All published articles of this journal are available on ScienceDirect.
Is Casting for Non-Displaced Simple Scaphoid Waist Fracture Effective? A CT Based Assessment of Union
Abstract
Objective:
The purpose of this study is to report the union rate and time to union for acute non-displaced scaphoid waist fractures treated with a short arm thumb spica cast.
Methods:
A database was searched (2006-2013) to identify acute undisplaced scaphoid waist fractures. Cases that were not given a trial of casting were excluded (n=33). X-rays, CT scans and health records for each patient were reviewed to extract data.
Results:
172 patients met inclusion criteria. There were 138 males, 34 females, the mean age was 30 ± 16 years. The union rate was 99.4% (1 nonunion/172 subjects). The mean time to union was approximately 7.5 weeks (53 ± 37 days). Energy of injury, age or gender did not affect union rates or time to union. Cysts did not affect the union rate (p=0.73) but patients with cystic resorption along the fracture line required approximately 10 weeks for union (69 ± 60 days) compared to 7 weeks (51 ± 34 days) for those without cysts (p=0.05). Diabetes did not affect the union rate (p=0.81) but was found to increase the risk of delayed union (p=0.05). There was a weak, but statistically significant correlation between the number of days before the fracture was casted and the length of time needed to achieve union (r=0.27, p=0.001).
Conclusion:
Non-displaced scaphoid waist fractures have a high healing rate with appropriate identification and immobilization. Follow-up CT scans to assess healing can identify union within a shorter time frame (~7 weeks) than previously reported in the literature.
INTRODUCTION
The approach to the treatment of undisplaced scaphoid waist fractures varies widely. Some advocate early surgical fixation for undisplaced scaphoid waist fractures citing higher union rates and a faster time to union [1, 2] while others adopt a conservative approach, treating the majority of patients non-operatively, reserving open reduction with internal fixation (ORIF) for those who fail a trial of cast immobilization [3]. In instances where casts are used, the typical recommendation is for immobilization between 9-12 weeks [4, 5] with some advocating the use of a long arm thumb spica cast (LATSC) for 4-6 weeks followed by a short arm thumb spica cast (SATSC) for an additional 6-8 weeks [6, 7]. Because casting protocols can limit function and contribute to patient discomfort, avoidance of a lengthy period of casting often serves as the rationale for offering ORIF, even in cases with no fracture displacement.
Another reason many avoid cast treatment is the length of time needed to achieve union. Traditionally, the literature reports that the average time needed to heal a non-displaced scaphoid waist fracture with casting is 9 to 12 weeks [6, 8-12]. However, this data is based on radiographs, which have proven to be unreliable in documenting union [5, 13]. Imaging advances have allowed us to more accurately determine union than was previously possible with x-rays alone [13-16]. Geoghegan recently used computerized tomography (CT) to demonstrate that an undisplaced scaphoid waist fracture can heal after as little as 4 weeks of immobilization [17]. CT also allows a more detailed assessment of the fracture, allowing the surgeon to identify features that can contribute to an increased risk of non-union or delayed union [18].
The purpose of this study was to report the union rate and time to union for acute scaphoid waist fractures treated with a short arm thumb spica cast after excluding previously identified, CT based, negative prognostic features (translation, humpback deformity, comminution and sclerosis) [18]. Additionally, we would determine if any negative prognostic factors could be identified to help determine which patients would do poorly with non-operative management.
MATERIALS AND METHODS
Approval to conduct this study was obtained from our institutional review board. An institutional radiology CT database was searched for all scaphoid CT scans conducted between Jan 2006 - Dec 2013 inclusive. All scaphoids were scanned using a CT scanning technique previously reported, using 0.625mm helical cuts through the long axis of the scaphoid [19]. With the arm held overhead, only essential cuts of the scaphoid were taken, minimizing radiation exposure to less than half of a typical chest x-ray [18]. Non-operative treatment consisted of a SATSC in all cases.
Each subject’s x-rays, CT scans, and health record was reviewed to determine the details of injury, treatment course and treatment outcome. At our center, baseline CT scans are obtained for all scaphoid fractures to assess displacement and the first follow-up scan is scheduled 6-8 weeks post injury. Once 50% union is achieved on CT, casting is discontinued. However, as this was a retrospective study, there was no formal treatment protocol and decisions were made at the discretion of the treating surgeon.
One of 2 observers (a senior orthopedic resident and hand surgery consultant) reviewed all CT scans and the method described by Singh was used to determine the percentage of scaphoid union [20]. If union was determined to be 50% or greater, we considered the fracture to be united and determined the time needed to achieve union [7].
The inclusion criteria for this study included all isolated acute scaphoid waist fractures presenting less than 6 weeks from initial injury. Fractures of the scaphoid distal pole and proximal pole were excluded. This resulted in 367 cases for which the CT scans were reviewed. We then evaluated the initial CT scan and excluded cases if they were found to have any radiographic features associated with non-union or delayed union [18]. These negative prognostic factors included any displacement (translation and/or humpback deformity), comminution and/or sclerosis [18].
We excluded 211 cases based on one or more of the following reasons: translation of the fracture fragments (n=120), humpback deformity (n=43), sclerosis (n=13), comminution (n=72), perilunate injury (n=14) and loss to follow-up (n=6). There were 33 cases that were not given a trial of non-operative treatment and were initially treated surgically. This decision was made by the treating surgeon and was usually due to the degree of fracture displacement, however there were 8 cases in which the fractures were undisplaced. In each of these 8 cases there was an associated upper extremity injury [bilateral scaphoid fractures (n=1), ipsilateral distal radius fracture requiring surgery (n=4), proximal humerus fracture (n=1), radial head fracture (n=1)]. An additional 10 patients were excluded because they did not have CT follow-up confirming union; however the treating surgeon felt the fracture had united both clinically and based on x-ray in every case. This left 172 subjects for inclusion in the study.
In the study cohort, we determined the union rate, time to union and incidence of delayed union for scaphoid waist fractures with no displacement (translation or angular deformity), comminution, or sclerosis (further termed ‘simple’ scaphoid waist fractures). We evaluated patient factors and radiographic factors to determine if additional factors predictive of union, time to union or delayed union could be identified. Continuous variables were assessed with Students t-test, ANOVA and Pearson correlations where appropriate. Categorical variables were assessed with the Chi-square test (or Fishers exact test where appropriate).
RESULTS
This cohort consisted of 172 patients with isolated ‘simple’ undisplaced scaphoid waist fractures. There were 138 males (81.4%) and 34 females (18.6%) with a mean age of 30.5±16.2 years (11-85 years). There were 39 smokers (22.7%), 82 non-smokers (47.7%) and 51 subjects in whom smoking status was unknown (29.7%). Nine patients had a history of diabetes. Sixty-seven (40.1%) subjects injured their non-dominant extremity, 54 injured their dominant extremity (31.4%) and hand dominance was not documented in 46 subjects (26.7%). The energy of the injury was considered low in 67 subjects (i.e. fall from standing height), moderate in 58 (i.e. fall from a slight elevation e.g. stool or bicycle) and high in 28 (i.e. high speed mva/fall from height). Energy of injury was not documented in 19 subjects. The length of time between injury and casting was 3.5±7.7 days (range 0-40 days). Each subject received on average, 2 CT scans (mean 2.1±1.0 scans) throughout the course of their treatment. The mean time from the date of injury to confirmed union was 53±37 days (mean length of time in a cast was 49±36 days).
Union Rate
The union rate in this group was 99.4% (171/172). We were unable to identify any other features associated with an increased risk of developing a non-union: age (p=0.28), gender (p=0.62), diabetes (p=0.81), cysts (p=0.73) or energy of injury (p=0.17). The one non-union seen in this cohort occurred in a patient who smoked 2 packs per day however because smoking data was incomplete, we could not study its role as a predictor. Of note, all 18 patients with cystic changes on CT united successfully.
Time to Union
The mean time to union in this cohort was 53±37 days (~7.5 weeks) (95%CI 47-59 days). Union times were found to be adversely affected in patients with diabetes and those with cystic changes evident on CT. Scaphoid fractures in diabetics (DM) took on average over 3 weeks longer to unite (DM: 77±53 days, non-DM: 52±36 days, p=0.04). Fractures with cysts (n=18) evident on initial scan took on average 69±60 days to unite compared with 51±34 days when cysts (n=153) were not present (p=0.05). When these additional negative prognostic factors were excluded (DM, cysts) the mean time to union was 49±32 days (~7 weeks) (95%CI 45-55 days). The energy of injury was not significantly related to time needed for union (high 59 days, moderate 49 days, low 55 days, unknown 54 days, p=0.69). Age was not correlated to union time (pearson r= -0.013, p=0.864). There was a weak, but statistically significant positive correlation (r=0.264) between the number of days between injury and casting and the length of time needed to achieve union (p<0.001). The effect a treatment delay on union time is demonstrated in Fig. (1).

Delayed Union
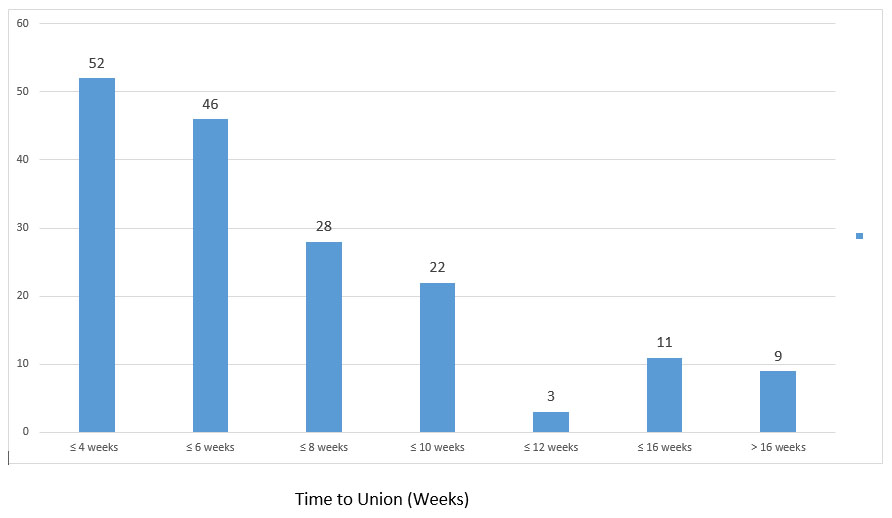
The mean time to union in this cohort was approximately 7.5 weeks (53 days). In total, 98 patients healed in ≤6 weeks (57%) and there were only 20 patients who took >12 weeks to heal (11.7%) (Fig. 2). The only factors linked to a higher incidence of delayed union were the presence of cysts, diabetes (Table 1), and a delay to receiving treatment (Fig. 2). Other predictive factors were not found to be associated with delayed union: age (p=0.47), sex (p=0.79), or energy of injury (p=0.82). If all factors shown to contribute to delayed union were excluded (cysts, DM, treatment delay: chosen to be a delay of >2 weeks based on clinical judgment), the mean union time was 48±30 days, or approximately 7 weeks (n=136) and less than 6% of cases took longer than 3 months to heal (8/136).
| Union < 3months | Union > 3months | p-value | ||
|---|---|---|---|---|
| Diabetes | yes | 6 | 3 | 0.05 |
| no | 147 | 15 | ||
| Cysts | yes | 12 | 6 | 0.005 |
| no | 140 | 12 | ||
| Treatment delay >2 weeks | Yes | 10 | 5 | 0.003 |
| No | 143 | 13 | ||
DISCUSSION
This study suggests that a high rate of union can be achieved with a reasonable period of immobilization in SATSC in a subset of patients with less severe or uncomplicated injuries. Some surgeons recommend ORIF over casting believing that casting is cumbersome for patients and that ORIF leads to a faster, more predictable union rate. While treatment must individualized to the patient’s injury, comorbid health status, and treatment preferences, this study provides information that can be useful to patients and surgeons making those choices. We feel that the added visualization of CT over plain radiography enables the surgeon to properly select which fractures are appropriate for non-operative cast treatment with an expected high degree of union. Our union rate of 99.4% compares favorably with the level 1 literature on scaphoid fractures [1-3, 21-23] (Table 2).
Prospective studies evaluating union in undisplaced scaphoid waist fractures, treated both surgically and with casting, revealed union rates between 77.3-100% (Table 2), however these studies did not evaluate their fractures with CT at baseline. As CT has been proven to be better able to diagnose factors such as displacement [5, 24], relying on x-ray alone can result in an under-appreciation of the degree of displacement. By accurately ruling out displacement with the use of CT at baseline, we were able to eliminate fractures which may have appeared undisplaced on x-ray but were actually minimally displaced. Since it has been shown that as little as >1mm displacement can adversely affect union rates [18], this may in part account for the varied union rates demonstrated in the literature. In addition, by using CT to define union, we were likely more able to confidently discontinue immobilization [13, 16, 25]. Another reason many do not favor a recommendation of cast treatment is that it is felt union takes much longer than with an ORIF; however there is little evidence to support this claim. The highest quality literature reviewing union times for scaphoid waist fractures can be extracted from three prospective RCT’s in the literature (Table 2) [1, 2, 21]. The union times in these studies have been reported to be anywhere between 10-24 weeks with casting and between 7-16 weeks with ORIF [1, 2, 21]. These studies rely on x-ray for defining union and because x-ray has been shown to be unreliable in determining union, this data may not be an accurate representation of union times [13].
| Author | Treatment type | Sample size | Union rate | Union time |
|---|---|---|---|---|
| CASTING ARM | ||||
| Bond [1] | LATSC x 6 weeks + SATSC until united |
14 | 100% | 12 weeks |
| McQueen [2] | Colles’ cast | 30 | 86.7% | 14 weeks |
| Dias [3] | Colles’ cast | 44 | 77.3% | |
| Adolfsson [21] | Below elbow | 26 | 100% | 10-24 weeks |
| Vinnars [22] | SATSC | 26 | 96.2% | |
| Saeden [23] | SATSC | 30 | 93.3% | |
| SURGICAL ARM | ||||
| Bond [1] | Percutaneous w Acutrak | 11 | 100% | 7 weeks |
| McQueen [2] | Percutaneous w Acutrak | 30 | 96.7% | 9 weeks |
| Dias [3] | ORIF (Herbert) | 44 | 100% | |
| Adolfsson [21] | Percutaneous w Acutrak | 23 | 95.7% | 10-16 weeks |
| Vinnars [22] | ORIF (Herbert) | 26 | 100% | |
| Saeden [23] | ORIF (Herbert) | 30 | 96.7% | |
In our study, union was assessed with CT and found to be approximately 7.5 weeks, with the majority of fractures healed in less than 6 weeks (57%). This is much shorter than the mean union times that can be extracted from the prospective RCT’s in the literature for both casting and ORIF (Table 2). Since union time data tends to be skewed, sample size, methods for defining union and handling of outliers all contribute to variations between studies on union times.
Delayed union is another concern when treating scaphoid fractures non-operatively. Although the definition of delayed union is controversial [26], the expected time for union of a scaphoid fracture is typically reported between 9-12 weeks [6, 8, 12]. In our study, only 11% took longer than 12 weeks to heal. We found that delayed unions (>3months/12 weeks) were more likely to occur in diabetics, those with evidence of cystic change on baseline CT or those who had a delay in receiving their cast treatment. Langhoff previously reported that a treatment delay under 4 weeks did not affect union rates or time to union, but we have demonstrated that a delay of as little as one week can be associated with a longer time needed to achieve union (Fig. 1) [27].
Another reason many do not support casting as an acceptable form of treatment is related to the cumbersome nature of casts, particularly the LATSC. In general it can be assumed that the more restrictive the cast, the less tolerable it is for patients. Over the years, there has been a varied approach to the type of cast recommended for the treatment of scaphoid fractures. The recommendations vary between a simple Colles’ cast, a SATSC and a LATSC. The type of immobilization used in the conservative arm for the RCT’s included in Table 2 vary between the use of all three. At our center, the protocol has been to use a SATSC. We have been satisfied with our clinical outcomes and have had good patient compliance.
Because we had no comparative group we cannot determine whether union rates or times would have been different if a LATSC was used, but in our anecdotal experience LATSC are poorly tolerated by patients. This study provides support for the use of SATSC with predictable union rates and times, offering an alternative for patients who would not tolerate a LATSC. The lack of a comparative operative arm is an additional limitation in this study. However because all patients with undisplaced scaphoid fractures were treated in a uniform fashion, we do not feel there is an underlying selection bias in this study. It should be noted however that union times for operatively treated fractures, similarly studied with CT, have not been established.
The retrospective study design does lead to several limitations. Data extracted from the charts was incomplete thus limiting our ability to fully evaluate the effects of various predictors on outcome (i.e. smoking). In addition, with such a low event rate (1 non-union/172 cases) it is difficult to develop a predictive model based on the risk factors reviewed in this study. It does however add strength to the predictive ability of the initial CT assessment and the exclusion of factors such as displacement, humpback deformity, comminution and sclerosis.
In this study the union times are overestimated because the CT scans were not taken at standardized time intervals. By convention, union was not assessed before 6 weeks post fracture and the CT’s were ordered in accordance to clinic schedules, which in the majority of cases did not occur before 6 weeks. It is possible that if the scans were taken earlier, perhaps we could have identified an even shorter time needed for union. Geoghegan has demonstrated that when evaluating union on CT, it appears that union may even be sufficient at 4 weeks to allow discontinuation of casting [17]. If future studies make assessments of union before the traditional 6 week time frame, we may find that the fractures unite even faster than demonstrated in this study. Despite this limitation, our conservative estimates of union times still compare favorably to the existing literature [1, 2, 21].
Our selection of 50% to define union may be debatable, however Hackney et al. report that most surgeons discontinue immobilization when there is 50% union [7]. Our selection of 50% is also based on work by Singh et al. who have reported that union >25% is sufficient to allow a return to all activity other than contact sports and that all patients in their study with union >25% at the time immobilization was discontinued proceeded to achieve full union [20]. Singh et al. did not advise return to contact sports or heavy physical labor if union was <50%. Based on these studies [7, 20] we felt that using 50% as a minimum criteria for union was appropriate, however this is an area that still requires further investigation.
CONCLUSION
This study was able to demonstrate that CT was able to define a subset of undisplaced scaphoid waist fractures that were able to almost uniformly achieve union using a short arm thumb spica cast in approximately 7 weeks. Additionally, it was determined that the likelihood of delayed union was increased in the presence of diabetes, cystic changes adjacent to the fracture and a treatment delay.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


