RESEARCH ARTICLE
Lengthening Over an Existing Intramedullary Nail In Cases of Post-traumatic Femoral Shortening. Technical Note. Case Series Study
Achilleas Boutsiadis*, Eirini Iosifidou, Xilouris Nikolaos, Ippokratis Hatzokos
Article Information
Identifiers and Pagination:
Year: 2016Volume: 10
First Page: 12
Last Page: 18
Publisher ID: TOORTHJ-10-12
DOI: 10.2174/1874325001610010012
Article History:
Received Date: 22/2/2015Revision Received Date: 21/8/2015
Acceptance Date: 26/8/2015
Electronic publication date: 17/3/2016
Collection year: 2016

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution-Non-Commercial 4.0 International Public License (CC BY-NC 4.0) (https://creativecommons.org/licenses/by-nc/4.0/legalcode), which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Background:
Intramedullary (IM) nailing is the method of choice for the treatment of most femoral shaft fractures. However, despite successful solid union, great initial fracture comminution can lead to significant leg length discrepancy affecting normal gait mechanics. Femoral osteotomy and distraction osteogenesis over the pre-existing IM nail could restore this limb inequality.
Methods:
Five patients with an average post-traumatic femoral shortening of 3.83 cm were presented in our department with the nail in situ. Limb lengthening was achieved with the application of a distal hybrid external rail frame over the pre-existing nail. We assumed that the choice of a distal external fixator ring with wires could facilitate the procedure and minimize the possibility of friction–contact problems with the large diameter nail.
Results:
The amount of length discrepancy, calculated preoperatively, was restored in all patients. The mean time in frame was 57.6 days and the external fixator index 16.978 d/cm. The mean time of total healing was 152.6 days and the average bone-healing index 44.9d/cm. No deep infection or hardware loosening was observed. One superficial pin track infection was treated successfully with oral antibiotics.
Conclusion:
This technique utilizes the principles and advantages of lengthening over an IM nail, avoids the necessity of nail removal and minimizes the complication rates and the overall time for complete recovery.
INTRODUCTION
Intramedullary (IM) nailing is the method of choice for the treatment of most femoral shaft fractures. In general, closed technique combined with reaming and interlocking screws has been associated with high union rates and small percentages of complications [1]. However, it is not always an easy procedure with predictable results [2]. Rotational or angular malunion and length leg discrepancy have been described in the international literature [3, 4]. Authors reported that despite solid union and excellent radiological results, initial fracture comminution could lead to significant residual length leg discrepancies in up to 43% of the cases [5, 6].
Shortening deformity can affect significantly the normal gait mechanics during daily living activities. Inevitable quadriceps weakness and asymmetric joint loading may lead to contralateral hip, knee and low back pain or even to limping gait [1-3]. Correction of this axial malunion can be challenging regarding intra-operative complications, post-operative stiffness,infections, muscles’ weakness or even patient’s compliance.
Limb lengthening was first described by Codivilla in 1905 [7] but the new era was introduced by Ilizarov who described the distraction osteogenesis method [8]. The innovative method of lengthening over an intramedullary nail was described by Palley et al., reducing the external fixator period and thus making the treatment more comfortable for the patient and also eliminating the complication of regenerated bone fracture after the fixator removal [9]. Purpose of this study is the presentation of the surgical technique and the prospective evaluation of the intra-operative difficulties and the results of femur lengthening over the pre-existing intramedullary nail using hybrid external fixator.
The scientific council of our general hospital has approved the project (Log No. 1794).
SURGICAL TECHNIQUE
Pre-operative planning involved accurate assessment of the Leg-Length Discrepancy (LLD) with assisted computed tomography scanogram (Fig. 1). Careful soft-tissue evaluation and laboratory blood tests (ESR, CRP) were also performed in order to exclude any possibility of infection.
The patients were positioned on a traction radiolucent table in order to facilitate anteroposterior and lateral x-ray views of the hip and knee joints and of the entire femur.
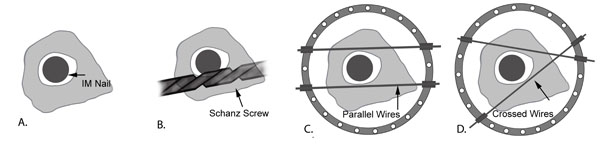
The distal locking screws of the pre-existing antergrade intramedullary nail (IMN) were firstly removed. Initially, three or four proximal external fixator hydroxyapatite-coated half-pins were placed at the level of the lesser trochanter, perpendicularly and posteriorly to the nail. Distally, an external fixator ring with four wires was applied at the metaphyseal region parallel to the knee joint in order to avoid the possibility of friction–contact problems with the large diameter nail (Figs. 1, 2).
Then the osteotomy site was decided depending on the site of the malunion, bone quality and position of the IMN. Adequate length of the intramedullary nail was left at the distal fragment of the osteotomy calculating its final position-migration after limb lengthening. The osteotomy was performed through a lateral 3cm skin incision, away from the fracture site. It was started using the multiple-drill-hole technique and finished carefully with an osteotome. Care was taken not to damage the IMN. Slight rotational manipulation of the distal fragment confirmed the disengagement of the bone canal from the nail and the osteotomy completion, in order to allow sliding of the nail.
Finally, a lengthening rail frame (LRS, Orthofix S.R.L., Bussolengo, Verona, Italy) was applied parallel to the IMN and the femur, connecting the proximal half-pins with the distal ring. Before the rail application and under fluoroscopy evaluation any rotational deformity was also corrected through the distal ring. In all cases distraction was started ten days post-operatively at a rate of 0.75mm/day, in increments of 0.25mm.
Isometric quadriceps and knee range-of-motion exercises were started immediately. Touch toe walking with two crutches was encouraged from the first post-operative day. The distraction of the osteotomy was confirmed with x-rays 10 days later. The lengthening progress was monitored by means of plain radiographs every three weeks.
After the achievement of the desired distraction all patients were brought to the operating theatre. Two distal interlocking screws were inserted with the freehand technique, under fluoroscopic guidance. The external fixator was removed and partial weight bearing of approximately 20kgs was allowed until new bone consolidation was confirmed (Fig. 1).
CASE SERIES
Five patients with post-traumatic femoral shortening, in which the initial fracture was managed with closed intramedullary nailing, were presented in our department with the nail in situ. Four patients were male and one female with an average age 28.3 years (range 21-38 years). Despite fracture healing, great initial comminution led to a mean leg length discrepancy of 3.83 cm (2.5- 4cm). Limb lengthening with application of a distal hybrid external rail frame (LRS, Orthofix S.R.L., Bussolengo, Verona, Italy) over the pre-existing nail, as described above, was decided in all cases.
The mean lengthening achieved was 3.84cm and the amount of the discrepancy, calculated preoperatively, was restored in all patients. The mean time in frame was 57.6 days (range 48-67 days) while the external fixator index was 16.978 d/cm (range 13.7 d/cm – 19.14 d/cm). The mean time of total healing was 152.6 days (range 138-175 days) and the average bone-healing index was 44.9d/cm (range 42.9-48.57d/cm).
No intraoperative or postoperative neurovascular complications occurred. No malrotation or other axial deformity was observed in any patient during final clinical and radiographic evaluation. Range of motion of the knee joint was normal and not affected by the treatment method. In one case 20° restricted hip flexion and abduction were not significantly improved after limb lengthening. According to Paley’s scoring system for outcome of femoral lengthening in all cases the outcome was excellent (Fig. 3) [9].
In one patient superficial pin track infection was treated successfully with oral antibiotics. No deep infection or hardware loosening was observed. In two cases slight over-lengthening (0.3-0.4cm) was observed during the last radiographic examination before external fixator removal. Using the hybrid rail frame, gradual shortening for a period of 1 week restored the desired length before the insertion of the nail’s interlocking screws.
 |
Fig. (3). Clinical views of the same patient six months post-operatively. Note the complete length restoration and the complete range of motion of the knee. |
DISCUSSION
Locked intramedullary nailing remains the preferred surgical technique for the treatment of femoral shaft fractures [2]. However, fractures with bony defects and high comminution can result in leg-length discrepancy that may affect gait mechanics, cause pain of the contralateral joints and even increase energy expenditure during walking [2]. Distraction osteogenesis over the pre-existing IM nail can restore this axial malunion and improve the clinical outcome with minimum complication rates [10]. The external fixator can be removed immediately after the distraction period, increasing patient’s tolerance. The preservation of the IM nail protects the hip abductors and possibly the femur’s head vascularity from a second violation. Additionally, the IM nail provides greater stability to the construct during the consolidation phase acting as an internal scaffold that maintains the alignment [10].
The classical technique of lengthening over a nail utilizes a unilateral fixator with 2 or 3 Schanz screws at each bone segment [10]. However, successful distraction and adequate sliding of the bone over the intramedullary nail necessitates parallel application of the external fixator to the nail in both axial and coronal planes. Otherwise minor malrotation or malposition of the screws may cause friction between the nail and the femur especially after the attachment of the fixator and initiation of the distraction sequence. Additionally, most reported complications during lengthening over nail are associated to the Schanz screws and include difficulties in inserting, cut outs, pin track infection, joint contracture and stiffness [11].
In order to avoid these possible complications we decided to apply a hybrid rail frame in all cases. Due to their smaller diameter (2mm), the insertion of the ring’s wires was easier and there was less possibility of an undesirable contact and friction with the nail, during the distraction. Additionally, due to the presence of the big diameter nail, the parallel application of the wires could also be performed without any concern that a possible ring shearing movement could affect the final result (Fig. 2) [12]. Also, it is of outmost importance to understand that the pre-existing nails are somehow “re-used” during this procedure because they have already been implanted for the initial fracture healing. We do not know their ultimate failure point due to fatigue and consequently our purpose was to avoid any inadvertent damage of them during the rail frame insertion. The application of the 2mm wires instead of the 6mm Schanz screws minimizes the risk of abrading the nail (Fig. 2). Additionally, great attention was given to the osteotomy procedure in order not to damage the shaft of the nail, which will withstand all the loading forces during the consolidation period. Finally, it has been reported that hybrid external fixator have shown lower rates of pin tract infection, observation that is very important in these post-traumatic re-operated cases [13].
Despite the small case series our results show low complications rate and similar external fixator and bone healing index compared with previous published studies (Table 1) [9, 10, 14-18]. However, this technique has only been used for correcting axial deformities. Angular (varus-valgus, apex anterior-apex posterior) or even translational (in frontal-in sagittal plane) deformities are more difficult to be corrected with lengthening over nail and it has not been described before in post-traumatic cases [11].
Summary of our study and previous published studies showing the results after femoral lengthening over an intramedullary nail.
| Post-Traumatic | Pre-existing Nail | Type of External Fixator | Time in frame | External Fixation Index | Bone Healing Index | Mean Length Achieved |
|
|---|---|---|---|---|---|---|---|
| Kim et al. (2011) | 5 cases | 5 cases | 5 Unilateral | 32.2 days | 0.46mo/cm | 1.71mo/cm | 2.58cm |
| Simpson et al. (1999) |
16 cases | 0 cases | 3 Ilizarov 13 Unilateral |
98 days | 0.65mo/cm | Not available | Not available |
| Song et al. (2005) | 16 cases | 0 cases | 16 Unilateral | 140 days | 0.8mo/cm | Not available | 5cm |
| Lin et al. (1996) | 4 cases | 0 cases | Ilizarov | 1 month after completion of distraction | Not available | 1.83mo/cm | 4cm |
| Mahboubian et al. (2012) | 15 cases | 0 cases | Unilateral | 48 days | 0.4mo/cm | 1.39mo/cm | 4cm |
| Paley et al. (1997) | 11 cases | 0 cases | Unilateral Ilizarov |
120±60 days | 0.7±0.4mo/cm | 1.4mo/cm | 5.8cm |
| Kucukkaya et al. (2013) | 7cases (Not explained Number of post-traumatic) |
0 cases | Unilateral (Retrograde Nail) |
48.1 days | 0.37mo/cm | 1.38mp/cm | 4.3cm |
| Our study | 5 cases | 5 cases | Hydrid External Fixator | 57.6 days | 0.56mo/cm | 1.49mo/cm | 3.84cm |
CONCLUSION
By lengthening over the pre-existing intramedullary nail, the duration of the external fixation was reduced, thus leading in increased patient’s comfort and decreased incidence of complications such as pin track infection and joint stiffness. Additionally, the presence of a large diameter intramedullary nail prevented fracture and deformation of the regenerated bone. The novelty of our study is the application of a distal ring with wires that facilitates the successful performance of the procedure and minimizes the possibility of friction–contact problems with the nail. Compared with the already published small case series, our excellent results suggest that it is a safe procedure that can be performed in any patient with post-traumatic axial deformity of the femur.
LIST OF ABBREVIATIONS
| CRP | = C-reactive protein |
| ESR | = Erythrocyte Sedimentation Rate |
| IM | = Intramedullary Nailling |
| IMN | = Intramedullary Nail |
| LLD | = Leg-Length Discrepancy |
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We would like to thank Mrs EC, Graphic Designer, for the design of the professional quality drawing.