All published articles of this journal are available on ScienceDirect.
Open Pelvic Fractures: Review of 30 Cases
Abstract
Background:
Open pelvic fractures are rare but usually associated with a high incidence of complications and increased mortality rates. The aim of this study was to retrospectively evaluate all consecutive open pelvic fractures in patients treated at a single Level-1 Trauma Center during a 10-year interval.
Patients and Methods:
In a 10-year interval, 30 patients with a diagnosis of open pelvic fracture were admitted at a Level-1 Trauma Center. A retrospective analysis was conducted on data obtained from the medical records, which included patient’s age, sex, mechanism of injury, classification of the pelvic lesion, Injury Severity Score (ISS), emergency interventions, surgical interventions, length of hospital and Intensive Care Unit stay, and complications, including perioperative complications and death. The Jones classification was used to characterize the energy of the pelvic trauma and the Faringer classification to define the location of the open wound. Among the survivors, the results were assessed in the last outpatient visit using the EuroQol EQ-5D and the Blake questionnaires. It was established the relationship between the mortality and morbidity and these classification systems by using the Mann-Whitney non-parametric test, with a level of significance of 5%.
Results:
Twelve (40%) patients died either from the pelvic lesion or related injuries. All of them had an ISS superior to 35. The Jones classification showed a direct relationship to the mortality rate in those patients (p = 0.012). In the 18 (60%) other patients evaluated, the mean follow-up was 16.3 months, ranging from 24 to 112 months. Eleven (61%) patients had a satisfactory outcome. The Jones classification showed a statistically significant relationship both to the objective and subjective outcomes (p < 5%). The Faringer classification showed a statistically significant relationship to the subjective, but not to the objective outcome. In addition, among the 18 patients evaluated at the last outpatient visit, the Faringer classification showed statistical significance on the need of colostomy (p = 0.001) in the acute phase of treatment.
Conclusion:
We suggest the routine use of the Jones classification for the emergency room assessment and management of all open fractures of the pelvic ring. We believe the Faringer classification seems to be useful for the abdominal surgeons for the indication of gut transit derivation but not for the acute management of the bony component of an open pelvic fracture.
INTRODUCTION
Open pelvic fractures are one of the most disabling injuries of the skeleton characterized by direct communication between the fracture haematoma and the external environment, including the rectum and the vagina [1]. Although rare, with an estimated rate of 2% to 4% of all traumatic pelvic ring lesions, these injuries predominantly occur in young adults and motorcycle users, typically victims of high-energy accidents, and are usually associated with a high incidence of complications [2]. Almost 75% of the patients are polytraumatized, presenting with associated visceral, thoracic, and lower extremity lesions [3, 4].
The acute management of these injuries continues to be challenging, requiring a multidisciplinary approach. Historically, the mortality rate following pelvic fractures reached rates as high as 50%, but more recently a steady decrease has been observed secondary to the improvements made in all disciplines of emergency medicine and pre-hospital resuscitation protocols [5]. Injury Severity Score (ISS), advanced age, prolonged haemodynamic instability, extend of the degloving, injuries to the bowel and/or bladder, presence of other life threatening injuries, and increased risk of sepsis are some of the important factors that have been known to contribute to the increased mortality rates [6, 7].
The aim of this study was to retrospectively evaluate all consecutive open pelvic fractures in patients treated at a single Level-1 Trauma Center during a 10-year interval.
PATIENTS AND METHODS
Sampling and Data Collection
The Institutional Review Board approved the study. The charts from all patients admitted to our institution between January 2000 and January 2010 with an open pelvic fracture were reviewed by the Senior Author. All skeletal immature patients, patients with incomplete charts, and patients lost to follow-up were excluded from the study. Data obtained from the medical records included patient’s age, sex, mechanism of injury, classification of the pelvic lesion, Injury Severity Score (ISS), emergency interventions, surgical interventions, length of hospital and Intensive Care Unit (ICU) stay, and complications, including perioperative complications and death.
All patients were brought by the rescue regional system of our city and the pre-hospital support was performed in accordance to the recommendations of the Trauma Committee of the American College of Surgeons. At the hospital setting patients were managed according to the ATLS® protocol.
The energy of the pelvic trauma was defined based on the classification of Jones et al. (from now on, Jones classification), which determines the mechanical stability of the pelvic ring and the potential contamination of the open wound [7]. This classification was developed after a multicenter study involving 39 patients that reported an increase in mortality in patients with unstable fracture patterns and perineal injuries with rectal lacerations. This system is currently used to help predict morbidity and mortality based on fracture pattern and associated injuries.
The location of the open wound was determined according to the Faringer et al. external wound classification (from now on, Faringer classification), which correlates the site of the open wound and the need for colostomy [8]. The Faringer system was developed to classify the location of the soft tissue injury anatomically: zone I (perineum, anterior pubis, medial buttock, posterior sacrum), zone II (medial thigh, groin crease), and zone III (posterolateral buttock, iliac crest).
Operating Room (OR) Management Protocol
Patients were taken to the OR as soon they were adequately stabilized or when they needed any surgical bleeding control due to an unstable hemodynamic status. The standard protocol involved irrigation, debridement, and pelvic stabilization at the first opportunity by the members of the orthopaedic surgical team. The choice of implant for stabilization of the fracture was decided by the surgical team and reflected the fracture pattern with consideration of the site of injury and the hemodynamic status of the patient. Skeletal fixation was initially achieved by anterior external fixation in all patients and four patients had posterior percutaneous sacroiliac joint fixation with one cannulated screw either in S1 or S2 during the initial procedure. Intravenous antibiotics and tetanus prophylaxis were done initially for all patients.
Other specialists (abdominal surgeons, vascular surgeons, plastic surgeons, and neurosurgeons) treated all non-skeletal injuries either at the same time or at different times during the Erb phase. Twenty-two (73.3%) patients had associated injuries to other organs and systems. The ‘damage control’ protocol was applied in the 22 patients with associated injuries. These data are shown in Table 1. Five (16.6%) of these patients died during the resuscitation. The other 18 patients were transferred to the ICU for continuation of the resuscitation measures. Four (13.3%) out of those 18 patients died in the ICU during the first 24 hours after hospital admission.
| Associated injuries | Patients (n = 22) |
|---|---|
| Musculoskeletal | 20 |
| Abdominal | 11 |
| Intra-pelvic organs | 07 |
| Thoracic | 04 |
| Cranial | 03 |
| Vascular | 03 |
Outcome Assessment
Patients were followed up in an outpatient basis for our surgical team and all the other professionals involved on the initial treatment. The average follow up was 16.3 months, ranging from 24 to 112 months. The results were assessed in the last outpatient visit using the EuroQol EQ-5D and the Blake et al. questionnaires (from now on, Blake questionnaire) [9].
Statistics
Statistical analysis was performed with the use of the nonparametric test of Mann-Whitney to determine whether there was a correlation between the severity of pelvic injury and the morbidity and mortality rates. The level of significance was defined as p < 5%.
RESULTS
During the period of this study, out of 396 patients that were treated in our institution with pelvic ring injuries, 30 patients met the inclusion criteria (7.6%). There were 25 male and 5 female, with a mean age of 28.4 years old (ranging from 19 to 46 years old). The Injury Severity Score (ISS) ranged from 15 to 41, with an average of 21 [10]. Patient data according to the classification systems used are presented in Table 2.
| Classification | Patients (n = 30) |
|---|---|
| Jones et al. • Class I • Class II • Class III |
17 07 06 |
| Faringer et al. • Zone 1 • Zone 2 • Zone 3 |
04 10 16 |
The patients primarily managed by the ‘damage control’ protocol were operated on for definitive fixation of all skeletal injuries (including the pelvic ring fracture) in an average of seven days after hospital admission (ranging from five to 17 days).
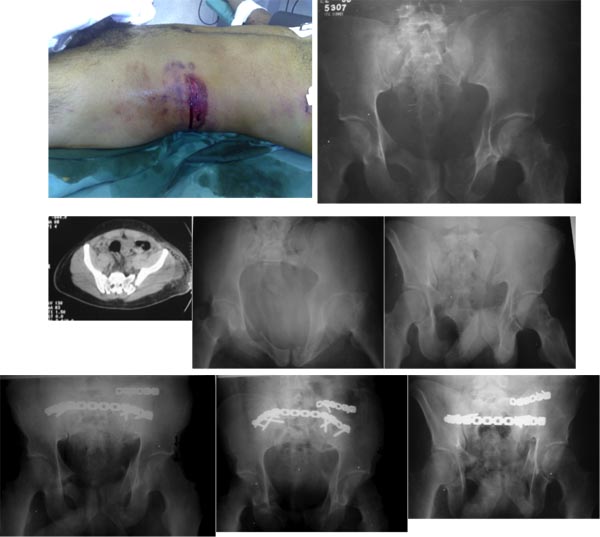
Seven patients had an isolated pelvic ring injury. These patients had definitive pelvic fixation after irrigation and debridement of the open wound (Fig. 1). Of this small group, there was no requirement for post-surgical ICU admission. Three (10%) cases required colostomy and the abdominal surgeons always performed on this procedure.
The total length of hospitalization averaged 19 days, ranging from 6 to 90 days.
Of the 30 patients, 12 (1.6%) died, 5 (16.6%) in the immediate period (during hospital resuscitation), 4 (13.3%) very early (during the first 24 hours of hospital admission), and 3 (10.0%) late (for nonrelated reasons to the pelvic ring injury). All patients that died had an ISS greater than 35, demonstrating the severity of injury in different organs and systems. The Jones classification showed a statistically significant relationship with the mortality rate in these patients (p = 0.012). The Faringer classification was not related to the mortality rate, with p = 0,41.
All 18 (60%) remaining patients attended the last ambulatory visit within the past six months, completing the evaluation questionnaires. The Senior Author always performed the follow-up evaluations. Among the 18 patients evaluated at the last outpatient visit, the Faringer classification showed statistical significance on the need of colostomy (p = 0.001) in the acute phase of treatment. The Jones classification showed a statistically significant relationship both with the objective and subjective results (p < 5%). This leaves an obvious conclusion that the more severe the injury, the worse is the outcome. The Faringer classification showed a statistically significant relationship with the assessment of subjective but not to the objective result (p < 5%).
According to the EuroQol EQ-5D, 11 (36.6%) of the 18 evaluated patients had satisfactory final result and seven (23.3%) had unsatisfactory result. The main factors related to the unsatisfactory results were persistent pain, impotence, and active fistula and chronic infection. Gait disorders and decreased sexual intercourse due to coitus pain were directly related to the symptom of persistent pain in these patients.
The evaluation of Blake’s questionnaire demonstrated that the seven patients who had unsatisfactory objective results also had obvious symptoms of post-traumatic stress disorder (PTSD) syndrome. These patients suffered from a direct impact on their social and professional performances, characterized by high rates of marital separation, depression and unemployment.
DISCUSSION
The emergency management of traumatic injuries of the pelvic ring is one of the most difficult situations for the Trauma Team on duty [11]. The adoption of coordinated resuscitation measures between a multidisciplinary team that is properly trained is of major importance for being able to gradually and effectively reduce the morbidity and mortality rate in this population.
In this sense, one of the most important points is the adoption of stratification scores that correctly assess the severity of the patient with an open fracture of the pelvic ring. Several classifications have been proposed [5, 7, 8, 12]. In this study, we evaluated two different systems often used in the literature: Jones classification evaluates the mechanical instability of the injury and its potential for contamination, and Faringer classification evaluates the need for faecal diversion according to the location of fracture exposition.
In the present study, it was observed that Jones classification showed statistical significance with respect to objective evaluations and emotional profile of the 18 surviving patients. As mentioned before, the more severe the skeletal injuries, the worse are the final results. Our patients had a high number of perineal exposure (class I) and the occurrence of chronic fistula, sexual (erectile) dysfunction, and painful intercourse was directly related to an unsatisfactory outcome.
In fact, sexual complaints, which occur in approximately 30% of patients after pelvic trauma, are closely related both to urogenital injuries, mainly from the prostatic urethra, and to a lesser extent to perineal injuries [13, 14]. Intercourse pain and erectile dysfunction are major problems among this population and are mainly attributed to both neurogenic etiology and pelvic floor dysfunction [13-15]. Baessler et al. observed that women who sustained an injury to the bladder developed coital incontinence during penetration and urinary urge incontinence, and women that sustained an injury to the perineum complained of incomplete bowel emptying, faecal urge incontinence and irritable bowel syndrome [15]. Severe damage to the lumbosacral plexus may occur either by trauma or during surgery, with incidence ranging from 1% to 30% in literature [16, 17]. Another major cause for the sexual dysfunction is the PTSD syndrome behavior, which is greatly related to the presence of scar tissue, cosmetic complaints, and skeletal pelvic asymmetry [3].
The Faringer classification showed no statistically significant relationship with the final objective but to the subjective result. We believe that the presence of a colostomy, even when reversed, was decisive for this observation. Although not found in our study, Hanson et al. demonstrated that there is a direct relationship between sepsis and colostomy in patients with very high ISS [6]. Contrarily, Woods et al. observed that faecal diversion was not associated with a lower incidence of abdominopelvic infectious complications [18]. Corroborating the observations from Woods et al., we found no association between the area of bone exposure and the EuroQol EQ-5D questionnaire.
The mortality rate in our series of open pelvic fractures was 40%, which is considerably higher than observed in other series [6, 19-22]. We believe this can be attributed to the high number of associated injuries, especially head and thoracic lesions, as all patients that died had an ISS greater than 35. Of the 12 patients that died, nine occurred during hospital admission, five during resuscitation and four during the first 24 hours. Factors that correlate with mortality are increasing age, the overall ISS, pelvic instability, size and contamination of the open wound, rectal injury, faecal diversion, and the number of blood units infused [2, 6]. In our study, it was observed that only the Jones classification showed a statistically significant relationship with mortality. We believe this observation is due to its combined assessment of the mechanical stability and the contamination degree.
LIMITATIONS
There are some limitations in our study. The principal limitation is its retrospective design based on patient’s chart review, although there were clear exclusion criteria for data collection. We were very rigorous to exclude all patients with incomplete medical records. Other potential limitation is the small number of patients, mainly when interpreted as two groups, the dead and the survivor patients. Clearly the small sample size could have distorted the statistical conclusions. However, even with a small case series, we were able to find that Jones classifications showed a statistically significant relationship both with mortality and evaluation outcome among survivors. These findings were supported by Cannada et al., who found that an unstable pelvic fracture using the Jones Classification seems to be an independent predictor of mortality in open pelvic fractures [23]. In addition, open pelvic fractures are rare, accounting for only 2% to 4% of all pelvic fractures, and to the best of our knowledge, there are no large series in the literature. Nevertheless, further studies with larger sample sizes are needed for validating our findings, showing the role of the Jones et al. classification in the acute scenario of the initial assessment and management of patients with open pelvic fractures.
CONCLUSION
We suggest the routine use of the Jones classification for the emergency room assessment and management of all open fractures of the pelvic ring. We believe the Faringer classification seems to be useful for the abdominal surgeons for the indication of gut transit derivation but not for the acute management of the bony component of an open pelvic fracture.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


