RESEARCH ARTICLE
Modified Weaver-Dunn Procedure Versus The Use of Semitendinosus Autogenous Tendon Graft for Acromioclavicular Joint Reconstruction
Galal Hegazy*, Hesham Safwat, Mahmoud Seddik, Ehab A. Al-shal, Ibrahim El-Sebaey, Mohamed Negm
Article Information
Identifiers and Pagination:
Year: 2016Volume: 10
First Page: 166
Last Page: 178
Publisher ID: TOORTHJ-10-166
DOI: 10.2174/1874325001610010166
Article History:
Received Date: 12/11/2015Revision Received Date: 9/3/2016
Acceptance Date: 25/4/2016
Electronic publication date: 31/05/2016
Collection year: 2016

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution-Non-Commercial 4.0 International Public License (CC BY-NC 4.0) (https://creativecommons.org/licenses/by-nc/4.0/legalcode), which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Background:
The optimal operative method for acromioclavicular joint reconstruction remains controversial. The modified Weaver-Dunn method is one of the most popular methods. Anatomic reconstruction of coracoclavicular ligaments with autogenous tendon grafts, widely used in treating chronic acromioclavicular joint instability, reportedly diminishes pain, eliminates sequelae, and improves function as well as strength.
Objective:
To compare clinical and radiologic outcomes between a modified Weaver-Dunn procedure and an anatomic coracoclavicular ligaments reconstruction technique using autogenous semitendinosus tendon graft.
Methods:
Twenty patients (mean age, 39 years) with painful, chronic Rockwood type III acromioclavicular joint dislocations were subjected to surgical reconstruction. In ten patients, a modified Weaver-Dunn procedure was performed, in the other ten patients; autogenous semitendinosus tendon graft was used. The mean time between injury and the index procedure was 18 month (range from 9 – 28). Clinical evaluation was performed using the Oxford Shoulder Score and Nottingham Clavicle Score after a mean follow-up time of 27.8 months. Preoperative and postoperative radiographs were compared.
Results:
In the Weaver-Dunn group the Oxford Shoulder Score improved from 25±4 to 40±2 points. While the Nottingham Clavicle Score increased from 48±7 to 84±11. In semitendinosus tendon graft group, the Oxford Shoulder Score improved from 25±3 points to 50±2 points and the Nottingham Clavicle Score from 48±8 points to 95±8, respectively.
Conclusion:
Acromioclavicular joint reconstruction using the semitendinosus tendon graft achieved better Oxford Shoulder Score and Nottingham Clavicle Score compared to the modified Weaver-Dunn procedure.
INTRODUCTION
Acromioclavicular (AC) joint injuries are among the most common injuries encountered by practicing orthopedic
surgeons. AC joint injuries can account for up to 12% of shoulder injuries [1, 2]. These injuries typically occur in the particular demographic of males, 30 year of age or younger, and during contact sports [3]. Tossy et al. [4] in 1963 originally described AC joint injuries as types I, II and III and Rockwood et al. [1] in 1990 further refined the classification to include types IV, V and VI. The spectrum of injuries can range from simple sprains with minimal sequelae to severe dislocations with fascial tears, AC joint or coracoclavicular (CC) ligament ruptures, resulting in major and debilitating shoulder dysfunction [5]. While nonoperative treatment recommended for type I and II injuries, and operative treatment seems to be the accepted option for type IV and VI injuries, there remains some controversy on the management of acute type III injuries [6]. Beitzel et al. [7] in 2013 reviewed the literature and over 150 different techniques for AC joint reduction and fixation. The optimal technique should have five components: anatomic reduction of the AC joint, repair or reconstruction of the CC ligaments, protection of the repair or reconstruction during the healing process, repair of any deltoid or trapezial fascial injury, and distal clavicular excision in patients with evidence of AC joint osteoarthritis [8]. Classically, the Weaver-Dunn [9] (WD), modified Dewar [10], Cadenat [11], and Bosworth [12] procedures have been used all with varying results. Each of these procedures provides different approach to fixation and/or reconstruction of the AC joint and the CC ligaments. Of these, The WD procedure involved excision of the distal end of the clavicle and transferring of coracoacromial (CA) ligament to the distal end of the clavicle, using the ligament as a substitute for the ruptured CC ligament [9]. This and other nonanatomic procedures have somewhat fallen out of favor because of poorer results in long term follow-up studies [13]. The WD procedure has been studied extensively, demonstrating up to a 30% failure rate and only approximately 25% biomechanical strength when compared to intact CC ligaments [14, 15]. Many publications exist which describe modifications to original WD procedure [16-23]. The Modified WD method involved excision of the distal end of the clavicle and transferring of the CA ligament to the distal end of the clavicle, using the ligament as a substitute for the ruptured CC ligament with augmentation of the transposed CA ligament by either cerclage wires, [24] screw fixation, [12] autogenous fascia lata graft, [25] or synthetics such as GORE-TEX, [26] Dacron, [27] carbon fibers, [28] and braided polyester [29]. Recently the modified WD procedure was compared with synthetic ligament and Graft Ropet (Arthrex, Naples, FL) reconstruction in both clinical and biomechanical studies revealing inferior results [30, 31]. It seems that while most nonanatomic techniques were able to restore vertical stability at the AC joint they still were significantly lacking in anteroposterior anatomic reconstruction of the CC ligaments [8]. In recent years, biomechanical studies focusing on an anatomic reconstruction of the CC ligament complex using tendon grafts have been reported. The structural properties of the normal CC ligament complex were tested and compared to various reconstructive techniques [32-35]. Costic et al. [36] 2004 compared the structural properties of the semitendinosus tendon (ST) graft as an anatomic reconstruction to the intact CC ligament complex. The authors concluded that with this graft, the course of the ligaments can be imitated, providing stability to the clavicle that is very close to that provided by the intact ligaments, with the added advantage of autogenous tissue. From a biomechanical point of view, an anatomic reconstruction using a free tendon graft and imitating the 2-bundle course of the CC ligament complex provides improved stability as compared with AC joint stabilization using a WD procedure [14, 37]. The anatomic CC reconstruction was shown to confer significantly less anterior and posterior translation than the modified WD procedure, which revealed greater laxity in comparison with the intact state. The authors suggested that with this anatomic reconstruction technique, recurrent subluxation and dislocation can be eliminated, decreasing the incidence of postoperative pain secondary to residual anterior-posterior instability and compromised clinical outcomes that have been observed with the modified WD procedure [14]. The purpose of this prospective clinical study is to make a comparison of clinical and radiologic outcomes between a modified WD procedure and an anatomic CC reconstruction technique using autogenous ST graft.
MATERIALS AND METHODS
Patients
Twenty patients (17 male and three females) with an average age 39 years (range from 21 to 60) underwent surgical reconstruction of painful, chronic complete AC joint dislocation. Indications for surgical treatment and thus inclusion criteria for this study were (1) failed primary nonoperative treatment of complete AC joint dislocation according to the classification of Rockwood type III (2) persistent disability and impairment for at least six months after primary treatment; and (3) written consent of patient without any general contraindication against surgery. Patients with cervical spine disorders, rheumatoid arthritis, or previous surgery of the shoulder joint were excluded from this study. The first ten patients were operated on using a modified WD procedure (WD group) and ten patients subsequently had autogenous ST graft for CC ligament reconstruction (ST group). Gender, age at the time of surgery, injury mechanism, affected side and hand dominance shown in Table 1. The mean time between injury and the index procedure was 18 month (range from 9 – 28). There were no statistically significant differences between the two groups regarding age, gender, primary treatment, level of activity, or time of follow-up.
Patient data.
| Gender | Age | Mechanism of Injury | Affected Side | Dominant Hand | Time from Injury to Surgery (months) | Reconstruction Procedure | Follow up (months) | |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 34 | RTA | LT | + | 21 | WD | 24 |
| 2 | M | 21 | RTA | RT | + | 14 | WD | 26 |
| 3 | M | 54 | RTA | RT | + | 28 | WD | 32 |
| 4 | M | 43 | FALL | RT | + | 18 | WD | 25 |
| 5 | F | 23 | RTA | LT | - | 24 | WD | 31 |
| 6 | M | 45 | RTA | RT | + | 19 | WD | 24 |
| 7 | M | 39 | FALL | RT | + | 9 | WD | 30 |
| 8 | M | 29 | RTA | LT | - | 14 | WD | 28 |
| 9 | M | 60 | FALL | LT | + | 9 | WD | 28 |
| 10 | M | 55 | FALL | RT | + | 26 | WD | 31 |
| 11 | M | 48 | FALL | RT | + | 21 | ST | 32 |
| 12 | F | 27 | RTA | RT | + | 27 | ST | 29 |
| 13 | M | 30 | RTA | RT | + | 15 | ST | 27 |
| 14 | M | 26 | RTA | RT | + | 10 | ST | 24 |
| 15 | M | 38 | RTA | LT | + | 12 | ST | 30 |
| 16 | M | 34 | RTA | RT | + | 19 | ST | 26 |
| 17 | M | 36 | RTA | RT | + | 13 | ST | 25 |
| 18 | F | 46 | RTA | RT | - | 17 | ST | 29 |
| 19 | M | 38 | RTA | RT | + | 23 | ST | 31 |
| 20 | M | 56 | FALL | LT | - | 25 | ST | 24 |
Surgical Technique of Modified WD Procedure
The surgical technique was the WD procedure as described in 1972 [9] and slightly modified by Shoji et al. [38] in 1986. The procedure was performed with the patient in the beach-chair position under general anesthesia (Fig. 1).
 |
Fig. (1). The beach-chair position. |
The AC joint with lateral end of the clavicle and the coracoid process were exposed after subperiosteal detachment of the deltotrapezial fascia using an anterior approach, which was a saber incision in line from the clavicle to the coracoid process (Fig. 2).
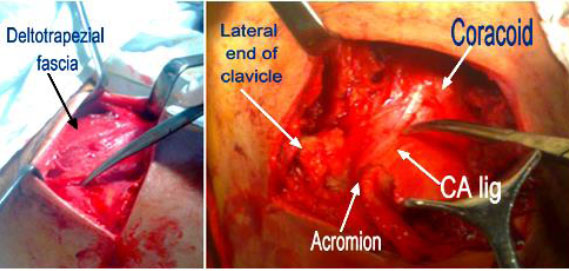 |
Fig. (2). Deltoid elevation, coracoid and coracoclavicular ligament exploration. |
The CA ligament was detached from the undersurface of the acromion with a small piece of bone. Resection of 10 mm of the lateral end of the clavicle was measured by a ruler just lateral to the attachment site of the trapezoid component of CC ligament (Fig. 3).
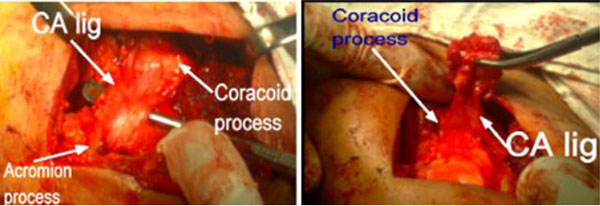 |
Fig. (3). CA ligament dissection and separation from its acromial insertion using Gigli saw. |
The AC joint reduced manually through upward displacement of the scapulohumeral complex by an assistant and a large point-of-reduction forceps placed on the coracoid and clavicle in order to aid in and ensure proper reduction of the AC joint (with great care to avoid medial displacement of the reduction forceps to protect the musculocutalleous nerve). The reduction maintained by a CC non-absorbable polyprolene braided suture sling passed under the coracoid process using a curved suture passer placed from medial to lateral under the coracoid to retrieve the suture and pull it around the coracoid. The sutures then passed through two drill holes (one for each end of the suture) in the clavicle and tied over it. Also the polyprolene sutures protect the CA ligament from detachment or dislodgment during the healing period (Fig. 4). The medullary canal of the lateral clavicle was prepared with a bur, allowing the bony end of the CA ligament to be inserted into the canal. This was performed by means of sutures placed through drill holes 5 mm medially from the end of the clavicle. To control correct reduction of the AC joint, we routinely used an image intensifier during surgery. Only after anatomic AC joint reduction was the graft sutured and fixed.
 |
Fig. (4). Rapping of polyprolene suture around the coracoid and passing through two holes in the clavicle. |
Surgical Technique of ST Graft
The Setup and surgical approach were identical to the WD group. In addition, the knee of the same side was draped and prepared for harvesting the ST tendon. Tendon harvesting was performed before AC joint exposure through a vertical incision (5 cm) over the pes anserinus area opposite the tibial tubercle, midway between the tubercle and the posterior edge of the tibia, the ST tendon was identified and harvested by a tendon stripper then the wound was closed in layers. The free ends of ST tendon sutured with No.2 Fiberwire sutures in a Krakow fashion. The AC joint and distal clavicle was exposed by detaching the origin of the deltoid muscle and the insertion of the trapezius muscle. The coracoid process was exposed by excising the scar tissue, remnants of CC ligaments and fat pad in the region of the CC ligaments. Aggressive medial dissection around the coracoid process avoided to protect the musculocutaneous nerve. There were three patients with a visible osteoarthritis existed in the AC joint, so a 10 mm of the distal clavicle was resected with an oscillating saw. At the insertion sites of the CC ligaments in the clavicle were drilled conoid and trapezoid tunnels. Conoid tunnel created approximately 45 mm medial to distal clavicle (35 mm if 10 mm of distal clavicle has been excised). The footprint of the conoid is posterior on the clavicle, thus the bone tunnel placed as posterior as possible. A cannulated reamer guide pin is placed at a 45 degrees posterior-to-anterior oblique angle. A bone tunnel is created with the appropriately sized reamer (5.5 or 6 mm depending on graft thickness). Trapezoid tunnel created approximately 30 mm medial to the distal clavicle (20 mm if 10 mm of the distal clavicle has been resected). The footprint of the trapezoid is more anterior than that of the conoid, thus the bone tunnel placed in the center of the clavicle. A cannulated reamer guide pin is placed prior to reaming. The bone tunnel is reamed with the appropriately sized reamer (5.5 or 6 mm depending on graft thickness) (Fig. 5).
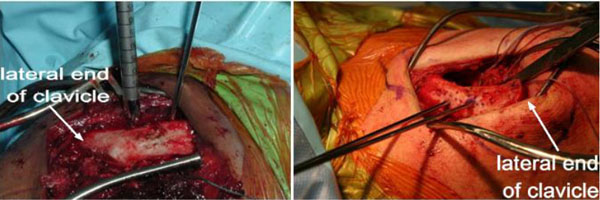 |
Fig. (5). Tunneling of the clavicle. |
The prepared tendon looped under the coracoid process from lateral to medial using a curved suture passer placed medial to lateral under the coracoid to retrieve the suture in the ST tendon graft and pull it around the coracoid (Fig. 6).
 |
Fig. (6). Tunneling of the clavicle. |
After the AC joint was reduced manually by the same technique as WD group, one limb of the graft passed through the conoid tunnel to re-create the conoid ligament. As the grafts passed, a guide wire inserted through the tunnel as well, and is fed through the cannulated process of the screw and driver. A 5.5 x 8 mm PEEK interference screw placed into conoid tunnel after ensuring tightness of the graft in the tunnel. Then other limb of the graft passed through the trapezoid tunnel to re-create the trapezoid ligament. The second screw is placed into the bone tunnel after the guide wire had been passed through the screw and driver. The free end of the ST tendon directed laterally to the medial aspect of the acromion to augment the AC ligaments with the remaining part of the tendon graft in seven patients who the lateral end of the clavicle was intact without bone resection. The free graft end attached laterally to the medial end of the acromion through drill holes using polyprolene sutures to strengthen the superior AC ligament. Finally, the deltotrapezial fascia is repaired securely with interrupted non-absorbable sutures and the subcutaneous tissue and skin were closed in layers. The postoperative management did not differ between surgical techniques. The shoulder was immobilized in a sling for four weeks. After this time, range of motion was restricted to 90° for another eight weeks. Free range of motion was allowed three months after surgery. Radiologic controls were performed in four weeks intervals. A single observer reviewed all 20 patients, both clinically and radiographically. The mean follow-up time was 27.8 months (range from 24 to 32 months). Preoperative and post-operative clinical assessment consisted of a structured interview, a detailed physical examination, and evaluation using Oxford Shoulder Score [41] and Nottingham Clavicle Score [42]. Active abduction, flexion, and external rotation were measured in degrees. Internal rotation was graded according to the posterior spinal level the thumb was able to reach. Finally, patients were asked their overall satisfaction with the postoperative result on a visual analog scale (VAS). We used the simplest VAS which is a straight horizontal line of fixed length (100 mm). The ends are defined as the extreme limits of the parameter to be measured (pain) orientated from the left (best) to the right (worst). Using a ruler, the score is determined by measuring the distance (mm) on the 10-cm line between the “no pain” anchor and the patient’s mark, providing a range of scores from 0–100. A higher score indicates greater pain intensity. According to the distribution of pain VAS scores, no pain (0–4 mm), mild pain (5-44 mm), moderate pain (45–74 mm), and severe pain (75–100 mm) (11). In addition, all patients from the ST group were asked at follow-up about complaints such as pain, weakness, or hyperesthesia in the donor knee. The radiologic examination consisted of anteroposterior AC joint and axillary shoulder radiographs for each shoulder, as well as bilateral stress radiographs with a 10-kg weight suspended from each arm with wrist straps [39, 40]. The degree of displacement of the AC joint was evaluated measuring the CC distance on the anteroposterior view for vertical displacement and assessing the horizontal displacement on the axillary view.
Statistical Analysis
The paired t test was used to determine if there was a significant difference between preoperative and postoperative Oxford Shoulder Score [41] and Nottingham Clavicle Score [42]. A 2-sample t test was used to determine if there was a significant difference between the WD and the ST groups. Results were confirmed using a 2-sample Wilcoxon rank sum test. A P value of less than .05 was considered statistically significant.
RESULTS
Clinical Outcome
In the WD group, the Oxford Shoulder Score improved from 25±4 points preoperatively to 42±2 points postoperatively. The Nottingham Clavicle Score increased from 48±7 points before surgery to 84±11 at follow-up. The visual analog scale improved from 48±10 mm to 10±3 mm. At follow-up, the average abduction was 174° ± 4°, flexion 171° ± 7°, and external rotation 56° ± 9°. In the ST group, the Oxford Shoulder Score improved from 25±3 points to 50±2 points and the Nottingham Clavicle Score from 48±8 points to 95±8, respectively. The visual analog scale improved from 49±3 to 4±2 mm. At follow-up, the average abduction was 178° ± 2°, flexion 179° ± 3°, and external rotation 66° ± 6°. Preoperative and postoperative differences in the Oxford Shoulder Score and the Nottingham Clavicle Score were statistically significant (P< .001) for both surgical techniques. Comparison between the WD and ST groups showed a significantly better outcome in terms of both outcome surveys and subjective satisfaction (P< .001), in favor of the ST group Table 2.
Pre-operative and post-operative clinical results.
| Patient No. | OSS Preop. | OSS Postop. | NCS Preop. | NCS Postop. | VAS Preop. mm | VAS Postop mm |
|---|---|---|---|---|---|---|
| 1 | 28 | 42 | 64 | 93 | 38 | 8 |
| 2 | 26 | 41 | 55 | 83 | 43 | 12 |
| 3 | 23 | 40 | 48 | 90 | 55 | 11 |
| 4 | 29 | 42 | 65 | 94 | 47 | 9 |
| 5 | 27 | 42 | 60 | 85 | 39 | 10 |
| 6 | 22 | 38 | 41 | 62 | 54 | 14 |
| 7 | 27 | 39 | 54 | 84 | 48 | 11 |
| 8 | 28 | 40 | 56 | 90 | 51 | 10 |
| 9 | 25 | 38 | 51 | 86 | 57 | 12 |
| 10 | 23 | 39 | 45 | 80 | 51 | 10 |
| 11 | 22 | 48 | 40 | 83 | 56 | 6 |
| 12 | 24 | 50 | 49 | 90 | 49 | 5 |
| 13 | 26 | 51 | 52 | 100 | 51 | 2 |
| 14 | 24 | 49 | 43 | 95 | 50 | 3 |
| 15 | 27 | 51 | 46 | 102 | 49 | 4 |
| 16 | 29 | 52 | 56 | 103 | 48 | 2 |
| 17 | 23 | 50 | 45 | 89 | 48 | 5 |
| 18 | 24 | 51 | 48 | 96 | 49 | 3 |
| 19 | 28 | 52 | 53 | 103 | 48 | 3 |
| 20 | 25 | 49 | 50 | 95 | 49 | 4 |
Radiologic Outcome
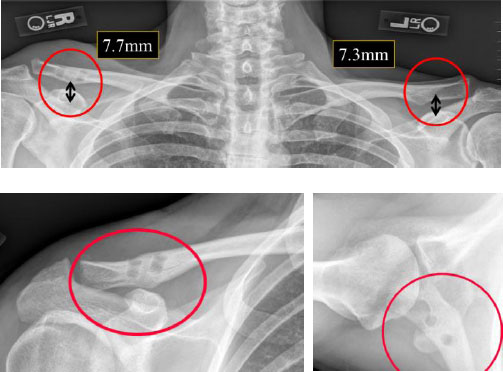
In the WD group, the mean CC distance was 13.3 ± 3 mm. With 10-kg–weight stress loading, this distance increased to 15.9 ± 4 mm, compared with 11.1 ± 2 mm on the non injured side (Figs. 7a and 7b). In the ST group, the mean CC distance was 11.7 ± 3 mm. In the stress view, a distance increase to 12.1 ± 3 mm was observed, compared with 10.8 ± 2 mm on the unaffected side (Figs. 8a and 8b). No statistically significant correlation was observed between the clinical scores and the CC distance (P> .05). A significant correlation existed between the clinical scores and the amount of the displacement under stress loading (P< .05). The more displacement that occurred under stress, the lower was the clinical score. When the postoperative CC distances between the WD and ST groups were compared, a statistically significant difference existed during stress loading, when compared with the uninjured side (P= .037).
Fig. (7) Preoperative and postoperative radiography for WD procedure.
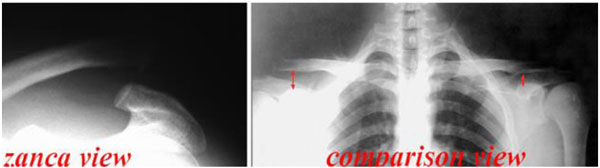 |
Fig. (7a). a) Pre-operative radiography of male patient 38 y old shows right ACJ dislocation with increased coracoclavicular distance in RT shoulder. |
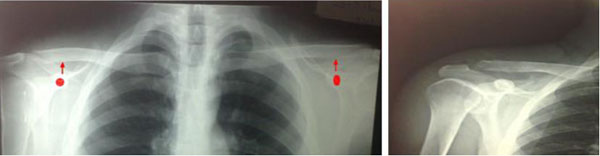 |
Fig. (7b). b) 4 weeks Post-operative radiographs show equal coracoclavicular distance and reduced ACJ after modified Weaver-Dunn procedure on right AC joint. |
Fig. (8) Preoperative and postoperative radiography for ST graft reconstruction.
Complications
Three patients in the WD group had failure within six months treated with ST tendon graft reconstruction. No failures were recorded in the semitendinosus tendon graft group. Superficial infection occurred in three patients in the WD group and four patients in the ST group; all were successfully treated with antibiotics. No serious complications in the donor knee could be observed, with only a mild hyperesthesia of the infrapatellar branch of the saphenous nerve in one patient.
DISCUSSION
The surgical treatment of symptomatic chronic dislocations of the AC joint included two main pathways [24]. In patients with incomplete injury, Rockwood types I and II, the usual procedure has been resection arthroplasty of the distal end of the clavicle, as described by Mumford [43]. In cases with complete AC joint dislocation, Rockwood types III through V, resulting in deficiency of the CC ligament complex, AC joint stabilization was performed, addressing the reconstruction of the CC ligaments. In this context, a widely used and frequently favored surgical technique was the transfer of the CA ligament from the acromion to the lateral end of the distal clavicle, which was used for the treatment of acute injuries as well, including its various technical modifications [37]. Excision of the distal clavicle with a coracoid based transfer of the CA ligament is a popular technique, but it has its drawbacks: a tendency to displace the clavicle anteriorly [27] and (often) recurrent deformity [44]. The CA ligament may be biomechanically insufficient in terms of strength and stiffness as a replacement for an injured CC ligament [45]. Deshmukh et al. [32] in 2004 showed that anteroposterior laxity of the AC joint was significantly (P< .01) greater after a WD reconstruction than in the native state, which may account for the high rate of loss of reduction after a CC reconstruction via a CA ligament transfer. Therefore, many have recommended augmentation procedures to protect the transferred CA ligament. Modifications of the WD procedure have achieved good outcome for acute and chronic AC joint dislocations [28-31]. A biomechanical studies concluded that the CA ligament has only 30% of the strength and 10% of the stiffness of the intact ligaments, and failures occur mainly at the suture that attaches the transferred CA ligament [35, 36]. The mean laxity after reconstruction was 42 mm in an anteroposterior plane and 14 mm vertically, compared with 8 mm and 3 mm, respectively, in intact ligaments. Tauber et al. [45] in 2009 concluded that the anatomic properties of the CA ligament result in an anterior and slightly inferior subluxation of the distal end of the clavicle when coracoacromial ligament transfer is performed. The entire weight of the upper extremity pulls at the distal end of the clavicle with an accordingly nonanatomic longer lever arm, whereas suspension of the coracoid to the clavicle in the anatomic reconstruction results in a shorter lever arm with less muscle fatigue at the shoulder girdle [45]. In 1976, Zaricznyj [46] reported using the extensor tendon of the fifth toe as a free tendon autograft. He reconstructed the AC joint and CC ligaments but did not reproduce the anatomical configuration of both limbs of the CC ligament; he augmented this repair with Kirschner wires across the AC joint. In 2001, Jones et al. [47] first described use of autogenous ST tendon as a free graft for reconstructing the CC ligament. They did not reconstruct the AC joint ligaments or attempt to restore the anatomical configuration of the trapezoid and conoid ligaments. They augmented their reconstruction with suture CC stabilization techniques. In 2003, Lee et al. [48] biomechanically compared the strength and stiffness of the native CC ligament with that of reconstructions with CA ligament or free tendon grafts (semitendinosus, gracilis, or long-toe extensor tendons). They reported that all tendon grafts had strengths equivalent to the native CC ligament strength, and all were significantly stronger (P< .05) than the CA ligament reconstruction [48]. Debski et al. [49] in 2001 showed that the trapezoid and conoid ligaments act separately to stabilize the AC joint and recommended that the conoid and trapezoid ligaments not be treated as a single structure during reconstruction. Other studies have suggested that all AC joint soft tissues function synergistically to provide AC joint stability and should participate in the healing process for maximum stability [35-37]. Biomechanical studies have shown that, compared with other constructs, the semitendinosus tendon has clinically insignificant (<3 mm) permanent elongation after cyclic loading, and a stiffness that more closely approximates the stiffness of the intact CC ligament [31-34, 37]. On the basis of the clinical and biomechanical success of this tendon in anatomical reconstructions [34, 35, 37]. Mazzocca and colleagues [14] used a ST autograft to reconstruct the anatomical configurations of the trapezoid and conoid ligaments, as well as the AC ligaments, without use of supplemental CC or AC stabilization. Compared with the previously described techniques, autogenous free graft reconstruction has numerous advantages. First, the ST tendon is easy to harvest [14] and biomechanically strong (favorable comparison with reported strength of intact CC ligament) [32, 34, 37]. Second, the strength of this graft obviates the need for augmentation with nonbiological devices [45]. Such devices are the source of many complications such as foreign body tissue reaction, need for hardware removal and lack the remodeling capacity of autologous grafts [45, 47]. Third, the strength of this graft also decreases the risk for premature failure, theoretically promoting earlier postoperative range of motion and rehabilitation, resulting in less shoulder stiffness, and facilitating earlier return to sports [48]. Fourth, the biological nature of these grafts allows healing and thereby increases the likelihood of long term stability. Fifth, there are no reports of long term functional morbidity from such graft harvest [45]. Sixth, these grafts are long enough to allow anatomical reconstruction that duplicates the origins and insertions of the trapezoid and conoid ligaments and that reinforces the ruptured AC ligaments [48]. In our comparative study the rate of complications was high in patients with modified WD procedures, there were three of ten patients had failure in the reconstruction within the first six months post-operative in contrast to ST group there was no patient had failure in the reconstruction.
CONCLUSION
The optimal operative method for treatment of chronic AC joint dislocation Rockwood types III remains controversial. The surgery was indicated in patients who failed non-operative treatment and had symptoms affecting activities of daily living. The modified WD method is one of the most popular methods in treating chronic AC joint dislocation, but it has its drawbacks and the CA ligament may be biomechanically insufficient in terms of strength and stiffness as a replacement for CC ligament. Using of ST graft for anatomical reconstruction of CC ligament in chronic AC joint dislocation, providing stability to the clavicle that is very close to that provided by the intact ligaments, with the added advantage of autogenous tissue. AC joint reconstruction using the semitendinosus tendon graft achieved better Oxford Shoulder Score and Nottingham Clavicle Score compared to the modified Weaver-Dunn procedure.
LIST OF ABBREVIATIONS
| AC | = Acromioclavicular |
| CA | = Coracoacromial |
| CC | = Coracoclavicular |
| Kg | = Kilogram |
| MHQ | = Michigan Hand Questionnaire |
| mm | = Millimeter |
| ST | = Semitendinosus Tendon |
| VAS | = Visual Analog Scale |
| WD | = Weaver-Dunn |
INSTITUTIONAL REVIEW BOARD STATEMENT
The study was reviewed and approved by the Faculty of Medicine – Al-Azhar University Institutional Review Board.
STATEMENT OF INFORMED CONSENT
All study participants provided informed written consent prior to study enrollment.
STATEMENT OF HUMAN RIGHTS
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declare none.