y | Sutures did not rip out, instead had a gradual elongation of the tendon, re-operated with two Mitek Suture Anchors, recovered after second reoperation |
3.2. Surgical Findings
Nine patients had complete tears and ten had partial tears. Of those partial tears, 7 were off the superior pole of the patella, 1 from the vastus medialis, 1 from the rectus femoris, and 1 was a midsubstance tear (Table 2). Of the 9 complete tears, 6 were from the superior pole of the patella, 2 from the vastus medialis, and 1 was a midsubstance (Table 2). Three patients underwent a concomitant operation; a lower extremity hardware removal and placement of antibiotic spacers; a left TKA with revision polyethylene liner; and a right knee irrigation and debridement.
The QT was repaired in two main methods, suture Anchor or Trans-Osseous repair (ATO)9 (1 anchor, 5 trans-osseous) and End to End (EE) (13 patients) [5, 6]. Of the ATO repairs, 4 were complete tears, with only suture anchor repair being done on one of the two partial tears in this group (Table 2). Of the EE repairs, 8 were partial tears and 5 complete tears.
3.3. Implant Characteristics
Of the TKA implants used, 9 were Johnson and Johnson, 6 Zimmer, 3 Smith and Nephew, and 1 Sulzer Apollo knee replacements (Table 1). There were 8 Sigma (Johnson and Johnson, Warsaw, IN), 3 Genesis II (Smith and Nephew, London, UK), 3 Nexgen, 2 Persona, 2 Natural Knee (Zimmer, Warsaw, IN), and 1 Apollo (Sulzer, Austin, TX) systems used. The average patella thickness following the TKA was 18.3mm (range, 15.1mm-24.9mm).
3.4. Clinical Findings
There was no significant difference in the time from QT tear to surgery between patients with ATO repair (52.6 +89 days) and those with EE repair (58.4+78 days) (p=.21). Overall, there was a significant improvement of KSS from 70 to 85 (p=0.0015) after QT repair surgery. There was no significant difference between ATO and EE in pre- KSS (ATO=68.0 ± 22.5 vs. EE=67.8 ± 13.1, p=0.98), post- KSS (ATO=82 ± 9.16 vs. EE=86 ± 16.75, p=0.196) and ROM (ATO=26-114°, EE=4-104°, p=0.057). In the ATO group, there was no difference in pre (68.0 ± 22.5) and post KSS (82 ± 9.2) (p=0.231), but there was a significant difference in the EE pre and post KSS (pre=67.8 ± 13.1, post=86 ± 16.75, p=0.0027). There was a significant difference in ATO versus EE in post-op extension lag (ATO=26.0 ± 12.6 vs. EE=4.0 ± 2.74, p=0.0083). Only two of the thirteen patients in the EE group had extensor lags greater than or equal to ten degrees, compared to 4 of 6 in the EE group. The average postoperative flexion was 111 degrees (range, 75-135 degrees) with 11 of 19 patients being able to flex their knee 120 degrees or greater.
There were 3 (15.7%) infections and 2 (10.5%) deep vein thromboses. Three (15.7%) patients had re-tears, 2 in the ATO group (1 trans-osseous, 1 suture anchor) and 2 in patients with complete tears. Compared to EE, ATO repair had an 8.00 times odds of re-tear (95% CI: 0.53,120.6; p=0.133) and 2.75 times greater risk of infection (95% CI: 0.284, 26.61; p=0.382).
4. DISCUSSION
The findings of this study show that quadriceps tendon repair following a total knee arthroplasty can improve active knee extension and improve patients’ functional outcomes. The EE group had significant improvement in functional outcome and less extension lag compared to the ATO group.
Surgeons often favor EE repairs on patients with partial tears, and perform ATO repairs when the patient has a complex, complete tear. Therefore, the poorer outcomes with regards to post-operative extensor lag would be expected for the ATO group. The idea that the severity of the initial trauma correlates with functional outcomes is supported by the fact that 67% of the ATO group had a lag ≥ 10 degrees compared with just 15% of the EE group.
Additionally, this study showed a low re-rupture rate, even among the more severe complete tears (Table 2). Treatment options should be made on a case by case basis using current guidelines: EE for partial tears and trans-osseous repair for complete tears [3, 4, 10]. The single tear repaired with a Suture Anchor (SA), however, re-ruptured, whereas only one of the four complete tears repaired with trans-osseous repair failed. We believe that the SA technique may be more prone to failure due to the poor bone quality and thinner viable bone available after patellar resurfacing during a TKA. This conclusion supports findings by Bushnell et al. [9] who acknowledged the propensity for suture anchors to undergo stripping during insertion, something that is sure to be magnified in patients with TKAs. This does, however, conflict with the findings in Lighthart et al. [11], but this study did not take into account the thinning of the patella during a TKA. Since there was only one patient in our study that fell into this category and this information conflicts with other studies on the same subject with similarly limited data, more research must be done to confirm this recommendation [6].
The poor outcomes found in this study in regards to re-rupture rate and postoperative extensor lag are consistent with those in other papers that document the low success rate of this procedure [2-4, 12]. Although the average KSS increased, there was still a relatively high rate of complications. The rate of infection is consistent with that found in other studies, however, DVTs and re-tears were lower than those seen in previous reports [2, 5].
This study is limited due to the small number of patients who qualified for inclusion, especially once individuals were split into ATO and EE cohorts. Furthermore, due to the susceptibility of complications from outside factors, conclusions for long-term outcomes from the procedure may need more exploring. Finally, due to the nature of this surgical procedure, these results are difficult to duplicate since surgeons use different techniques for their repairs and the variable degree in which QT tears can present does not allow for consistency in treatment. Outcomes are slowly continuing to improve, and new techniques are being tested with varying degrees of success, though the overall success of this procedure remains low [12-15]. Nevertheless, it is important to identify these issues quickly and intervene accordingly.
CONCLUSION
Patients who underwent end-to-end repair of quadriceps tendon following total knee arthroplasty had better functional improvements compared to the ATO group and smaller extension lag
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the ethics committee of Tulane School of Medicine, USA.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


